Cardiovascular burden and percutaneous interventions in Russian Federation: systematic epidemiological update
Cardiovascular (CV) disease is the leading global cause of death, accounting for 17.3 million deaths per year, a number that is expected to grow to more than 23.6 million by 2030 (1-4). The burden of CV diseases and particularly coronary heart disease (CHD) is projected to rise from around 47 million disability-adjusted life years (DALY) globally in 1990 to 82 million DALY in 2020. More than 60% of the global CV burden occurs in developing countries. CV disease is responsible for 10% of DALY lost in low- and middle-income countries, and 18% in high income countries (1-4).
The situation with CV burden in Russian population remains critical, and becomes of high interest due to high CV mortality, and shorter lifespan if compare with the Western society. CV diseases in Russia accounted for 54.9% of all deaths (1.739 millions of about 143.4 million people, 2012), while the share of all non-communicable diseases (NCD) and injuries was about 90% (5-10).
Regretfully, Russia, unlike the U.S., Commonwealth of Nations and European Union (E.U.), has no established monitoring or screening system for major CV risk factors which makes impossible to get a comprehensive vision of their prevalence and trends. Moreover, there are no real-world general population randomized studies that might characterize the modern-day concerns of the Russian Public Health system which impair CV burden in Russia. We conducted this analysis with the purpose to explore CV burden in Russia matching data of the results of the national CV screening and a prospective randomized real-world population NANOM-FIM trial as the only available real-world population study.
Methods
We overviewed data from a number of the available Russian-speaking data sources of 2001-2014 from Bokeria’s Cardiac Center (11,12), Russian Federal State Statistics Service (FSSS) (13), annual screening report of Russian Ministry of Health (14,15), RIA news (integral socio-economic rating) (16), and NANOM-FIM trial (NCT01270139) (17-21) in comparison with the data sets for the European region of the European Health For All DataBase (HFA-DB) of the World Health Organization (WHO) Regional Office for Europe (22). This epidemiological systematic review (without meta-analysis) was carried out by two reviewers who worked independently to screen abstracts, extract data and assess risk of bias, thereby reducing the chance of reviewer bias and increasing reliability. Data sources and data sets were chosen with consideration of the data quality, date of most recent update, and coverage of all Russian regions. These sources are refreshed annually through routine and administrative data collections and they allow for an overview of the burden and distribution of CV diseases in Russia through the mortality, morbidity, and treatment. The WHO European region database (22) doesn’t contain any appropriate data sets about 83 regions of Russia to be a representative source of the health information, and any matching of the European and Russian data is essentially not ‘ideal’ due to difference in epidemiological approaches and statistical methods. The received data have the different quality, and potential of comparability, but describe the most up-to-date information about CV burden in Russia. It was inapplicable to get our data standardized by the 2013 European Standard Population (ESP) or by WHO Standard Population Average 2000–2025 because ESP was developed for EU-27 plus EFTA countries (it was not coordinated with Russia) and proportion of WHO dramatically differs from that in Russia, but the age distribution between ESP, WHO Standard and Russian populations as well as correlation and Russian national coefficient for standardization of the provided data were calculated. We investigated the available Russian- and English-speaking sources of the information about risk factors and CV burden in Russia published between 2010 and 2016 in PubMed/ Medline (primary electronic database), Google Scholar, ResearchGate, Russian Science Index (elibrary.ru), and SCOPUS with the medical subject headings and free-text terms including such key-words as Russia, Soviet Union, cardiovascular burden, mortality, public health, insurance, diet, economics, statins, stenting, poverty, nutrition, policy, and risk factors. The existence of running and completed trials in general and real-world population in Russia was tested with ClinicalTrials.Gov. A Service of the U.S. National Institutes of Health registered 3,254 trials by February, 2016, but mostly in selected Russian cohorts involved to the international studies with the specific profiles of the population.
Database of Bakulev Cardiac Center
The CV, CHD or coronary artery disease (CAD) morbidity rates, number of underwent angio/quantitative coronary angiography, percutaneous cardiovascular intervention (PCI), stenting and coronary artery bypass surgery (CABG) received from the Russian-speaking national database of the Bakulev Cardiac Center (Bakulev Research Center for Cardiac Surgery of the Russian Academy of Medical Sciences, Moscow, Russia) which was released (11,12) under the supervision of Prof. Leo Bokeria, M.D., D.Sc. The database was routinely collected from all the licensed Russian hospitals (1,332.3 thousand hospital beds, or 92.9 beds per 10,000 in 2012; 3.9 beds for cardiology per 10,000). The data presented for the Russian population of 143,056,000 people in 2012 (a 0.1% gain if compare with 2011) or 143,347,000 citizens registered in 2013 (a 0.2% gain matching with 2012) with a 73.9% urban population in 2012 and 74.0% in 2013. The number of cardiologists in Russia achieved 0.9 per 10,000 in 2012. The database of PCI and stenting was directly gathered from 202 PCI centers (337 cath labs with 1,023 interventionalists/ invasive cardiologists) across Russia in 2013 without involvement of the Russian Ministry of Health. The results were independently evaluated by the Russian Society of Roentgenoendovascular Diagnostics and Treatment under the supervision of Prof. Leo Bokeria, MD, D.Sc., and Prof. Bagrat Alekyan, MD, D.Sc. (11,12).
Database of the Russian FSSS (Rosstat)
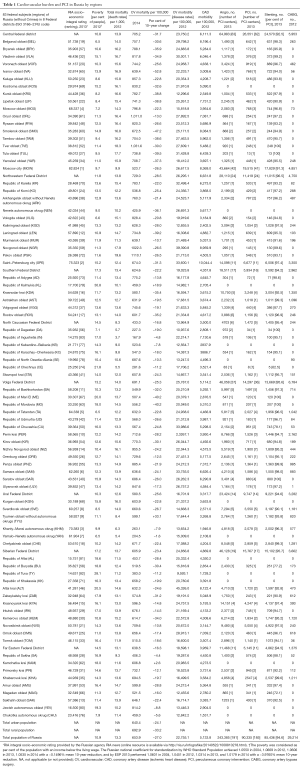
The total mortality (since 1980), CV mortality (in 2004-2014), and some risk factors data sets come from the online-available database of the Russian FSSS (13) for population of 143,056,400 in 2012 (74% of urban population), 143,347,100 in 2013 (74.2% of urban) and 146,267,300 in 2014 (a 74% urban). These data were compared with the total mortality rates in E.U. received from the European Commission’s Eurostat database (1980–2014). The data were presented for 83 constituent entities (without Crimea) of Russian Federation. As of 1 January 2014 there were the following units: 22 Republics (with Crimea), 9 territories (krai), 46 regions (oblast), 3 cities of the federal subordination (with Crimea), 1 autonomous region (oblast), 4 autonomous districts (okrug). They are given in Table 1 referring to eight Federal Districts established according to the Decree of the President of the Russian Federation No 849 of May 13, 2000. The data from two new federal subjects which were established in the Russian Federation in 2014 (Federal Constitutional Law of the Russian Federation of March 21, 2014 No 6-FKZ “On the connection of Republic of Crimea to the Russian Federation and establishment of new entities in the Russian Federation—Republic of Crimea and the federal city Sevastopol”, and Decree of the President of the Russian Federation on March 21, 2014 No 168 “On the formation of the Crimean Federal District”) (13) were not included to the analysis.
Full table
Screening Database of the Russian Ministry of Health
The data sets of the federal national screening of the Russian population provided by the regular screening report of the Russian Ministry of Health published (14,15) online in 2015 (with results of 2014). In accordance with the Presidential Decree of May 7, 2012 and the orders of the Government of the Russian Federation in 2012–2014, the Ministry developed and approved the most important strategic documents to improve the quality and accessibility of health care, human resources policy in the sphere of health, improving drug supply, the development of medical science, healthy lifestyles and other essential directions including multi-step mass screening of the population. The most direct and effective organizational technology in this regard is the formation of an annual report on health status and health organizations on the basis of the executive authorities of the Russian Federation, which is a result of constant observation of the public health system and health development (14,15).
