Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: a cross-sectional study
Introduction
Hypertension is a major public health problem worldwide (1). It is the most common cause of cardiovascular morbidity and mortality with proven benefits of treatment. The presence of hypertension more than doubles the risk for coronary heart disease; including acute myocardial infarction and sudden death and more than triples the risk of congestive heart failure and strokes (2). The prevalence of hypertension in Sub-Saharan Africa has attained epidemic proportions likely due to the epidemiological transition with adoption of Western lifestyles. The estimated prevalence of hypertension among adults in SSA increased 4 folds from 2005 to 2008 and is projected to affect 125.5 million adults by 2025 (3). In Cameroon; two recent population based studies estimated the prevalence rate of hypertension between 30% and 47.5% (4,5).
Despite the availability of multiple effective antihypertensive medications with proven benefits in reducing cardiovascular morbidity and mortality, control of hypertension remains poor (6,7). In both high and low income countries, less than 27% and 10% respectively of hypertensive patients have achieved their target blood pressure (6,7). In a recent population based survey in Cameroon, only 24.6% of patients with hypertension on treatment had their blood pressure controlled (4). Improvement in the management and control of hypertension will require an understanding of the factors that affect blood pressure control. Unfortunately, the reasons for uncontrolled hypertension remain unclear in low income countries and have been insufficiently studied in Cameroon.
The main goal of this study is to determine the correlates of blood pressure control amongst patients with hypertension followed up in outpatient clinics in Yaoundé, the capital city of Cameroon. Understanding predictors of poor control can facilitate development of targeted strategies.
Methods
Study setting
This was a descriptive, cross-sectional study done at five outpatient hypertension units in hospitals in Yaoundé, the capital city of Cameroon with a catchment population of about 2 million individuals in 2012. The follow-up of patients at these centers was done by cardiologist, internists and general practitioners in dedicated hypertension units. Participants were 18 years and older, previously diagnosed with hypertension, and had been prescribed antihypertensive medications.
Definitions
Hypertension or diabetes were based on documented history, ongoing drug treatments, or a documented previous systolic (and/or diastolic) blood pressure ≥140 mmHg (90 mmHg) for hypertension or fasting blood glucose ≥126 mg/dL for diabetes. Dyslipidemia was based on documented history, ongoing drug treatment or documented total cholesterol ≥200 mg/dL, LDL cholesterol ≥100 mg/dL, and HDL-cholesterol ≤40 mg/dL for men or ≤50 mg/dL for women, and/or triglyceride ≥150 mg/dL. Alcohol consumption and status for smoking were recorded during patient interview.
Recruitment and data collection
Patients were identified on the basis of antihypertensive medication use and a diagnosis of hypertension. All consecutive patients aged 18 years and above who came for their scheduled follow up visit between May and September 2015 was recruited. After explaining the purpose of the study, we obtained informed consent from the participants. Baseline socio-demographic data including age, gender, place of residence, occupation, marital status, monthly income, level of education, health insurance and the antihypertensive medications were recorded. History of cardiovascular risk factors and co-morbidities including diabetes mellitus, smoking, hyperlipidemia, hyperuricemia, past history of stroke, heart failure, chronic kidney disease, cancer and alcohol consumption were obtained through interviews, complemented by data from the medical records. Height was measured with a calibrated stadiometer to the nearest 0.5 cm, weight in light clothes with a scale balanced to the nearest 0.5 kg. The height and the weight were used to obtain the body mass index expressed in kg/m2. The blood pressure on the day of clinic visit was measured after the patient had rested for at least 10 minutes, two blood pressure readings were measured and the average calculated using an OMRON 3 validated automated blood measuring device. Medication adherence was assessed using the Morisky Medication-taking Adherence Scale- MMAS-4 (8). Patients who scored ≥2 on MMAS-4 were considered to have good adherence. Types and number of anti-hypertensive medications was recorded. We also recorded information regarding lifestyle modifications or changes (diet rich in fruits, vegetables, low in fat and salt and physical activity). Questions were also asked on the duration of hypertension, medical personnel following up patient, frequency of follow-up visits, possession of a home blood pressure monitoring apparatus. We excluded patients with cognitive impairment that made it impossible to conduct a reliable interview. The hospital authorities granted permission to carry out the study.
