Grading aortic stenosis severity when the flow modifies the gradientvalve area correlation
Valvular aortic stenosis (AS) is the most frequent valvular disease in developed countries. The diagnosis of AS is classically confirmed by echocardiography, the standard tool for detecting and assessing the severity of the disease (1). Nevertheless, assessment of AS severity is still challenging. Severe AS is usually defined as mean gradient >40 mmHg, aortic valve area (AVA) <1 cm2 and peak aortic jet velocity >4.0 m/s (2). However, discrepancies are frequently observed between the mean gradient and the valve area in a single patient (3). These discrepancies are easy to understand in patients with low cardiac output secondary to reduced LV ejection fraction, but also may occur in patients with apparently preserved LV function (4). In daily practice, they may potentially lead to an underestimation of stenosis and symptom severity and thus to inappropriate delay of aortic valve replacement (AVR), which may, in turn, have a negative impact on patient outcome (5-7). In this issue of Cardiovascular Diagnosis and Therapy, OZKAN has elegantly reviewed the concept of low gradient AS in patients with preserved LV function (8).
New aortic stenosis grading classification
Recently, several authors have reported that under the same denomination of severe AS (AVA <1 cm2), several entities may be identified which differ in terms of transvalvular flow rates and pressure gradients develop (9-11). The first to underline the importance of integrating the valve-gradient relationship to the flow pattern was the group of Pibarot et al. (5), whereas Miners et al. (3) were the first to clearly show the inconsistencies for grading the severity of AS and to propose with Dumesnil et al. (6) the new classification of AS. In patients with an AVA <1 cm2, four flow-gradient AS categories can be identified: normal flow/low gradient (NF/LG), normal flow/high gradient (NF/HG), low flow/high gradient (LF/HG) and low flow/low gradient (LF/LG). LF is defined as an indexed LV stroke volume <35 mL/m2 and LG as a mean trans-aortic pressure gradient <40 mmHg (12).
Normal flow-low gradient
This pattern is observed in 31-38% of patients and seems to identify a group of patients with a less severe degree of AS-inherent inconsistency contained in the guidelines-or who has been exposed to the disease for a shorter period of time. This entity is characterized by a preserved LV longitudinal myocardial function, resulting in lower BNP level and Monin’s risk score (12,13). The prognosis of these patients seems to be relatively preserved as compared with the other categories.
Normal flow-high gradient
This pattern represents the most prevalent entity (39-72%) and is fully consistent with the criteria proposed by the guidelines (4,5,12). When compared with NF/LG group, although the LV longitudinal function is preserved, the BNP is higher and the cardiac event-free survival rate of NF/HG is reduced. Furthermore, patients with NF/HG seem to have more severe AS suggesting a longer exposition to this progressive disease. When symptomatic, these patients are classically referred for AVR, whereas when asymptomatic, the management of these patients underlines the need for optimized risk stratification.
Low flow-high gradient
This pattern accounts for 8% of patients with severe AS (4,12). It is characterized by an indexed LV stroke volume <35 mL/m2 in spite of preserved LV ejection fraction, a high BNP level and Monin’s risk score and a significant reduction in LV longitudinal function (14). Of note, LV ejection fraction is a crude estimate of LV systolic function. LV ejection fraction is influenced by both intrinsic myocardial function and LV cavity geometry. Hence, for a similar extent of intrinsic myocardial shortening, the LV ejection fraction will tend to increase in relation to the extent of LV concentric remodelling. The LV ejection fraction may therefore markedly underestimate the extent of myocardial impairment in the presence of LV concentric remodelling such as is generally the case in AS patients. Hence, what is normal for an LV with normal geometry may be abnormal for a LV with concentric remodelling. Moreover, the reduction in LV output (related to intrinsic myocardial dysfunction and significant LV remodelling) may, in turn, result in lower than expected trans-valvular gradients. The outcome of these patients is nearly identical to patients with NF/HG. When symptomatic, these patients tend to have a better survival if treated surgically.