The clinical examination (screening) of the population considered as one of the most important mechanisms maintaining health and reducing mortality in Russia. The effectiveness of the screening was a priority of the Russian Ministry of Health in 2014. The screening of the adult population was conducted in 2014 in accordance with the Regulations of the medical examination of certain adult groups approved by the Russian Ministry of Health (Order No 1006n of December 3rd, 2012). The screening at least once every three years, subject to the employed and unemployed citizens, as well as studying in educational organizations. The screening was carried out in two stages. First step of the clinical examination (screening) was performed to identify the citizens with signs of chronic non-communicable diseases (NCD), their risk factors, illegal consumption of narcotic drugs and psychotropic substances, and the determination of medical indications for implementation of additional tests and examinations by experts to refine the diagnosis in the second stage of the clinical examination. The second stage was carried out with the aim of further investigation and clarification of the diagnosis as well as in-depth preventive counseling. The clinical examination of the adult population was implemented within the free-of-charge program of the state guarantees. A 49.2 billion rubles (558.8 million euros, a 88.04 exchange rate of February 2016 available from the Russian Central Bank) were paid in 2014 to carry out medical examinations (screenings) and preventive health inspections of healthcare organizations. Totally, medical examinations (screening) were undergone in 40.1 million people in 2014: 22.4 millions of the adult population (24 million people were scheduled), and 17.7 millions of children (18 millions were on agenda) (14,15).
Direct health care costs related to treatment of myocardial infarction (MI) and stroke events were calculated for analysis by multiplying a unit cost with each event from the available database of the Russian Ministry of Health and insurance data of the Ural Institute of Cardiology (Yekaterinburg, Russia). Direct health care costs attributable to the third-party payer were included. The exchange rate (between rubles, U.S. dollars and euros) was extracted from the database of the Russian Central Bank (www.cbr.ru) on the date of the calculation. The information about markets of statin drugs and devices which serve the needs of the interventional cardiology were collected from the published Russian- and English-speaking data sets in Medline/PubMed and Russian Science Index.
RIA socio-economic integral rating
The rating of the socio-economic situation in 83 regions (without Crimea) of Russia is calculated (16) by the RIA news agency on the basis of the aggregation of the groups of indicators characterizing the economic, social and fiscal spheres. Each group includes a number of quantitative indicators for 2013 which were available on the official online databases of Rosstat (FSSS), the Federal Ministry of Finance, and the Federal Treasury. There 16 quantitative indicators were used in total for the construction of a rating, but without expert estimation. The ranking of Tyumen and Arkhangelsk oblasts (regions) were determined without taking into account their autonomous territories (16).
Real-world population of NANOM-FIM randomized trial
The NANOM-FIM trial was an observational prospective cohort analysis (initiated as a PROBE randomized trial) of the 1-year imaging and clinical outcomes (17,18) with the further consecutive assessment of clinical outcomes at 5 years at the intention-to-treat population (19) of 180 patients with CAD and angiographic SYNTAX score ≤22 (17-21). The study tested a plasmonic photothermal therapy of atherosclerosis with silica-gold nanoparticles in chest-pain all-comers which means patients who admitted to the cardiac hospital (Ural Institute of Cardiology, Yekaterinburg, Russia; www.cardio-burg.ru) via outpatient department or with ambulance. The methodology and results of this original study (NCT01270139, registered on December 30th 2010) which was completed technically in 2010 and ultimately resumed in 2012 were previously published (17-21). All clinical outcomes and biochemical investigation of subjects were assessed at the Outpatient department of the Ural Institute of Cardiology (Yekaterinburg, Russia) within regular examinations two times per year between 2007 and 2015. Information about patients lost to follow-up was received from archive of general practitioners in the subjects’ community retrospectively. The experimental and clinical protocol was approved by the Ethics Committee and the Research Steering Committee of the Ural Medical University (Yekaterinburg, Russia) as a body of the Russian Ministry of Health. The methods were carried out in accordance with the approved international ESC/ACC/AHA guidelines. The informed consent was obtained from all subjects (17-21).
Statistics
The Kolmogorov-Smirnov test was used to prove Gaussian distribution allowing for calculation of the mean and standard deviation. Non-Gaussian samples are described by median and range. Discriminant variables are evaluated with the two-sided Fisher’s exact test. Continuous variables are compared with student’s unpaired t-test. Differences between some groups in a randomized trial were analyzed by means of a repeated-measures 1-way ANOVA followed by a Fisher’s post hoc test. We used the Cox proportional hazards ratios (HR) and 95% confidence intervals (CI) for the endpoints. An event of diabetes, heart failure, previous percutaneous coronary intervention (PCI), male gender, smoking, alcohol abuse and hypertension were forced into all of the multivariable analysis. The cumulative incidence of adverse events was estimated according to the Kaplan-Meier method, and differences between groups were compared using the log-rank test. Patients lost to follow-up were considered at risk until the date of last contact, at which point they were censored. For all tests the significance level α is 0.05. Statistical analysis was performed with SPSS 20.0 software (SPSS Inc., Chicago, IL, USA).
Results
At 17,075,400 square kilometers (6,592,800 sq mi without Crimea), Russia is the largest country in the world, covering more than one-eighth of the Earth’s inhabited land area with a broad climatic and biodiversity. Russia is the world's ninth most populous country where the situation with CV burden remains alerting, being relatively civilized and industrialized country, and an estimated gross domestic product (purchasing power parity) GDP (PPP) per capita which equal to 23,744 U.S. dollars [53rd economy by GDP (PPP) per capita and 6th by total GDP (PPP) in the world in 2015]. A 11.2% of Russians live below the national poverty line [2014] with the average nominal monthly wages of 32,611 rubles (or 728.41 euros in 2014; about 374.83 euros by 2016 due to collapse of ruble), and the federal minimum wage of 6,204 rubles (70.47 euros since January 2016) (5-10). Meanwhile, the source of the Russian Higher School of Economics (23,24) reports a 41.4% poverty (by the subjective evaluation) of the Russian population in June 2016. Russian cardiologists remain one of the most unsatisfied groups of the population with the mean annual compensation of 9,621 U.S. dollars (13,16) if compare with 410,000 U.S. dollars in the United States in 2015 (Medscape Cardiologist Compensation Report 2016).
General and medical demographics of Russian population
According to Rosstat (5-10,13,15), the permanent population of the Russian Federation on January 1, 2015, excluding the Crimean Federal District amounted to 144.0 millions (including the Crimean Federal District—146.3 million people), and increased by 305.5 thousand people or 0.2% during 2014. The documented population growth was related to both the emerging patterns of migration, and the natural growth of population.
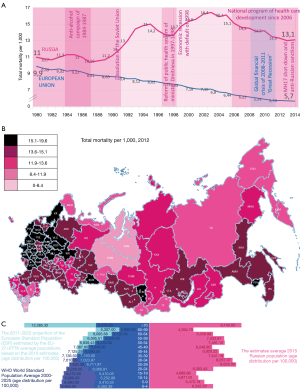
A 1,913,613 people have died in Russia in 2014, which is a 0.2% less than in 2013 (1,910,623 people). The reduction of mortality observed in 34 regions of Russia (see Table 1, Figure 1), the most significant—in Nenets Autonomous Okrug—a 16.8% decrease, in the Republic of Mordovia: by 3.4%; in Novgorod oblast: 2.8%; in St.-Petersburg city and the Republic of Buryatia: 2.5%; in Smolensk oblast: by 2.4%; in Novosibirsk Oblast: by 2.2%; Vologda oblast: by 2.0%; in Kostroma; Yaroslavl and Kirov oblasts: 1,9%; and in the Republic of Altai: 18%. The death rate is not changed in 18 Russian regions. The lowest mortality rates are observed: in the Republic of Ingushetia: 3.5; in the Chechen Republic: 5.0; in Yamalo-Nenets Autonomous Okrug: 5.1; in the Republic of Dagestan: 5.6; and Khanty-Mansi Autonomous Okrug: 6.4 per 1,000 population. The highest rates are found in Pskov oblast: 18.5; Tver oblast: 17.8; Novgorod oblast: 17.3; Tula oblast: 17.1; Kursk oblast: 16.6; and in Vladimir oblast: 16.5 per 1,000 population (11,12,14,15).
The first position in the structure of the causes of death in Russia (2014) (14,15) is still occupied by the CV diseases—49.9% or 653.9 per 100,000 of the population (a 6.6% drop), in second place-neoplasms—15.3% or 201.1 per 100,000 with a decline of 0.2%, the third—external causes—9.1%, or 118.8 per 100 thousand people (0.6% decrease), including road accidents—14.0 per 100 thousands (without dynamics), then—diseases of the digestive system—5.0%, or 66.1 per 100 thousand of the population (growth by 8.4%), respiratory diseases—4.0%, or 53.0 per 100 thousands (an increase of 6.2%).
