Coronary CT angiography with prospective ECG-triggering: an effective alternative to invasive coronary angiography
Introduction
Over the last decade a great deal of interest has been focused on imaging and diagnosis of coronary artery disease (CAD) using coronary CT angiography due to its less invasive nature and improved spatial and temporal resolution. Moderate to high diagnostic accuracy was achieved with 64- or more slice CT, owing to further technical improvements (1-5). These studies have indicated that coronary CT angiography has high accuracy for the diagnosis of CAD and could be used as an effective alternative to invasive coronary angiography in selected patients. However, coronary CT angiography has the disadvantage of high radiation dose which raises concerns for both clinicians and manufacturers. This is reflected in the changing research directions from the early research focus on the diagnostic value of coronary CT angiography in CAD to the increasingly reported studies on dose reduction (6).
Radiation dose is becoming a major issue for coronary CT angiography, since 64- or more-slice CT shows improved and promising results in the diagnosis of CAD (7-10). It is estimated that in daily practice, effective dose of coronary CT angiography may reach up to 40 mSv in female patients if no dose-saving strategies are applied, and this is associated with radiation exposure to breast tissues (11). The radiation risks associated with coronary CT angiography have become a hot topic of debate in the literature (12-14). The general view about radiation dose is that CT is associated with a risk of cancer development. Therefore, coronary CT angiography should be performed with dose-saving strategies whenever possible to reduce the radiation dose to patients.
Of various dose-saving strategies used in coronary CT angiography (11,15,16), prospective ECG-triggered scanning represents one of the most promising radiation saving techniques with a significant reduction of radiation dose when compared to the retrospective ECG-gating and invasive coronary angiography (17-19). Early studies demonstrated the feasibility of prospective ECG-triggering and later reports confirmed that diagnostic images could be acquired with this new technique while achieving reduction of the effective dose by up to 90% (20-23). It has been reported that the effective dose of prospective ECG-triggered coronary CT angiography is comparable to or even lower than that of invasive coronary angiography (20-27). Since prospective ECG-triggered coronary CT angiography shows promising results in the diagnosis of CAD with resultant very low effective dose, we expect that more and more studies will be conducted with this technique in cardiac imaging. It is critical to develop methods that reduce radiation dose without compromising image quality when choosing coronary CT angiography as the main diagnostic modality in cardiac imaging. The purpose of this paper is to provide an overview of coronary CT angiography with use of prospective ECG-triggering with focus on the imaging protocols, diagnostic accuracy and radiation dose when compared to traditional retrospective ECG-gating. Future directions on prospective ECG-triggered coronary CT angiography are highlighted. It is expected that this paper will provide readers with a good understanding of the current status of prospective ECG-triggering in the diagnostic applications of coronary artery disease.
Ospective ECG-triggering-general technical requirements
Prospective ECG-triggering with non-helical scan was used a long time ago with electron-beam CT for calcium scoring; however, it was recommended recently for multislice CT cardiac imaging, and this imaging protocol is increasingly being reported in the literature due to its resultant very low radiation dose (17-27).
Prospective ECG-triggered coronary CT angiography uses the partial-scan technique to the motion of the heart, which is defined as the step-and-shoot method, so that scan is triggered by ECG signal instead of spiral CT acquisition. This technique allows data to be acquired in a certain phase of cardiac cycle, preferably in the mid-diastolic phase, when cardiac motion is minimal.
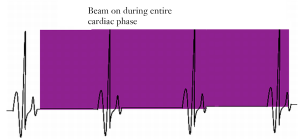
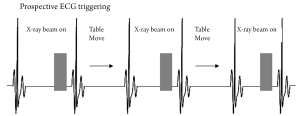
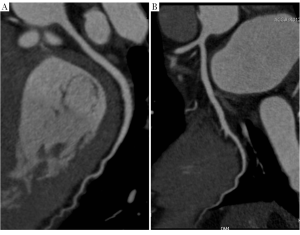
The principle of prospective ECG-triggering is that data acquisition only takes place in the selected cardiac phase by selectively only turning on the x-ray tube when triggered by the ECG signal, and turning it off or dramatically lowering it during the rest of the R-R cycle (Figure 1). This contrasts significantly to the retrospective ECG-gated coronary CT angiography, which acquires the volume data during spiral scanning at a very low pitch (0.2-0.5) so as to produce volume coverage without gaps in each phase of the cardiac cycle with multiple overlapping regions (Figure 2). Prospective triggering is also referred to as sequential data acquisition with an effective pitch of 1.0. The main advantage of this scanning protocol is the very low radiation dose as the x-ray exposure time is short. Most importantly, this prospective ECG-triggered method is still accurate in diagnosing coronary artery disease. However, it suffers from several limitations.