Outcome measure
The outcome variable was blood pressure control defined as blood pressure ≤140/90 mmHg.
Statistical analysis
Analysis of the data collected was performed using SPSS 16 for windows. Continuous data was presented as means and standard deviation, while categorical data was presented as percentages. Differences between means of two groups was compared using student’s t-test, while differences between proportions was compared using the chi-squared test and equivalents. Logistic regression was used to determine factors of blood pressure control. The variables that were significant in the univariate analysis were included in the multivariate logistic regression model. A P value less than 0.05 was considered significant.
Results
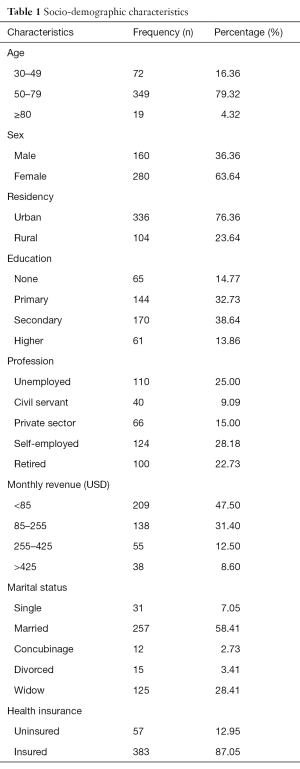
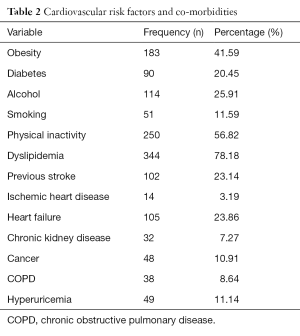
Socio-demographic characteristics, cardiovascular risk factors, co-morbidities and clinical characteristics
Among the 440 patients enrolled in the survey, 280 (63.6%) were females. Sociodemographic characteristics are summarized in Table 1. The mean age was 61.1 (SD ±11) years. Men were older than women (mean age 62 vs. 60 years old, P=0.03). The most common age group was 50–79 years (79.3%). More than three quarters of patients had academic achievement beyond primary school level. The majority were married (58.4%), lived in an urban area (76.4%), uninsured (87.1%) and unemployed (25%). More than half (56%) of the patients were physically inactive and more than three quarters had dyslipidemia. About 40% of the patients had obesity and 26% were consumers of alcohol. The most common co-morbidities were heart failure (23.86%) and previous stroke (23.14%) (Table 2). The mean systolic and diastolic blood pressures (DBPs) were 147.15 mmHg (SD ±22) and 88.43 mmHg (SD ±13) respectively. Only 36.82% of patients had blood pressure ≤140/90 mmHg. About 30% of patients had severe hypertension.
Full table
Full table
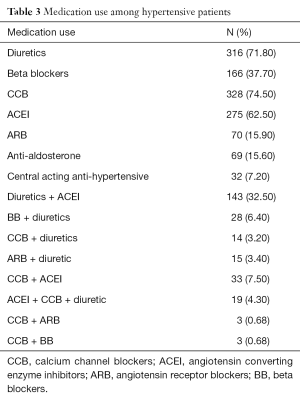
Anti-hypertensive medication and lifestyle modification
The most common class of anti-hypertensive medication was calcium channel blockers (CCB) (74.64%); followed by thiazide diuretics (71.98%) and angiotensin converting enzyme inhibitors (ACEI) (62.76%). The most common combination drug therapy used was the association of a diuretic and an angiotensin converting enzyme inhibitor (32.5%) (Table 3). About 60% of patients had good adherence to anti-hypertensive medication. More than 60% of patients were adherent to dietary lifestyle modifications. Only 20% of patients had a home blood pressure monitoring apparatus.
