Post-traumatic ventricular septal defect: a rare indication for extracorporeal membrane oxygenation as a bridge to transplant
Introduction
The incidence of isolated traumatic ventricular septal defect (VSD) in the setting of non-penetrating trauma is extremely rare. The management usually involves timed surgical repair, which depends on the patient’s clinical condition and the presence of other injuries (1). Ventricular assist with extracorporeal membrane oxygenation (ECMO) has become a rescue option for patients in refractory cardiogenic shock of different etiologies (2). Since ECMO indications are currently spreading, we present a rare case in a post-traumatic VSD where its support allowed us to bridge the patient to heart transplantation after failed repair surgery.
Case presentation
A 44-year-old male with unremarkable past medical history was crushed by a rock in a mine. On arrival to the emergency room, he was conscious, hemodynamically stable and with severe chest pain. Inspection revealed bruises on his back and the left side of the chest. A pansystolic murmur was audible. Electrocardiogram showed sinus tachycardia and right bundle branch block. Blood tests showed elevated markers of myocardial damage (total CK 2757 IU/L, Troponin I 187 ng/mL). A total body scan was performed, showing multiple fractures in left ribs and scapula, left pneumothorax, pneumomediastinum and bilateral pulmonary contusions.
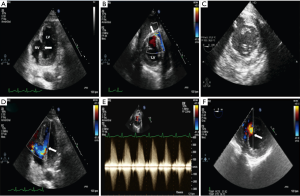
Few hours after admission to the ICU, the patient had two episodes of non-sustained ventricular tachycardia followed by hemodynamic instability, needing endotracheal intubation and increasing inotropic support. Echocardiography showed a discontinuity of 2.5 cm in the inferior segment of the interventricular septum (IVS), with left-to-right shunt (Figure 1). Moderate tricuspid regurgitation was also observed. Biventricular contractility was preserved. With these findings emergent surgery was carried out. A right atrial approach was used. The VSD was exposed through the tricuspid valve. The defect was in the inferior middle portion of the IVS, had irregular borders and the tissue around was friable. A PTFE™ patch was sutured to the limits of the contused myocardium, in the right ventricular side of the VSD and a tricuspid mechanical prosthesis implantation was necessary. Few hours later, the patient developed profound shock despite inotropes and intra-aortic balloon pump support, with progressive worsening of renal and liver function (Creatinine 1.5 mg/dL, Urea 53 mg/dL, ALT 718 IU/L, AST 752 IU/L) and increasing lactic acid (5.9 mmol/L). Echocardiography showed detachment of the interventricular patch, with a recurrent left-to-right shunt and rapid progressive deterioration of right ventricular systolic function (Figure 2).
In view of the clinical deterioration and echocardiographic findings, a peripheral veno-arterial ECMO was implanted, to attempt the stabilization of patient’s hemodynamics and improvement of organ dysfunction, while the stunned myocardium could recover. Clinical and hemodynamic outcomes after ECMO implant were satisfactory, with progressive improvement of metabolic status and normalization of renal and hepatic function. On day 3 with ECMO, the RV systolic function was severely depressed, he was dependent on IABP support and the VSD was bigger on the echocardiography. Due to the low probability of success with another surgery to repair, the patient was listed for heart transplantation on an urgent basis. On day 10 after ECMO implantation, a compatible donor was available and heart transplant was carried out successfully.
Discussion
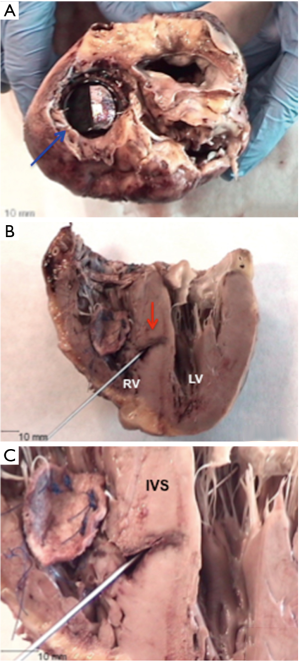
Blunt chest trauma may be associated with a variety of cardiac injuries, being VSD an uncommon complication. Several theories concerning the pathogenesis of traumatic VSD have been described. The main mechanism is the compression of the heart between the sternum and spine causing a sudden pressure increase, during the early systole or late diastole, when ventricles are filled and the valves are closed. The resulting myocardial contusion injury causes a microvascular disruption, leading to necrosis of the IVS, facilitating the rupture at this point (1). In our case, the surgeons found a defect with irregular borders and surrounded by friable myocardial tissue. Macroscopic findings in the study of the explanted heart showed a patch in the right ventricular face of the IVS, with a residual communication of less than one centimeter, with bleeding edges (Figure 3). These findings suggest that the compression of the thoracic cavity by a heavy stone caused the immediate rupture of the IVS after injury, and given the appearance of the tissue surrounding the defect, the myocardial necrosis had a significant role.
Presentation of traumatic VSD is variable, ranging from acute cardiac failure to detection of asymptomatic defects several months later. Echocardiography provides diagnosis in the majority of cases and should be considered in all cases of blunt thoracic trauma where cardiac injury is suspected.
The most appropriate management strategy remains unclear. When surgical repair is indicated, the timing of surgery is the most controversial and difficult decision to make, depending on the patient’s clinical condition and associated injuries. In this case, given the rapid hemodynamic deterioration, urgent surgical repair was attempted, but the patch detached within hours, probably due to the contused myocardium frailty. This situation has been well described in patients with post-infarction VSD. In this setting, using ECMO as a bail-out approach to bridge the unstable patient towards a definite surgical repair has been reported (4,5). In our patient, the early failure of surgery brings to mind that, although the underlying mechanism of VSD is different, one must expect a similar behavior of friable myocardial tissue as in post-infarction VSD. In view of these results, ECMO support may play a crucial role to allow an optimal timing of surgery in these patients. Finally our patient had to be transplanted. Severe injuries in the IVS and right ventricle failure made a new surgical repair unsuitable.
To the best of our knowledge, this is the first case where ECMO is implanted as a bridge to transplantation after failure of surgical repair of post-traumatic VSD.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: We could not obtain the informed consent from the patient because he had died. The relatives of the deceased patient could not be traced and their consent could not be obtained either. The authors ensure that all the details that would enable any reader to identify the patient are omitted and all images included in the case report are completely anonymised.
References
- Rootman DB, Latter D, Admed N. Case report of ventricular septal defect secondary to blunt chest trauma. Can J Surg 2007;50:227-8. [PubMed]
- Yoann L, Erwan F, Nicolas N, et al. Extracorporeal life support in a severe blunt chest trauma with cardiac rupture. Case Rep Crit Care 2013;2013:136542.
- Restrepo-Córdoba MA, Hernández-Pérez FJ, Gómez-Bueno MF, et al. Transesophageal echocardiogram in transgastric view after surgical repair. Note the persistent large ventricular septal defect after patch detachment. Asvide 2017;4:007. Available online: http://www.asvide.com/articles/1313
- Neragi-Miandoab S, Michler RE, Goldstein D, et al. Extracorporeal membrane oxygenation as a temporizing approach in a patient with shock, myocardial infarct, and a large ventricle septal defect; successful repair after six days. J Card Surg 2013;28:193-5. [Crossref] [PubMed]
- Rohn V, Spacek M, Belohlavek J, et al. Cardiogenic shock in patient with posterior postinfarction septal rupture--successful treatment with extracorporeal membrane oxygenation (ECMO) as a ventricular assist device. J Card Surg 2009;24:435-6. [Crossref] [PubMed]