Cardiovascular mortality and major national risk factors
The highest CV mortality of 1,110.1 per 100,000 documented in Pskov oblast (see Table 1 and Figures 2,3) (13). The phenomenon of this region as well as of so called ‘Black Belt’ of Europe (with CV mortality above 1,000 per 100,000) including such regions as Pskov oblast (1,110.1 in general population, and 1,402.6 in rural population), Oryol oblast (1,011.0—in general, and 1,230—in rural), Tver oblast (1,031.6 in general, and 1,152.3 in rural), and Novgorod oblast (1,022.3 in general, and 1,215.2 in rural) of Russia (2014) (13), and countries as Belarus (1,448 in males, and 726.9 in females in 2011), Ukraine (1,544.9 in males, and 1,065.8 in 2012), Moldova (1,380.2 in males, and 1071.6 in females in 2013), Romania (1,143.9 in males, and 903.9 in females in 2012), Bulgaria (1,332.3 in males, and 970.3 in females in 2011), and FYR Macedonia (1,228.8 in males, and 1,012.5 in females in 2010) (1) is not yet clarified.

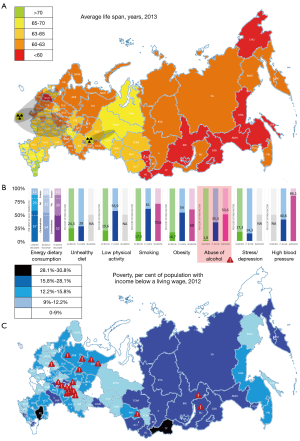
A 28% increase in CV mortality might be attributed to the so called ‘Russian diet’ (24.3% of screened pts) with abundance of (I) saturated (‘butter-and-mayo culture’) and trans (‘fast-food culture’) fat; (II) sugar and carbohydrates (‘white bread culture’); and (III) strong alcohol (‘vodka culture’). The smoking (17.3% of screened with a 2,786 cig a year; 63.2% of male and 9.1% of female; 70.6% in the trial; a contribution to mortality is about 29%), excessive alcohol consumption (1.8% of screened with a 11.6 L per year mostly of beer and vodka; 50.6% in the trial; about 70% consumed strong alcoholic beverages; responsible for 25.6% of CV deaths in male and 15.4% in female), unhealthy diet with insufficient consumption of fruits, vegetables, sea food, unsaturated fat, and proteins (mean 12% of the daily consumption) with abundance of carbohydrates/ sugar (up to 57% of diet), saturated and trans fats (up to 29–40% of the energy) including palm oil, butterfat, mayonnaise, and junk processed red meat), psychosocial factors (75% of Russians are not adapted to new living conditions, 20%—stress, 11.7%—anxiety, and 9.6%—depression) and physical inactivity (19.6% of screened; at least 73.9% of men and 74.8% of women) remain the major modifiable risk factors. They, in turn, affect (see Figure 3) (5,14,15,17-22,25-30) such risk factors as dyslipidemia (86.7% in the trial), obesity (16.7% of screened; mean BMI in the trial was 28.4), and hypertension (about 40.8% suffered; 86.1% in the trial), which is relevant to findings of the EUROASPIRE IV trial (31,32) in the European population, and screening studies of the Russian Higher School of Economics (23,24).
The lowest CV mortality revealed in both poorest and richest regions of Russia without strong correlation with socio-economic development (R2=0.1752, r=0.0540, P=0.63), but with a weak or moderate association with a poverty (R2=0.1999, r=0.2574, P=0.02) there, and particularly in two regions in Caucasus (167.9) and Yamal (204.5) with a life style trending toward higher physical activity (PA), and predominant consumption of fish (Mugil fish and Clupeidae fish, or herrings in the mountain subtropical South, and Coregonus fish, especially Muksun, a type of whitefish or a relative of salmon in the Arctic zone respectively) without culture of unsaturated oil (no olive oil or omega-3 type of oil industry; the Black-Sea olive-tree cultivation starts in 1975, however the climate is not optimal), but with a ‘moonshine-and-deer-meat culture’ in the North and a ‘wine-brandy-and-lamb-meat culture’ in the South including low or moderate consumption of alcohol. In both regions people avoid consumption of butter, mayo or processed meat, they prefer to grill and smoke their fresh meat and fish, and never fry which means they totally exclude saturated and trans fats. The Russian Caucasus is quite unique climatic zone with excellent ecology, subtropical mountain environment with very close neighborhood of two seas—The Black Sea and The Caspian Sea—with very specific nature and abundance of fruits, vegetables, grains and nuts (hazelnut, nuts of beech tree, walnut, peanut) when the vegetation/growing season lasts at least 200–240 days a year. Undoubtedly, the Caucasian lifestyle is more similar to the principles of the Mediterranean diet, but in Arctic Yamal with an 8-month winter and extreme temperatures down to −70 °C there is another situation. This is the only Arctic region in Russia with such a low CV mortality (in 2004 there was a CV death rate of 207.8 if compare with 715.4 in Murmansk oblast, 666.0 in Nenets autonomous okrug of Arkhangelsk oblast, 352.7 in Taymyr autonomous okrug of Krasnoyarsk krai, 424.9 in Republic of Sakha, and 486.0 in Chukotka autonomous okrug) amid high Arctic Sea fish oil consumption and relatively advanced economic development of the region (7th in the federal ranking of 83 regions) due to presence of gas and oil industry, but despite some ecological concerns first of all from Ob river with the highest industrial and radioactive pollution (from Chelyabinsk oblast, after accident in Ozersk of 1957 up to 0.1–2 Ci/km2 in Ob river, and 2.75 Ci/km2 in Techa river which is the most radioactive river in the world) in Russia with the methylmercury exposure (see Table 1, Figures 2,3). This Arctic paradox is very challenging phenomenon. Seasonal variation of CV morbidity and mortality was previously noted across the globe (27) with the highest rates in the coldest months of winter and late spring or very hot summer because of the rather complex mostly acute adaptive reaction. Such a detrimental impair of the cold weather was related to the seasonal variations of the plasma level of fibrinogen, cholesterol, hormones, and other vasoactive substances, but this phenomenon was studied in the regions with very moderate warm climate. Most probably, the long-term or lifelong accommodation in the Arctic zone plays some beneficial role for reduction of CV burden which is not well understood.
Nutrition
The nutritional trends in Russia are discouraging (5,33,34) whereas the above-mentioned principles of the Russian diet. The decline in fruit and vegetable consumption alone is attributable to a 28% increase in CV mortality in Russia especially after 1994 when the average per-capita consumption of vegetables in Russia fell from 85 kg per year in 1990 (a 75% of the USA consumption) to 71 kg. Since the Soviet time the recommended daily intake for protein was almost twice that of Europe and North America, creating the erroneous belief that such high intakes of the mostly saturated fat and ‘processed’ protein/meat are necessary for maintenance of health (5). The total recommended daily amount of calories for a Soviet person till 1991 ranged from 2,800 to 3,600 for males and 2,400–3,100 for females, depending on their occupation. People of all ages in Russia suffered from an excess intake of the ‘processed’ red-meat protein and saturated fat with bread, sugar and potatoes, rather than a deficiency, a trend that continues to the present day despite relatively high prices for these commodities. From 1992 to 1998, the proportion of the Russian population living below poverty level increased from 12 to 46%, with very immediate impact on food availability, but with the average energy consumption of about 2,900 kcal (mostly simple carbohydrates, saturated fat, some grain, potato, beetroot and carrot) per capita per day in 1990–2000 (about 70% of the Russian households experienced hunger in early 90s after the dissolution of the Soviet Union) (33).