Full table
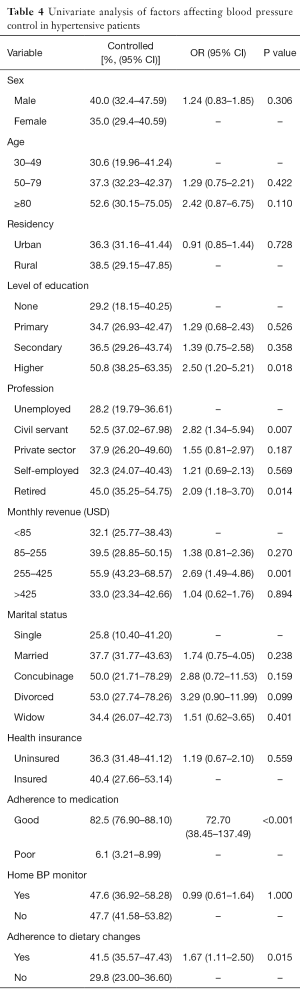
Blood pressure control and predictors
Overall, only 162 (36.81%) of patients had their blood pressure controlled. The result of univariate analysis of factors affecting blood pressure control is shown in Table 4. No cardiovascular risk factor was associated with blood pressure control. Multivariable logistic regression analysis showed that the following factors were independent predictors of controlled blood pressure: good adherence to anti-hypertensive medications (OR =3.99; 95% CI: 2. 20–7.23; P<0.000) and adherence to dietary lifestyle changes (OR =1.5; 95% CI: 0.53–2.49; P=0,031).
Full table
Discussion
The study represents the first analysis of factors that may be associated with blood pressure control in a large cohort of hypertensive patients in Yaoundé, the capital city of Cameroon. We observed that only one out of three patients had their blood pressure controlled. Result from multivariate logistic regression analysis showed that good adherence to anti-hypertensive medications and dietary lifestyle changes were associated with blood pressure control in this cohort. These rates of control among hypertensive adults on treatment are similar to those described in the United States (29–53%) and European (30–50%) populations (9,10) and higher compared with a previous report by Dzudie et al. in Cameroon (24.6%) in a population based study in 2012 (4). The higher rates of blood pressure control in our study population may be the result of patients having regular follow-up visits at dedicated hypertension clinics. Our blood pressure control rates was however slightly lower than that reported in previous studies in Ethiopia, Tanzania and South Africa with blood pressure control rates of 46.6%, 47.7% and 41.9% respectively (11-13).
There was no association between socio-demographic characteristics and blood pressure control. Also, there was no difference in rates of blood pressure control between men and women. These findings are similar to that reported in Tanzania by Maginga et al. (12). Living in an urban area is significantly associated with an increased risk of hypertension but in this report, there was no difference in blood pressure control between patients living in urban and rural settings. This is consistent with previous reports in Africa (14,15). In our report, insurance status did not have a significant association with blood pressure control, a similar finding that was reported in Tanzania (12). In the United States, studies have shown that among patients treated for hypertension, uninsured individuals are at lower odds of adequate blood pressure control (16). Unfortunately only a small proportion of patients in our setting have health insurance coverage. Education level did not affect blood pressure control rates, a similar finding that was reported in Tanzania (12).
Our present study found a significant association of blood pressure control with good adherence to anti-hypertensive medication and dietary lifestyle changes including low salt which was similar to findings in previous reports (17,18). Poor blood pressure control translates into increased cardiovascular morbidity and mortality. It has been documented from earlier studies that high adherence to antihypertensive treatment is associated with a significant decrease in the risk of cardiovascular events compared with lower adherence (19). Also, studies have shown that medication adherence is associated with lower rates of hospitalization and healthcare costs and emphasizes the need to create and test targeted interventions to increase adherence (20). More than half of the patients (60%) in our study were adherent to anti-hypertensive medication. This good adherence rate was lower than that reported in South Africa (13). Thus adherence in this population should be encouraged through education that anti-hypertensive medications should be taken daily and consistently even when feeling well. Educational interventions have been shown to improve adherence with blood pressure medications (21). Multiple factors that affect patient adherence to medications have been described, but these were studied in this report. Regarding anti-hypertensive medication, CCB and thiazide diuretics were the most prescribed drugs. Additionally, no specific medications were poorer versus better blood pressure control in multivariable analysis suggesting that other factors other than medication class may be determinants of blood pressure in this setting. There was no association between cardiovascular risk factors and blood pressure control in our study population. This contrary to other studies in Africa and developed countries that showed that alcohol consumption was associated with decreased blood pressure control (12,18). Although we did not have any association between cardiovascular risk factors and blood pressure control, interventions should promote a reduction in hypertension risk factors in this population to reduce cardiovascular morbidity and mortality.