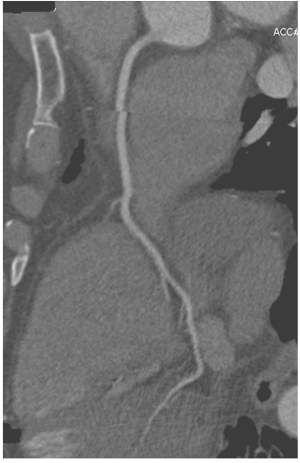
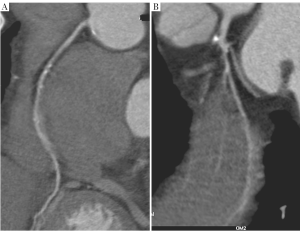
First, it is limited to heart rate less than 70 or 65 beats per minute (bpm). Estimation of the next R-R interval may be incorrect when heart rate changes are present such as arrhythmia (28). Second, ECG-triggered sequential scan is usually restricted to scanning with non-overlapping adjacent slices, or slice increments with only small overlap. The scan time to cover the heart volume is thus directly proportional to the slice increment. Consequently, prospective ECG-triggering puts high demand on the z-axis coverage, therefore, it is normally performed with 64-slice or more slice scanners. Presence of misalignment due to acquisition of images in 4-5 heart beats to cover the entire heart with 64-slice CT is an example of this limitation (Figure 3). This can be overcome with the latest 320-slice CT scanner, which enables coverage of the cardiac volume in a single heartbeat. Last, cardiac images are acquired during only a small portion of the R-R interval as ECG-triggered acquisition targets only a specific phase of the cardiac cycle; thus, functional information about cardiac valve or ventricular wall motion is not available (17,27).
Prospective ECG-triggering can also be performed with high-pitch spiral scan which is a new type of spiral acquisition developed specifically for dual-source CT (DSCT) scanner, Siemens Definition Flash. This scanning protocol enables acquisition of 128 slices simultaneously (flying focal spot) (29-31). The pitch can be increased substantially while still allowing image reconstruction due to dual-source geometry. Overlapping radiation dose is avoided, thus substantially reducing the effective radiation dose to the patient. According to Achenbach and Alkadhi’s reports, a very high pitch value (up to 3.4) was used to cover the volume of the heart in a very short (approximately 0.260 s), enabling acquisition of complete data in a single cardiac cycle with excellent image quality at a consistent dose lower than 1.0 mSv (29,31). Thus, high-pitch spiral cardiac CT angiography seems to be very attractive in the future due to its very low dose.
Radiation dosemeasurements in prospective ECG-triggering
Radiation dose estimates for coronary CT angiography are best expressed as volume CT dose index (CTDIvol), dose-length product (DLP), and effective dose. These parameters are accurately defined and allow comparisons of the radiation doses of various cardiac CT imaging protocols. Clinicians referring for performing coronary CT angiography should fully understand the radiation doses associated with various CT scanning protocols. This may aid in making decisions as to whether a cardiac CT examination is medically justified and which protocol addresses the clinical question properly with the least radiation exposure to patients (32).
Dose-length product
The DLP is an indicator of the integrated radiation dose of an entire CT examination. DLP increases with an increase in total scan length or variables that affect the CTDIvol (tube voltage or tube current or pitch). A recent systematic review of coronary CT angiography with use of prospective ECG-triggering versus retrospective gating shows that in characterising a cardiac CT study, DLP is a more objective physics metric than effective dose (33). The variability of DLP between different study sites observed in that review was striking, as the DLP reported in the studies ranged from 129 to 337 mGy cm. Median DLP at the highest dose sites was more than 3 times that at the lowest dose sites. Thus, coronary CT angiography may be associated with significantly higher or lower dose than invasive coronary angiography, depending on how CT angiography is performed at a study site. The DLP represents most closely the radiation dose received by an individual patient and may be used to set reference values for a given type of CT examination to help ensure patient doses at CT are as low as reasonably achievable. It is recommended that DLP should be recorded for each study and serve as the cornerstone of quality assurance efforts (34).
Effective dose
Effective dose is a single parameter used to reflect the relative risk from exposure to ionizing radiation. The calculation of the effective dose in the current literature is based on a method proposed by the European Working Group for Guidelines on Quality Criteria in CT (35), deriving radiation dose estimates from the product of the DLP and an organ weighting factor for the chest as the investigated anatomic region (k=0.014 or 0.017 mSv· mGy-1·cm-1) averaged between male and female models from Monte Carlo simulations (36).