Meanwhile, the modern-day Russia’s food environment falls short in offering healthy choices at affordable prices. The availability of vegetables and fruits in Russia is lowest if compare with other countries in the WHO European Region and below the recommended threshold of 400 g per capita per day (only in early autumn Russians consume more than 400 g of vegetables daily: 75% males and 81% females) down to 300–340 g. The consumption of meat (including red meat and chicken) in 2012 achieved 74 kg per person per year (a 34.5% 5-year gain); milk: 249 kg (a 6.4% gain since 2005); eggs: 276 kg (a 10.4% increase); sugar: 40 kg (a 5.3% gain); potatoes: 111 kg (a 1.8% 5-year growth); vegetables: 109 kg per year (highest at the Republic of Dagestan with 231 kg per person, but just 83 kg at the zone of the Arctic paradox) or 298.6 g a day (a 25.3% 5-year gain); oil (mostly sunflower): 13.7 kg (a 13.2% increase); and bread: 119 kg a year (a 1.7% 5-year loss). The average percent of energy (33,34) from fat achieves 29.4 in low-income population, 32.9—in middle income, and 33.4%—in high-income screened subjects decreasing from 40% to 29% (mostly of saturated fat) between 1992 and 2000. Protein intake as a per cent of energy displayed very similar trends (about 12–14%) to fat intake, decreasing among all groups, but with the lowest-income groups consuming the least protein in all years (below 12% of the consumption per day), and continuing to decrease after the middle and higher income groups stabilized. These decreases in fat and protein were compensated for by commensurate increases in carbohydrate intake (from 45% to 57% of the daily energy consumption). Although trends indicate that the overall consumption of high-fat livestock product and sugar has decreased, people in Russia still consume too much saturated fat, sugar, junk meat, strong alcohol and not enough complex carbohydrates, unsaturated fat, sea food, chicken or pulses and nuts.
Physical activity
Despite the proven benefits of exercise, few people in Russia engage in regular PA (5,35). A behavioral risk factor surveillance system does not exist in Russia, but several surveys on PA behavior of the population have been conducted during the last decade. In the Russian Federation, 22.6% of the population aged 15 years and over were insufficiently active (men 22.9% and women 22.4%), according to estimates generated for 2008 by WHO. In a survey in Tver oblast in 2001, 56.9 percent of males and 51.4 percent of females reported low PA in their leisure time. The survey conducted in Russian cities in 2001-2002 found that 73.9–81.7 percent of men and 74.8–86.2 percent of women had low PA [less than 20-30 min a day or less than 3 metabolic equivalent of task (MET) daily] during their rest time. The cross-sectional analysis of the European population in 24 countries (31,32) registered 59.9% people who have a little or no PA. Meanwhile, a large study by Kokkinos et al. showed that fitness conferred a 13% reduction in mortality per MET achieved between 4 and 10 MET. However, there did not appear to be any additional benefit beyond 10 MET with a U-shaped dependence. Unfortunately, most probably more than 70% of the Russian population have intensity of the physical exercise less than 3–4 MET that potentiates a risk of obesity, high blood pressure, diabetes, atrial fibrillation and CAD despite the existence of the National program supporting sport in Russia since 2014 with some plans to invest at least 1.5 billion euros in 2016–2020 to build public sport facilities and communities. The situation with a public sport and development of the physical culture remains very complex in Russia with reduction of stadiums from 2,108 in 2000 to 1,805 in 2012, but a 42.9% 5-year expansion of the sport fields (138,259 in 2012), and a 82.1% increase of the public swimming pools (4,575 in 2012). The affordability of the Health & Sports centers for children dramatically decreased through the last 15 years from 6,170.6 thousand healthy children who underwent physical rehabilitation in 2000 down to 4,958.3 thousands in 2012.
Smoking
Russia is a country with one of the world’s highest rates of male smokers (5) being a 4th in the ranking with 2,786 cigarettes per adult per year (only Greece and Balkan countries ahead) vs. for instance 1,841 in Japan, 1,045 in Germany, 1,028 in the U.S., 801—in the Netherlands, and 750 cigs in the U.K. in 2007. To the word, about 15 to 20 percent of CV deaths in the U.K. and Central European countries are caused by smoking where at least 16% of the population (vs. min 22.2% in Russia) remain active smokers (31,32). According to the Public Opinion Foundation poll conducted in June 2014 regarding to the public opinion towards the governmental politics over tobacco control, 8 of 10 Russians (including exactly 50% of smokers and 90% of ex-smokers) support the measures taken by the State. According to Rosstat, a number of non-smokers aged 15 years or older increased from 61.8% in 2011 to 63.5% in 2014. In the large observational study of the alcohol abusers Zaridze et al. (35-37) reported 68.9% of smokers among adult males and 48.4% amongst females in the general population (n=131,252) with a 89.4% current smokers among male heavy abusers of the alcohol, and 63.9% among women in the cohort drinking more than half-litre bottle of vodka per week (n=4,051). At least 21.5% of men and 81.7% of women in the general population never tried to smoke. In another smaller study in students (17–21 years old, n=1,200) of the Russian Far East the smoking was documented in 78% of the screened subjects (60.3% of them were males).
The expansion of the e-cigarette culture, a “healthier alternative” (actually, with at least 40 toxic compounds and carcinogens; 0.5 to 15.4 mg of nicotine in 15 puffs of vapor) to conventional cigarettes (with 7,000 compounds with at least 70 recognized carcinogens; 1.54 to 2.60 mg of nicotine per cigarette), becomes critical for Russia in sense of both health and business. According to the 2015 edition of Eurobarometer, about 12% of the population tried e-cigarettes at least once, and 13% of them are of 15–24 years old. A 67% of the smoking population motivates consumption of e-cigarettes by the attempt to reduce or stop smoking tobacco, 44%—would smoke where tobacco smoking is not allowed, and 24% because they found it attractive. Regretfully, only 14% of them quit smoking. The Russian Senators are in the midst of preparing a bill for Russian State Duma (Parliament), which will ban the use of electronic cigarettes and vaping in Public Places in 2016 or later. The bill will also restrict the sale of vaping products to minors (9).
Obesity and diabetes
According to latest estimates from WHO, almost 60% of Russia’s adult population are overweight, and more than one in four (26.5%) is obese (5,22). The prevalence of overweight and obesity in Russia has been increasing over the past three decades. In adults, it is higher among women (56.2% of overweight among males vs. 62.8% in females, and 18.6% of males with obesity vs. 32.9% of females), whereas in childhood, rates are higher among boys (13% of 15-year-old boys and 7% of girls have overweight). The EUROASPIRE IV trial reported 93.1% of the screened population with overweight and 82.1% with obesity (vs. 37.6% obese people in Europe) (31,32). The prevalence of diabetes, particularly type 2 diabetes, is rapidly increasing in most countries in the world especially in Russia. A total of 12,088 thousand adult patients with diabetes were registered in Russia in 2015 (11.1% of adults), and 186,123 deaths in adults were due to diabetes.
The recent economic recovery after 2011 primarily fueled the overweight, obesity and diabetes epidemic in Russia. Similar to energy intake and diet, education and income have been shown to have a strong effect on obesity and BMI. There is an income effect among men in all time periods (1992–2000), with higher-income men consuming more calories, fat, and protein than lower-income men; this effect was not apparent in women except in the proportion of fat and protein intake. High-fat, high cholesterol, low fiber diet due to the low consumption of fruits and vegetables, high consumption of dairy, meat, sugar, and alcohol may have contributed to the high levels of overweight and obesity in Russian adults. With an average BMI in Russia of 26.5 for men and 29.8 for women, both genders exceed the normal range of 18.5–25 and, on average, fall into the overweight category. Overweight and unhealthy nutrition are underlying risk factors for CV diseases, diabetes and cancer, which together with injuries account for 78% of deaths in Russia (5,22,31,32).
Alcohol
The harmful alcohol consumption has been recognized as a major determinant of the male premature mortality in the European republics of the former Soviet Union and Russia (36,37). In the years 1980–2001 alcohol consumption was responsible for 25.6% of CV deaths in men and 15.4% in women in Russia (with 194.4 thousand deaths per year). However, Russia has a positive experience with alcohol regulation. From 1985 until 1987 there was an anti-alcohol campaign, which included higher prices for alcohol products as well as regulation of place and time of sale. As a result, alcohol consumption fell by 20 percent and CV mortality declined with one million secured lives. The recent larger prospective observational study of 151,000 35–74 years old adults residing in Siberia (1999–2008) strongly reinforced the evidence that vodka is a major cause of the high risk of premature death in Russian adults a 20-year risk of death in abusers achieved 50–64% depending on dose). The gradual decline of the average per capita alcohol consumption in terms of the absolute alcohol was marked in Russia in 2008–2014 [16.2 liters per capita per year in 2008, 11.9 liters (12.5 L was a target)—in 2013, and 11.6 liters in 2014 (a target of 12.0 L which is comparable with 12.0 L mostly of wine in France, 11.0 L of mostly beer in Germany, 10.0 L in the United Kingdom, 9.4 L in the Netherlands, and 8.6 L in the U.S. in 2008-2011)] after the monopolization of the alcohol industry by the government in May 2005 with the main objective to fight against the low quality and illegal alcohol which caused a 33% collapse of the alcohol market. A 73% of the Russian alcohol market in 2014 was possessed by the beer consumption, 10%—vodka (with a 1.1% annual decline), 7%—cocktails, 7% wine (mostly, sweet and sparkling wine, from Russia and the former Soviet republics; wine from Georgia and Moldova was partly banned), and 1%—premium alcohol generally with a shortage of the cheap alcohol.