Low flow-low gradient
The prevalence of LF/LG pattern seems to be lower than what initially reported. This entity accounts for 7% in asymptomatic patients and up to 15-35% in symptomatic patients (4-6,12,14). This pattern, namely paradoxical low-flow AS, represents a challenging clinical entity that has been recently emphasized. It is associated with more pronounced LV concentric remodelling, smaller LV cavity, increased global LV afterload, intrinsic myocardial dysfunction, myocardial fibrosis and a dismal prognosis (12,15). In asymptomatic patients, we have shown that the likelihood of remaining alive without AVR at 3 years was 5-fold lower than for the NF/LG pattern and 4.3-fold higher than in the NF/HG group (12). This clinical entity is often misdiagnosed, which may lead to an underestimation of AS severity and thereby to underutilization or inappropriate delay of surgery. It is important to recognize this entity in order not to deny surgery to a symptomatic patient with small AVA and LG.
Discordance between gradient and valve area
Potential causes of discordance between AVA and gradient in patients with preserved LV ejection fraction include (I) measurement errors; (II) small body size; (III) paradoxical low flow AS; and (IV) inconsistent grading related to intrinsic discrepancies in guidelines criteria (4,6,7,10,11). First of all, patients with small body size and LV dimensions may exhibit a lower trans-valvular pressure gradient because of a lower albeit normal stroke volume. Secondly, the stroke volume and therefore the AVA may be underestimated because of underestimation of LV outflow tract and/or misplacement of pulsed-wave Doppler sample volume. Several methods can be used to corroborate the Doppler-echocardiographic measurements of stroke volume and AVA. For example, in the absence of significant mitral regurgitation, the stroke volume can easily be estimated by the Simpson’s method (volumetric method to measure LV ejection fraction and volumes). If the stroke volume measured by these independent methods is consistent with the stroke volume measured in the LV outflow tract, one can be reassured about the accuracy of the measurement of stroke volume. Third, paradoxical LF/LG represents a new entity in which the LF state results from both LV concentric remodelling and reduced subendocardial longitudinal function. This outlines the absence of erroneous estimation of AS severity. Fourth, in some cases, discrepancy in gradient-valve area relationship may be related to inconsistencies in current guidelines. A harmonization of the definition of severe AS may reclassify some of these patients with “severe” AS into “moderate” AS. When one combines the current prospective clinical data with earlier hemodynamic echo and invasive data, it seems that a gradient of 40 mmHg fits more with a valve area of 0.8 cm2 whereas a valve area of 1 cm2 relates to a mean gradient of 26 mmHg (3,6,16). Furthermore, when there is a discordance between the valve area (in the severe range) and the gradient (in the moderate range) in patients with preserved LV ejection fraction, a more comprehensive Doppler echocardiographic evaluation and potentially other diagnostic tests (BNP, Calcium score by multislice computed tomography, exercise/dobutamine stress echocardiography) may be required to confirm disease severity and guide therapeutic management.
Clinical implications and management
In daily practice, the assessment of AS severity should integrate the flow-gradient pattern to the classic measurement of AVA. As a general rule, a low trans-valvular gradient (<40 mmHg) or velocity (<4 m/s) does not exclude the presence of a severe AS in patients with small AVA and preserved LV ejection fraction. In addition, a preserved LV ejection fraction (>50%) does not exclude the presence of myocardial systolic dysfunction and low trans-valvular flow in AS. Patients with NF/LG AS classically have no or minimal subendocardial dysfunction and a relatively preserved outcome. In this NF/LG category, indication for AVR should be restricted to patients in whom symptoms can clearly be attributed to AS. In the NF/HG category, AVR (surgical or percutaneous) is the only therapy to significantly improve both survival and symptoms. When asymptomatic, individual risk stratification can help identify patients who may benefit from early surgery. In the other categories, the LF state represents a witness of intrinsic myocardial dysfunction and a more advanced disease process. Symptomatic patients with LF/HG should also benefit from prompt AVR. When asymptomatic, individual risk stratification should also be encouraged. Exercise echocardiography may be of interest by unmasking patients with limited valve compliance and/or exhausted LV contractile reserve (17,18). Paradoxical LF/LG conveys a poor outcome even in asymptomatic patients. In this category, though the benefit of surgery is not proven, AVR may probably be beneficial in selected symptomatic patients (7,19,20) (Table 1). In clinical practice, ascertaining this entity is challenging. Before considering surgery, symptoms should be matched to the severity of AS. In low risk patients, AVR may be advocated. In high-risk patients, additional outcome studies are needed to determine the most appropriate modality and timing of treatment.