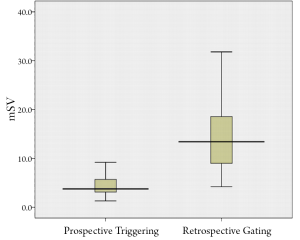
According to a number of systematic review and meta-analysis reports, the mean effective radiation dose for prospective ECG-triggered coronary CT angiography in patients with a low and regular heart rate ranges from 2.7 to 4.5 mSv (33,37,38), which is significantly lower than that for retrospective ECG-gated coronary CT angiography (Figure 4). Further reduction of radiation dose can be achieved in prospective ECG-triggered coronary CT angiography with use of lower kVp values and high-pitch mode. A reduction of effective dose by up to 55% has been reported in prospective ECG-triggering with application of 80 and 100 kVp without compromising image quality (33,38). Therefore, a combination of prospective ECG-triggering with a low kVp protocol should be recommended in patients with body mass index (BMI) less than 25 kg/m2, since changing tube voltage needs to be correlated with the patient's BMI.
The prospective ECG-triggered high-pitch mode further and significantly lowers the radiation dose to less than 1 mSv while maintaining the image quality and high diagnostic performance, as reported in some studies (29-31). This technique can only be achieved with the second generation of DSCT as it requires high temporal resolution to allow single cardiac cycle reconstruction without motion artefacts. For the high-pitch mode, only patients with a low and stable heart rate (<65 bpm) and BMI <30 kg/m2 are eligible to accommodate the long image acquisition window and allow accurate triggering of the image acquisition process. Both high and irregular heart rates preclude the use of high-pitch coronary CT angiography because inconstant heart rates would compromise image quality by causing data acquisition in an unfavourable segment of the cardiac cycle. In addition, the broader detector width of 128-slice scanner reduces the misalignment artefacts that are observed in 64-slice CT scanners.
Diagnostic value of prospective ECG-triggering at low heart rate
A significant dose reduction has been reported in several studies performed with prospective ECG-triggered coronary CT angiography (39-41), however, diagnostic value of prospective ECG triggering in the assessment of coronary arteries or CAD has not been systematically studied. Achieving high diagnostic accuracy with prospective ECG-triggering is essential to ensure that this scanning technique can be reliably used as an alternative to high-dose retrospective ECG-gating or invasive coronary angiography in the diagnosis of CAD.
Assessable coronary segments and image quality evaluation
Most of the studies performed with prospective ECG-triggered coronary CT angiography that are available in the literature focus on the assessment of coronary artery segments and image quality evaluation, in addition to the reduction of radiation dose. The mean assessable segments for prospective ECG-triggered coronary CT angiography were more than 97% (Figure 5), which are comparable to those for retrospective ECG-gated scans, according to recent analyses. On average, less than 3% of the coronary segments were reported to be non-diagnostic image quality in prospective ECG-triggered scans (37,38).
It is well known that the high-density calcification produces blooming artefacts, which lead to overestimation of the degree of coronary stenosis, thus affecting the assessment of coronary segments and resulting in low positive predictive value. Although it has been reported that the rate of nondiagnostic segments in patients with a higher calcium score was significantly higher than the rate of nondiagnostic segments in patients with a lower calcium score (42), the diagnostic accuracy was not affected in patients with higher calcium loads (38).
Qualitative assessment of image quality was normally performed by a likert-scale point score system (3 to 5-point ranking scale) in most of the studies, while quantitative assessment of image quality with use of signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) was only reported in a few studies (33). Although image noise (standard deviation) was slightly increased in prospective ECG-triggered coronary CT angiography when compared to that measured in retrospective gated scans, there is no significant difference in SNR and CNR between the two groups (33).
Diagnostic accuracy
Information about diagnostic value of prospective ECG-triggered coronary CT angiography in CAD is limited, as the majority of currently available studies focus on reduction of radiation dose with acceptable diagnostic images. Two meta-analyses of studies on the use of prospective ECG-triggered 64-or more slice coronary CT angiography reported that the mean patient-based sensitivities and specificities ranged from 99% to 100%, and 89% to 91%, respectively (37,38). The vessel- and segment-based estimates showed lower sensitivities and higher specificities, which ranged from 95% to 97% and 93% to 95%; 91% to 92% and 96% to 97%, respectively. Early evidence indicates that coronary CT angiography with prospective ECG-triggering has high sensitivity and good specificity for the diagnosis of significant CAD. The very high negative predictive value of prospective ECG-triggered coronary CT angiography with low radiation dose suggests that this imaging technique can be used as a reliable test for ruling out CAD.