Stress and depression
Stress is a cause of one fourth of the overall mortality increase (38,39). A significant stratification of the population into socioeconomic groups with sharp differences in levels of health has begun in Russia. A study conducted in Vologda oblast in 1999 demonstrated that in the group of people with the most adverse factors, including the lowest income per household member, the likelihood of poor health was 33 times higher than in the most favorable group. Three fourths of the residents were not adapted to new living conditions in the country, 20 percent of respondents experienced frequent stressful situations, 11.7 percent—severe symptoms of anxiety and 9.6 percent—depression. The so called ‘Russian mortality paradox’ among ethnic Russians living in the former Soviet republics and particularly in Kyrgyzstan is the brightest evidence of the detrimental role of the chronic stress and depression which dramatically contribute to the death rates. Cultural practices can have an impact on mortality through two main pathways. The first pathway involves health behavior such as diet, smoking, and alcohol consumption. This health behavior is closely related to the cultural practices and have well established consequences for health and mortality, especially in case of the alcohol abuse and heavy smoking in males. The second pathway involves social support and social integration, which are also related to culture to the extent that individuals’ ability to participate in social networks and derive social, emotional, and material support from these linkages is related to norms and beliefs about family relationships and obligations.
High blood pressure and dyslipidemia
The prevalence of hypertension, one of the most common risk factors for cardiovascular disease (CVD), is estimated at least at 39.7% in the adult population in Russia (vs. 29% in the USA, and about 42.7% in the European region) (5,28,31,32), and has remained relatively stable during the last 10 years with 12,277,489 patients (8,547.3 per 100,000 with a 11.2% 5-year gain) registered with hypertension in 2012 (amongst worst regions there are Tula oblast with 14,829.9 patients per 100,000, Novgorod oblast: 13,570.7; Altai krai: 19,139.0; and Omsk oblast with 14,356.1 patients; the lowest morbidity revealed in the Republic of Adygea with 3,233.8 patients per 100,000; Astrakhan oblast: 2,370.3; and the Republic of Dagestan: 3,922.4). The monitoring system for cholesterol level among Russians doesn’t exist that makes infeasible to estimate burden of dyslipidemia, but 74.9% of the screened Russian population in EUROASPIRE IV trial reported treatment with statin drugs (vs 80.5% in Europe) (31,32). A pharmacoepidemiologic study of hypertensive patients in clinical practices in Russia reported that approximately 26% of hypertensive patients are treated with monotherapy, 37% with two drugs and 37% with three or more drugs. Data on statins use in Russia have a large variability. From 2004 to 2009, use of statins in the population with CHD increased from 10.0% to 85.5% first of all due to broad reforms of the public health system. In another study conducted between 2005 and 2007, only 1.9% of the high-risk patients were taking statins prior to an acute MI. Hence, data suggested that the use of anti-hypertensive and statin drugs for primary CV diseases prevention in the high-risk Russian population was low. Reasons for suboptimal hypertensive and lipid-lowering management in Russia include additional comorbidities (e.g., smoking, left ventricular hypertrophy, obesity, dyslipidemia), poor treatment adherence (patients not taking their medication regularly), and nonadherence (unwillingness to change smoking, dietary, and PA patterns or show up for appointments/ regular check-outs). ‘Therapeutic inertia’ of physicians also contributes to poor management of hypertension and dyslipidemia in Russia. A 7,374,400 patients were managed with prescription of statin drugs in 2011 with approximately 50% adherence to the therapy. At least 6.9 million of CHD patients in Russia were not covered by the lipid-lowering strategy. It means only 6% of patients with dyslipidemia in Russia received the appropriate treatment with statin drugs and might be secured from any life-threatening conditions and death dramatically improving prognosis in this cohort of the Russian population.
Challenges of the national mass screening
The national screening in outpatient centers in 2014 detected 1.6 million people (every 12th citizen) with CV diseases (14,15). The annual mass clinical examination (screening) reveals about 200 thousands every year. The screening exposed ‘new’ patients with chronic lung diseases (every 100th) and more than 100 thousand patients with diabetes mellitus (every 200th). The results of the mass medical examination of the NCD risk factors underlined the significance such challenges as a poor or irrational nutrition—confirmed in 24.3% of the screened population, low PA: 19.6%; smoking: 17.3%; overweight: 16.7%; and abuse of alcohol: 1.8%.
As a result of the clinical examination in 2014, 33% of the population were classified as a health group (a risk group) 1 with a minimum set of diseases and risk factors. About 21% of the screened patients were interpreted as a health group 2 (mostly 40–60 years old males) with a high risk of death and asymptomatic natural history of the chronic diseases. At least 46% of the population required special medical supervision (health group 3). The preventive counseling on healthy lifestyle in 2014 was provided to 200 thousand more people than in 2013 with a total amount of the advised subjects achieving about 7.8 million people in 2013–2014.
Real-world general Russian population in a randomized trial
There is no such a culture in Russia to conduct a general population clinical trials as well as publish it in the English-speaking journals to be transparent for the international scientific community. We failed to find any general population or real world studies especially randomized clinical trials in Russian or English language. All the 3,254 clinical trials registered in ClinicalTrials.Gov are the international studies where very selected populations were enrolled without even a single chance to appreciate the CV burden in Russia. The only clinical trial, a NANOM-FIM trial (17-21), which was conducted by our group at the Ural Institute of Cardiology [a PCI-ready cardiac center with 2,560 angio (21st in Russia of 202 PCI centers) and 1,447 PCI (11th in Russia) with a placement of 1,230 stents a year in 2013] in Yekaterinburg (Russia), has assigned real world patients with CAD and might be a very fine-drawn way to judge the CV health in Russia at least in patients of the Ural region admitted to the PCI-ready cardiac hospital with relatively moderate CV mortality. Yekaterinburg is a 4th largest city in Russia and a capital of the Ural Federal district and administrative center of Sverdlovsk oblast (SVE) with quite developed economics (8th in RIA rating among 83 regions), being a reference of the general Russian population (total mortality by 2016 achieved 14.0 per 1,000, CV mortality—659 per 100,000), and high affordability of hi-tech medical technologies including PCI in 4 PCI centers with 6,233 angios a year [2013], and 2,877 coronary PCI (2,581 stents implanted) annually [2013].
The cohort of Russian patients in NANOM-FIM trial (N=180) was younger (mean age of 51.6 years old with 77.2% of males) if compare with general Western society population or even results of the national mass screening, has had more comorbidities and risk factors (mean BMI of 28.4, current smoking revealed in 70.6% of patients, a 50.6% of alcohol abusers, a 86.7% of patients with hypercholesterolemia), hypertension (a 86.1% of patients) and heart failure (groups in the trial were slightly unbalanced by the number of patients with NYHA III functional class revealed in 32.2% of patients, P=0.039), events of trauma, anamnesis of the smoking and alcohol abuse (more abusers in ferro group, P=0.044) with history of previous PCI (a 13.9% of patients with prevalence in XIENCE V control, P=0.049). Dyslipidemia manifested with the mean LDL cholesterol of 64.7 mg/dL, and HDL cholesterol of 51.4 mg/dL at the check-up moment under the lifelong management with atorvastatin 40 mg or rosuvastatin 40 mg orally daily. Meanwhile, hypertension, previous or simultaneous PCI and heart failure were confirmed as strong independent predictors of cardiac death with high rate of mortality and late thrombosis in patients underwent conventional intervention with the advanced second-generation metallic everolimus-eluting XIENCE V stent.
Trends of invasive strategies in treatment of CAD
In 2013 in Russia there were 202 PCI centers [1.42 PCI centers per million of Russian population (PMRP) with a 6.8% annual growth] with 337 catheterization labs (1.7 cath labs per one PCI center) and 1,023 roentgen endovascular surgeons (interventional/ invasive cardiologists) who implemented 382,223 interventions (1,892.2 interventions per PCI center; 72.0% of them was related to CAD) with a 17.9% increase if compare with 2012 (1,713.9 interventions per PCI center) (11,12). PCI centers treated 2,693 patients PMRP in 2013 with a 18.0% annual gain which was equal to the number of conducted interventions (see Table 1 and Figure 4).