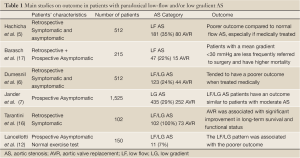
Full Table
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lancellotti P, Donal E, Magne J, et al. Risk stratification in asymptomatic moderate to severe aortic stenosis: the importance of the valvular, arterial and ventricular interplay. Heart 2010;96:1364-71.
- Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation 2006;114:e84-231.
- Minners J, Allgeier M, Gohlke-Baerwolf C, et al. Inconsistent grading of aortic valve stenosis by current guidelines: haemodynamic studies in patients with apparently normal left ventricular function. Heart 2010;96:1463-8.
- Adda J, Mielot C, Giorgi R, et al. Low-Flow, Low-Gradient Severe Aortic Stenosis Despite Normal Ejection Fraction Is Associated With Severe Left Ventricular Dysfunction as Assessed by Speckle-Tracking Echocardiography: A Multicenter Study. Circ Cardiovasc Imaging 2012;5:27-35.
- Hachicha Z, Dumesnil JG, Bogaty P, et al. Paradoxical low-flow, low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 2007;115:2856-64.
- Dumesnil JG, Pibarot P, Carabello B. Paradoxical low flow and/or low gradient severe aortic stenosis despite preserved left ventricular ejection fraction: implications for diagnosis and treatment. Eur Heart J 2010;31:281-9.
- Jander N, Minners J, Holme I, et al. Outcome of patients with low-gradient "severe" aortic stenosis and preserved ejection fraction. Circulation 2011;123:887-95.
- Ozkan A. Low gradient "severe" aortic stenosis with preserved left ventricular ejection fraction. Cardiovasc Diagn Ther 2012;2:19-27.
- Dumesnil JG, Pibarot P, Akins C. New approaches to quantifying aortic stenosis severity. Curr Cardiol Rep 2008;10:91-7.
- Pibarot P, Dumesnil JG. Assessment of aortic stenosis severity: when the gradient does not fit with the valve area. Heart 2010;96:1431-3.
- Lancellotti P, Magne J. Valvuloarterial impedance in aortic stenosis: look at the load, but do not forget the flow. Eur J Echocardiogr 2011;12:354-7.
- Lancellotti P, Magne J, Donal E, et al. Clinical outcome in asymptomatic severe aortic stenosis insights from the new proposed aortic stenosis grading classification. J Am Coll Cardiol 2012;59:235-43.
- Monin JL, Lancellotti P, Monchi M, et al. Risk score for predicting outcome in patients with asymptomatic aortic stenosis. Circulation 2009;120:69-75.
- Lancellotti P, Donal E, Magne J, et al. Impact of global left ventricular afterload on left ventricular function in asymptomatic severe aortic stenosis: a two-dimensional speckle-tracking study. Eur J Echocardiogr 2010;11:537-43.
- Herrmann S, Störk S, Niemann M, et al. Low-gradient aortic valve stenosis myocardial fibrosis and its influence on function and outcome. J Am Coll Cardiol 2011;58:402-12.
- Zoghbi WA. Low-gradient "severe" aortic stenosis with normal systolic function: time to refine the guidelines? Circulation 2011;123:838-40.
- Lancellotti P, Lebois F, Simon M, et al. Prognostic importance of quantitative exercise Doppler echocardiography in asymptomatic valvular aortic stenosis. Circulation 2005;112:I377-82.
- Maréchaux S, Hachicha Z, Bellouin A, et al. Usefulness of exercise-stress echocardiography for risk stratification of true asymptomatic patients with aortic valve stenosis. Eur Heart J 2010;31:1390-7.
- Tarantini G, Covolo E, Razzolini R, et al. Valve replacement for severe aortic stenosis with low transvalvular gradient and left ventricular ejection fraction exceeding 0.50. Ann Thorac Surg 2011;91:1808-15.
- Barasch E, Fan D, Chukwu EO, et al. Severe isolated aortic stenosis with normal left ventricular systolic function and low transvalvular gradients: pathophysiologic and prognostic insights. J Heart Valve Dis 2008;17:81-8.