Limitations
A degree of bias may exist in this present study. We did not assess patients’ knowledge of hypertension. However, these data have relevant clinical implications. This study provides a framework for identifying hypertensive patients who are at high risk of poor control, and identified factors may be amenable to improvement.
Conclusions
In this study of blood pressure control in hypertensive adults in Cameroon, only one out of three patients had their blood pressure controlled. Adherence to medication and dietary lifestyle changes are important factors for blood pressure control in patients with hypertension in this setting. This demonstrates that a high rate of blood pressure control is achievable in this resource limited setting if treatment adherence is improved. Identification of patients at risk of non-adherence to treatment and poor blood pressure control can lead to targeted interventions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement:The hospital authorities granted permission to carry out the study.
References
- Yusuf S, Reddy S, Ounpuu S, et al. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 2001;104:2746-53. [Crossref] [PubMed]
- Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA 1996;275:1571-6. [Crossref] [PubMed]
- Twagirumukiza M, De Bacquer D, Kips JG, et al. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies. J Hypertens 2011;29:1243-52. [Crossref] [PubMed]
- Dzudie A, Kengne AP, Muna WF, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open 2012.2. [PubMed]
- Kingue S, Ngoe CN, Menanga AP, et al. Prevalence and Risk Factors of Hypertension in Urban Areas of Cameroon: A Nationwide Population-Based Cross-Sectional Study. J Clin Hypertens (Greenwich) 2015;17:819-24. [Crossref] [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-52. [Crossref] [PubMed]
- Pereira M, Lunet N, Azevedo A, et al. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 2009;27:963-75. [Crossref] [PubMed]
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67-74. [Crossref] [PubMed]
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation 2013;127:e6-e245. [Crossref] [PubMed]
- Kearney PM, Whelton M, Reynolds K, et al. Worldwide prevalence of hypertension: a systematic review. J Hypertens 2004;22:11-9. [Crossref] [PubMed]
- Ambaw AD, Alemie GA. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health 2012;12:282. [Crossref] [PubMed]
- Maginga J, Guerrero M, Koh E, et al. Hypertension Control and Its Correlates Among Adults Attending a Hypertension Clinic in Tanzania. J Clin Hypertens (Greenwich) 2016;18:207-16. [Crossref] [PubMed]
- Adebolu FA, Naidoo M. Blood pressure control amongst patients living with hypertension presenting to an urban district hospital outpatient clinic in Kwazulu-Natal. Afr J Prim Health Care Fam Med 2014;6:E1-6. [Crossref] [PubMed]
- Riha J, Karabarinde A, Ssenyomo G, et al. Urbanicity and lifestyle risk factors for cardiometabolic diseases in rural Uganda: a cross-sectional study. PLoS Med 2014;11:e1001683. [Crossref] [PubMed]
- Seedat YK. Perspectives on research in hypertension. Cardiovasc J Afr 2009;20:39-42. [PubMed]
- Duru OK, Vargas RB, Kermah D, et al. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens 2007;20:348-53. [Crossref] [PubMed]
- Cutler JA. Combinations of lifestyle modification and drug treatment in management of mild-moderate hypertension: a review of randomized clinical trials. Clin Exp Hypertens 1993;15:1193-204. [Crossref] [PubMed]
- Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation 2008;117:e510-26. [Crossref] [PubMed]
- Blood Pressure Lowering Treatment Trialists' Collaboration, Turnbull F, Neal B, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ 2008;336:1121-3. [Crossref] [PubMed]
- Sokol MC, McGuigan KA, Verbrugge RR, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 2005;43:521-30. [Crossref] [PubMed]
- Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care 1998;36:1138-61. [Crossref] [PubMed]