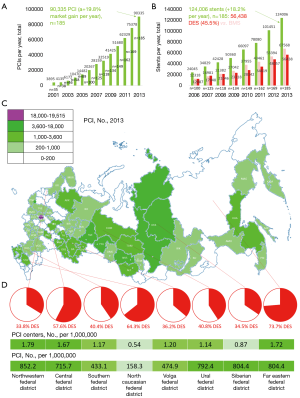
There were 175 Russian PCI centers in 2012 that implemented 205,902 angio, and 75,378 PCI (69.8% of MI, and 31.2% of angina) achieving a level of 531 PCI-interventions PMRP with a placement of 101,451 stents [1.37 stents per PCI; 48,057 of drug-eluting stents (DES)] without correlation (R2=0.0622) between CV mortality and affordability of PCI in the regions mostly due to generally poor access of the population to PCI medical care. In 2013, a positive trend (see Table 1) toward the development of the interventional care (a 9.1% gain) was documented with 191 angio-ready PCI-centers (1.35 PCI centers PMRP) and 243,385 angios (1,715.2 angios PMRP; a transradial access was in 36.7% of cases) with a 0.011% angio-associated mortality, and a placement of 124,006 stents (56,438, or 45.5% of DES; 289.9 interventions PMRP in patients with acute coronary syndrome, and 202.2—in patients with MI versus, for instance, 804 interventions per million of the population in the Netherlands). Russia experienced truly dramatic 16-time enhancement of the angio affordability from 107 PMRP in 2000 up to 1,715 PMRP in 2013. Exactly 90,335 coronary PCI interventions (636.6 coronary PCI PMRP with 1.37 implanted stents per one patient; transradial access—36.9%) were implemented in 185 PCI centers (1.30 PCI centers PMRP) in 2013 with a 19.8% annual growth and a 24-time 13-year increase from 27 coronary interventions PMRP in 2000 to 636 PMRP in 2013 which is significantly lower than in Europe (average 1,871 PMRP in 2013). Only 155 centers were advanced enough to treat chronic total occlusions (CTO), and 127 PCI centers—for left main (LM) with 9,409 successful CTO manipulations, and 1,851 technical complications, but just 1,913 LM interventions. At least 45 PCI centers were ready for intravascular ultrasound (IVUS) (1,632; 1.8% of all PCI), optical coherence tomography (OCT) (773; 0.9% cases) and fractional flow reserve (FFR) (410; 0.5%) in 2013. The valvular heart interventions (transcatheter aortic valve implantation or replacement, TAVI/TAVR) were feasible in 22 PCI centers with 142 placements of aortic valves (transfemoral approach—in 104 cases, and 38—transapical) in 2013 with a 26.5% growth since 2012. Russia has a 5-year experience of such interventions with 353 implanted aortic valves in 26 PCI centers. The number of CABG dramatically increased (see Table 1) from 13,913 in 2007 to 29,214 in 2012 with a 109.9% 5-year gain and general dynamics which was comparable with that of PCI. Thus, despite the positive trends, there is still a backlog of Russia in sense of the affordability of the performing coronary angiography and PCI interventions if compare with the developed European countries and the U.S. It is necessary to make some efforts to raise the number of the performed PCI procedures, improving the security of the Russian population and providing them with the available health benefits.
Cardiovascular health and scientific economics in Russia
The cost of MI and cerebrovascular event care in Russia is estimated at 7.6 billion U.S. dollars or 5.6 billion euros over 10 years (6-10,28,40,41). This represents an annualized cost of MI and cerebrovascular treatment of roughly 0.04% of GDP in 2011. Costs of MI which includes hospitalizations, emergency care, and percutaneous coronary intervention/ cardiosurgery (acute event) have increased from 48,783 rubles (1,178.1 euros) in 2011 up to 209,000 rubles (4,426.1 euros) in 2013 with further decrease to 183,700 rubles (2,688.0 euros) in 2014 despite the reduction of the federal health care budget from 3.7% of GDP in 2013 to a 3.6% GDP in 2014 (2,546.7 billion rubles or 37.3 billion euros: a federal budget contributed 480.8 billion rubles or 18.9%, consolidated budget of the regions—825.8 billions or 32.4%, and insurance system—1,240.1 billion rubles or 48.7%) with the estimated decline down to a 3.0% GDP by 2017 (vs. a 5.4% GDP in E.U., and a 17.1% GDP in the U.S.) which means from 515 billion rubles in 2013 (10.9 billion euros) to 332 billions in 2017 (3.8 billion euros) with a 4.1% decrease of the hospital beds. Follow-up costs, including outpatient visits and medications achieve 10,499 rubles (253.54 euros in 2011) for the first year after MI for patients surviving 30 days after the event. The market of statin drugs in 2011 in Russia was on the level of 4,159,265,369 rubles (100,441,086 euros in 466,077 compliant patients) with a 22.2% annual gain and potential of a 1,388,324,643 euros growth (42). The Russian market of PCI by 2014 achieved 247,540,440 euros (a 19.8% gain per year with the estimated potential of the market development at least up to 3,174,032,411 euros; 7,344,255 CHD patients, 6,878,581 patients with cerebrovascular diseases, and 11,399 patients with indications for a valve surgery (TAVR/TAVI) were registered in 2012 which means a potential volume of the PCI market has a ceiling of 35.9 billion euros) with an average cost of the PCI with stenting of 2,440 euros per procedure.
The official financial data of the Russian ministry of education and science are out of open access, and any details are available exceptionally from the media sources. The bench science generally in Russia according to unofficial pipeline was funded with 130 billion rubles (1.5 billion euros) in 2014 (mostly from federal or regional budgets in absence of the harmonious civilized grant system and an infrastructure for synergistic research collaboration) with a 14.6% decline to 111 billion rubles (to the word, with at least 26.5-fold 5-year boosting of the funds for the military and intelligence objectives) in 2016, but biomedical science was supported only with 21.2 billion rubles (240.8 million euros a year) with increase in output of the Web of Science indexed publications from 25,573 a year in 2003 to 26,503 in 2012. The small growth resulted in a falling world share in Russia from 3% to 2.1% (in clinical medicine 20% below the score world average of citation impact with a decline from a 0.7% global share or 5,946 papers annually to 0.62% or 6,219 manuscripts a year). Russia’s production of highly cited papers over the decade closely resembles the record of India, both in quantity and trend, and like India seems unusually low for a nation with the scientific talent that it possesses most probably due to obvious general poverty of the science and drift of the articles to the Russian-speaking journals which remain uncited (partially cited in the Russian Science Index in cooperation with Thomson Reuters since 2015, but mostly in Russian language; a database of 8.7 million articles from 655 Russian journals published after 2006 which is less than 12.4% of the existing manuscripts) being beyond the international system (43,44). Meanwhile, the Russian biomedical science is not free. Since April 2014 Russian Intelligence officially can proceed with the vetting of any publications via so called ‘Export Publishing Control’ committees at the Universities especially in case of the ‘controlled’ technologies (43,45,46).
The analysis of the Ministry of Health demonstrates that the state-of-the-art biomedical research development in Russia requires a number of the breakthroughs in such fields as genomics and gene engineering, pharmacogenetics and personalized therapy, cell technology, nuclear medicine, nano technology and others with unclear sources of funding, but to the moment Russia has a potential of 447.6 thousand researchers on-board or 11.08 R&D personnel per thousand labor force (2011, MSTI, OECD), and a growing domestic innovation, as measured by RU published patent applications originating from Russia, which is at a substantially higher level than fellow BRIC nations. In European terms, the patenting level falls somewhere between France and Germany and higher than the United Kingdom or Italy. It has grown significantly during the decade to a current level of around 25,000 p.a. with a less than 10% in health sciences despite the economic concerns (6-10,28,40,41).
The economic recession in Russia will be orchestrating the situation in biomedical science at least till 2019. In July 2016, the Russian government deliberated the reduction of the budget for both education and science merely because of the financial deficit amid the deployed international sanctions. The Russian ministry of education and science has an idea to cut a 40% of the budgetary seats for students at the Universities. Furthermore, at least 8,300 scientists will be sacked throughout the country. The budget for science will be shrunk from 0.98% to 0.87% by 2019. Meanwhile, the government thinks how to improve the quality of life for the ‘secured’ scientists enhancing the compensation up to 200 per cent of the regional average achieving at least 12,000–16,000 euros a year (instead of 4,000–8,000 euros annually for today) which is above of the Russian median wage but drastically lower than in the Western countries.
Summary and discussion
The changes in Russian mortality in the last few decades are unprecedented in a modern industrialized country in a peacetime across all the 83 regions, and analysis of the cause of these changes is fundamentally important to understand the link between rapid economic change and health and also to help prevent similar future changes in Russia and other countries in transition. To the word, the CV mortality in Russia alone remains much higher than, if to exemplify, the total mortality in the U.S. Russia’s economy has been hit hard in the past years. The drop in oil prices and sanctions imposed by the west have put the nation into an economic tailspin. GDP growth is negative and trade is on the decline. This is truly important today to understand where Russia is and what to expect in the future with a focus on CV burden.
The socio-economic development in the Russian regions was not directly associated (a M-shaped light correlation) with the rates of CV mortality, but with a weak or moderate correlation with a level of poverty which was relevant to the previous findings (40,41) where the CV mortality was similar in U.S. counties of all income levels. The historic dynamics of the total death rates demonstrates the certain role of the socio-economic disasters for both total and CV mortality, for instance in 90s after the dissolution of the Soviet Union and a default of 1998 (25,28,30), but most probably it makes a sense exceptionally in case of the larger dramatic economic events with the pronounced impoverishment of the population and degradation of the social life with significant changes in a lifestyle which was previously confirmed in both MONICA and HAPIEE studies that observed different populations in the Eastern Europe (1,29,30). The Russian mortality trend documents the dramatic increase of death rates after 1988 at the phase of the Soviet degradation (with a fold GDP decline of −0.36) and the further drop after 2002 with the lowest GDP (PPP) per capita of 8,539.00 U.S. dollars in 1998 growing up to actual $23,292.91 in 2016 amid broad reforms of both the Russian economics and public health system.
The lowest CV mortality was documented in the Russian Caucasus with a lifestyle which is typical for the principles of the Mediterranean diet including higher PA and harmonized nutrition despite relatively poor socio-economic situation at this region. The most remarkable was so called Arctic paradox when very comparable low CV death rates were determined in the subarctic and arctic regions of Russia with extremely cold weather (27) and a lifestyle which is not consistent with the concept of the healthy diet and physical training amid very emerging economic development of the region. The previous Russian studies (47) documented a high strain of the adaptive mechanisms and hemodynamic patterns in Northerners with more reactive vegetative feedback and higher median of blood pressure within the physiologic numbers, which is most probably plays a role of the pre-conditioning for coronary pool and myocardium dramatically reducing a risk of the CV death. We can only speculate about the nature of the Arctic phenomenon, but the only factor we must highlight in the Arctic lifestyle is a high consumption of the seafood. Actually what is truly common in both Mediterranean and Pacific Rim diets is a seafood and grains. Who knows, but may be Japanese health formula which comprises seafood and rice seems to be the most perfect for prevention of CV diseases and related mortality.
The reported with a mass screening (14,15) or a randomized NANOM-FIM trial (17-21) trends of the CV risk factors in Russia are very similar and resembling to the previously released patterns of the CV burden in Russian migrants living in the USA (33). Slavic immigrants report multiple health problems with higher prevalence rates than their counterparts in the U.S. Up to 90% of adult Slavic immigrants are overweight or obese with a low PA, sometimes smoking and abusing alcohol. Many are plagued with CV disease, diabetes, obesity, and depression. Depending on the source, 64–90% report hypertension. Depression rates are reported at 31% and as high as 77% among women.
Obviously, the national mass screening in Russia underestimates the CV burden and existing risk factors due to certain limitations of this approach. Regretfully, such pan-European international cross-sectional studies as EUROASPIRE and particularly EUROASPIRE IV (2015) (31,32) failed to entirely observe the CV burden in the Russian general population mixing results from the specific CHD populations in developed, developing and emerging economies with the different socio-economic situation, condition of the public health system and a lifestyle. Definitely, the larger general population (cross-sectional or prospective) clinical trials are required to ultimately and objectively estimate the trends and dynamics of the CV burden in Russia in the different multi-national (more than 160 ethnic groups) and multi-cultural regions.
The policy makers in the modern-day Russia with very complex economic situation (41) must be concentrated on both a modification of the lifestyle of the population with the optimization of the dietary preferences and PA, and elaboration of the biomedical clinical and scientific systems in order to provide patients with a good quality evidence-based health care. The database of the Russian Ministry of Health should be harmonized with the standardized rates, and accurately collected high quality data from the specific and general populations across Russia strictly within the WHO recommendations in order to grant policy makers with a chance to target and focus resources.
A 27% 10-year decline of CV mortality might be interpreted as a success of the national policy and reforms of the public health system in Russia during last years as well as generally wide efforts of the health professionals on the different levels to tackle CV diseases. However, the inequality of the current CV burden among Russian regions, the high CV mortality if compare with other NCD, along with increases in risk factors for CV diseases, concerns of the invasive service, general poverty of the real clinical practice and biomedical science should raise awareness amongst cardiologists and public health policy makers throughout Russia.
Conclusions
Mortality statistics show the stark reality of a high CV burden in Russia. New national program and aggressive emerging efforts are required to tackle CV diseases in Russia.
Acknowledgments
We appreciate the research assistance, tremendous intellectual contribution and non-profit service of the employees of the Ural Institute of Cardiology (UIC, Yekaterinburg, Russia) and Ural Medical University (UMU, Yekaterinburg, Russia) especially cardiologist-in-chief of the Ural Federal District and Sverdlovsk oblast, member of the Presidium of the Russian Society of Cardiology, chief of the UMU Department of Cardiology, C.E.O. of the UIC Prof. Jan L. Gabinsky, M.D., D.Sc. (UIC, UMU), and a member of the Executive Council of the Russian Society of Cardiology, Deputy C.E.O. of UIC Dr. Marina S. Freydlin, M.D., D.Sc. (UIC).
Funding: AK thanks FP7-IIF Marie-Curie Individual Fellowship program (Grant No. 329728) of the European Commission for support of the DREAM (Development of Bioresorbable Scaffolds and Nanotechnologies for Reversal of Atherosclerosis) project.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 2016;37:3232-45. [Crossref] [PubMed]
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Writing Group Members, Mozaffarian D, Benjamin EJ, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 2016;133:e38-360. [Crossref] [PubMed]
- Ribeiro AL, Duncan BB, Brant LC, et al. Cardiovascular Health in Brazil: Trends and Perspectives. Circulation 2016;133:422-33. [Crossref] [PubMed]
- Petrukhin IS, Lunina EY. Cardiovascular disease risk factors and mortality in Russia: challenges and barriers. Public Health Reviews 2012;33:436-49.
- Oganov RG. Cardiovascular disease at the beginning of the XXI century: medical, social, demographic aspects and ways of prevention. Occupational medicine, regenerative and preventive medicine 2010;11:257-64. Available online: http://federalbook.ru/files/FSZ/soderghanie/Tom%2013/IV/Oganov.pdf
- Babko NV. Orekhovsky PA. Health care reforms in post-Soviet Russia: Past and Future. Society and Economics. 2005;6. (Russian). Available online: http://lab.obninsk.ru/public/articles.php@htmlfile=babko-or-01.htm
- Ascher J, O’Connell S, Urozhaeva Yu. The evolution of the health care system in Russia. McKinsey Herald 2012;25. Available online: http://vestnikmckinsey.ru/healthcare-and-pharmaceuticals/ehvolyuciya-sistemyh-zdravookhraneniya-v-rossii
- Kharlamov A. Is There A Future For Theranostics of Coronary Atherosclerosis in Russia? Herald of Ural Medical University 2015. Available online: https://www.researchgate.net/publication/280941576_Is_There_A_Future_For_Theranostics_of_Coronary_Atherosclerosis_in_Russia?channel=doi&linkId=55cd9b7608aeeaab209b55e6&showFulltext=true
- Kharlamov A. Atheroregression Below Glagov Threshold as New Target of Lipid-Lowering Therapy From Interventional Cardiology Point of View. Available online: https://www.researchgate.net/publication/281094795_Atheroregression_Below_Glagov_Threshold_as_New_Target_of_Lipid-Lowering_Therapy_From_Interventional_Cardiology_Point_of_View?channel=doi&linkId=55d470e908ae0b8f3efa729c&showFulltext=true
- Bokeria LA, Alekyan BG. Roentgenoendovascular diagnostics and treatment of diseases of heart and vessels in Russian Federation – 2013 year. Moscow: Bakulev Research Center of Cardiac Surgery of the Russian Academy of Medical Sciences; 2014. Available online: http://www.bakulev.ru/publish/bcatalog/detail.php?ID=40598
- Bokeria LA. (editor) The Health of Russia; Atlas. 10th edition. Moscow: Bakulev Research Center of Cardiac Surgery of the Russian Academy of Medical Sciences; 2014. Available online: http://www.bakulev.ru/publish/bcatalog/detail.php?ID=40597
- Demography of Russia. Moscow: Russian Federal State Statistics Service (FSSS). Available online: http://www.gks.ru/wps/wcm/connect/rosstat_main/rosstat/ru/statistics/population/demography/#
- Report on the health status and health organizations on the basis of the executive bodies of subjects of the Russian Federation for 2014. Moscow: Russian Ministry of Health (MinHealth), 2015. Available online: http://www.rosminzdrav.ru/ministry/programms/doklad-o-sostoyanii-zdorovya-naseleniya-i-organizatsii-zdravoohraneniya-po-itogam-deyatelnosti-organov-ispolnitelnoy-vlasti-sub-ektov-rossiyskoy-federatsii-za-2014-god
- State report on implementation of the state policy in the sphere of health protection for 2014. Moscow: Russian Ministry of Health (MinHealth), 2015. Available online: http://www.rosminzdrav.ru/ministry/programms/gosudarstvennyy-doklad-o-realizatsii-gosudarstvennoy-politiki-v-sfere-ohrany-zdorovya-za-2014-god
- How to live the Russian regions: the study "RIA Rating". Moscow: RIA news, 2014. Available online: http://ria.ru/infografika/20140522/1008810278.html
- Kharlamov AN, Gabinsky JL. Plasmonic photothermic and stem cell therapy of atherosclerotic plaque as a novel nanotool for angioplasty and artery remodeling. Rejuvenation Res 2012;15:222-30. [Crossref] [PubMed]
- Kharlamov AN, Tyurnina AE, Veselova VS, et al. Silica-gold nanoparticles for atheroprotective management of plaques: results of the NANOM-FIM trial. Nanoscale 2015;7:8003-15. [Crossref] [PubMed]
- Kharlamov AN, Gabinsky JL. Noble metal nanoparticles for plasmonic photothermal therapy of atherosclerosis. Technical Proceedings of the 2013 NSTI Nanotechnology Conference and Expo, NSTI-Nanotech 2013. 2013:369-72.
- Kharlamov AN. Plasmonic photothermal therapy for atheroregression below Glagov threshold. Future Cardiol 2013;9:405-25. [Crossref] [PubMed]
- Kharlamov AN. Why do we fail to achieve Glagovian atheroregression in lipid-lowering trials? Interventional Cardiology 2015;7:469-82. [Crossref]
- European health for all database (HFA-DB). World Health Organization Regional Office for Europe, 2015. Available online: http://data.euro.who.int/hfadb/
- Ovcharova LN. Russian Population in 2016: revenues, expenditures, and social well-being. Monitoring of the Higher School of Economics. Moscow: Higher School of Economics. 2016. Available online: https://isp.hse.ru/data/2016/07/26/1119083176/04_%D0%98%D1%8E%D0%BB%D1%8C_%D0%9C%D0%BE%D0%BD%D0%B8%D1%82%D0%BE%D1%80%D0%B8%D0%BD%D0%B3_%D0%92%D0%A8%D0%AD.pdf
- Kozyreva PM. Bulletin of the Russian Monitoring of the Economic Situation and Health of Population. RLMS-HSE.Moscow: Higher School of Economics, 2011. Available online: https://www.hse.ru/data/2012/08/25/1243030112/Vestnik_RLMS-HSE_2012.pdf
- Men T, Brennan P, Boffetta P, et al. Russian mortality trends for 1991-2001: analysis by cause and region. BMJ 2003;327:964. [Crossref] [PubMed]
- Andreev EM, McKee M, Shkolnikov VM. Health expectancy in the Russian Federation: a new perspective on the health divide in Europe. Bull World Health Organ 2003;81:778-87. [PubMed]
- Fares A. Winter cardiovascular diseases phenomenon. N Am J Med Sci 2013;5:266-79. [Crossref] [PubMed]
- Shum K, Alperin P, Shalnova S, et al. Simulating the impact of improved cardiovascular risk interventions on clinical and economic outcomes in Russia. PLoS One 2014;9:e103280. [Crossref] [PubMed]
- Vikhireva O, Pajak A, Broda G, et al. SCORE performance in Central and Eastern Europe and former Soviet Union: MONICA and HAPIEE results. Eur Heart J 2014;35:571-7. [Crossref] [PubMed]
- Vandenheede H, Vikhireva O, Pikhart H, et al. Socioeconomic inequalities in all-cause mortality in the Czech Republic, Russia, Poland and Lithuania in the 2000s: findings from the HAPIEE Study. J Epidemiol Community Health 2014;68:297-303. [Crossref] [PubMed]
- Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol 2016;23:636-48. [Crossref] [PubMed]
- Pogosova NV, Oganov RG, Boytsov SA, et al. Monitoring of secondary prevention of coronary artery disease in Russia and Europe: results of the Russian part of the international multicenter study EUROASPIRE IV. Kardiologiia 2015;12:99-107. [Crossref]
- Lunze K, Yurasova E, Idrisov B, et al. Food security and nutrition in the Russian Federation - a health policy analysis. Glob Health Action 2015;8:27537. [Crossref] [PubMed]
- Jahns L, Baturin A, Popkin BM. Obesity, diet, and poverty: trends in the Russian transition to market economy. Eur J Clin Nutr 2003;57:1295-302. [Crossref] [PubMed]
- Purath J, Van Son C, Corbett CF. Physical activity: exploring views of older Russian-speaking slavic immigrants. Nurs Res Pract 2011;2011:507829.
- Zaridze D, Lewington S, Boroda A, et al. Alcohol and mortality in Russia: prospective observational study of 151,000 adults. Lancet 2014;383:1465-73. [Crossref] [PubMed]
- Grigoriev P, Andreev EM. The Huge Reduction in Adult Male Mortality in Belarus and Russia: Is It Attributable to Anti-Alcohol Measures? PLoS One 2015;10:e0138021. [Crossref] [PubMed]
- Guillot M, Gavrilova N, Torgasheva L, et al. Divergent paths for adult mortality in Russia and Central Asia: evidence from Kyrgyzstan. PLoS One 2013;8:e75314. [Crossref] [PubMed]
- Guillot M, Gavrilova N, Pudrovska T. Understanding the "Russian mortality paradox" in Central Asia: evidence from Kyrgyzstan. Demography 2011;48:1081-104. [Crossref] [PubMed]
- Spatz ES, Beckman AL, Wang Y, et al. Geographic Variation in Trends and Disparities in Acute Myocardial Infarction Hospitalization and Mortality by Income Levels, 1999-2013. JAMA Cardiol 2016;1:255-265. [Crossref] [PubMed]
- Anna Kontsevaya, PhDcorrespondencePress enter key for correspondence informationemailPress enter key to Email the Kontsevaya A, Kalinina A, Oganov R, et al. Economic Burden of Cardiovascular Diseases in the Russian Federation. Value in health regional issues 2013;2:199-204.
- Pugach IM. Analysis of consumption of statins in Russia in 2010-2011 years. Good Clinical Practice 2012;2:56-62.
- Kharlamov A. View point - Russian science through the prism of Intelligence - is fraud still possible. Eur Heart J 2013.
- Winning A. The Research & innovation performance of the G20 and its impact on decisions made by the world’s most influential economic leaders. Reuters 2014. Available online: http://sciencewatch.com/sites/sw/files/images/basic/research-innovation-g20.pdf
- Schiermeier Q. Russian secret service to vet research papers. Nature 2015;526:486. [Crossref] [PubMed]
- Kondrashov F. Russia's crackdowns are jeopardizing its science. Nature 2015;523:383. [Crossref] [PubMed]
- Solonin YuG, Markov AL, Bojko ER, et al. Comparison of the results of pre-nosological studies of “Mars-500” experiment participants in Syktyvkar and Yekaterinburg. News of the Komi Research Center of the Ural Division of the Russian Academy of Sciences 2013;1:50-5.