Based on the individual studies and meta-analyses, it can be concluded that for the group of patients with a low and regular heart rate (less than 70 bpm) examined to date with coronary CT angiography, use of a prospectively triggered scan has not been shown to change patient-based, vessel-based and segment-based sensitivity or specificity when compared to the existing data for retrospectively gated exams (1-5).
Radiation dose of prospective ECG-triggering at high heart rate
It is an essential step to control patients’ heart rate to 70 bpm or lower in coronary CT angiography using prospective ECG-triggering in order to guarantee image quality and low effective dose, as shown in previous studies (17-27). In patients with high or irregular heart rate, higher radiation dose has been reported in studies due to the use of padding (43-45).
The purpose of adding padding (additional surrounding X-ray beam on time) is to provide additional phase information to compensate for variations in heart rate by adding time before and after the centre phase of the acquisition. Padding is described in the range of 0-200 ms and is added to both sides of the centre of the acquisition with padding 0 corresponding to a window of 100 ms scanning time and padding 100 corresponding to a window of 200 ms scanning time. Padding is generally used when the heart rates are more than 65bpm or when there is apparent heart rate variability (heart rate variation is more than 10 bpm) (33). LaBounty et al. in their recently published large multicentre study showed that the use of minimal padding was associated with substantial reduction in radiation dose with preserved image interpretability (46). Use of no or reduced padding should be considered in dose-saving strategies. Freeman et al. in their prospective study consisting of 2025 patients undergoing prospective ECG-triggered 64-slice coronary CT angiography reported that the mean effective dose was 2.75 mSv in patients without use of padding, while the mean effective dose was increased to 5.88 mSv in patients studied with padding (44). Similarly, Hoe and Toh in their study performed with 320-slice CT coronary angiography showed that radiation dose has been significantly increased in patients with heart rate>65 bpm or irregular heart rate when compared to the low heart rate group (45). The mean effective was 5.7 mSv in patients scanned by one-heart beat protocol, but the dose was increased to 13.0 and 17.5 mSv in patients scanned by two- and three-heart beat protocols, respectively. Modification of the prospective ECG-triggered protocols is necessary to enable further dose reduction in these patients with high or irregular heart rate.
DSCT coronary angiography shows promise in examining patients with different heart rate. Few data are available to show the diagnostic value of DSCT coronary angiography with use of prospective ECG-triggering. Sun et al. investigated the diagnostic performance of DSCT prospective ECG-triggered coronary angiography in patients with low to high heart rate, and their results showed no significant difference among low, medium and high heart rate groups in terms of diagnostic image quality, and mean effective dose (43). Despite encouraging results, patients with irregular heart rate or heart rate more than 90 bpm were excluded from their study due to potential failure or unpredictable image quality (Figure 6). Xu et al. explored feasibility of DSCT prospective ECG-triggered coronary CT angiography in patients with heart rate higher than 70 bpm, and their results indicated that prospective ECG-triggering is feasible in patients with a heart rate between 70 and 110 bpm with excellent depiction of coronary segments and 57% dose reduction compared to retrospective gating (47). The second generation of DSCT system with capability of achieving 75 ms temporal resolution could be a promising solution for patients with irregular or high heart rate with use of prospective ECG-triggering technique.
Current status and future directions
Current available data indicate that achieving low-dose coronary CT angiography using prospective ECG-triggering is feasible in an everyday population but requires the use of strict exclusion criteria and careful patient preparation (44,48). Heart rate control is crucial for performing a successful coronary CT angiography with prospective ECG-triggering with use of either 64- or 128- or 320-slice scanners (20-24,44,49-52). A regular heart rate control of less than 70 bpm is achieved through oral or intravenous administration of β-blockers, and this is conducted in almost all of currently available reports. This may result in the exclusion of patients who do not respond or have known contraindications to β-blockers. DSCT coronary angiography offers potential opportunities for inclusion of patients with different heart rate, although more studies are needed to confirm the diagnostic value and image quality.
The tissue weightings of estimating the effective dose of prospective ECG-triggered coronary CT angiography are derived from the International Commission on Radiological Protection (ICRP) which focuses on all aspects of protection from ionizing radiation. In 2007, ICRP released the 103 publication updating the 16-year old ICRP 60 dataset, following the latest available scientific information of the biology and physics of radiation exposure, particularly the tissue weighting for breast tissue has increased from 0.05 to 0.12 (53). The conversion factor used to calculate effective dose from coronary CT angiography has been upgraded from 0.014 to 0.028, thus, doses from coronary CT angiography could be significantly underestimated due to failure of using a cardiac specific conversion factor in the recent ICRP documentation (54,55). Gosling et al. compared the effective dose using the latest ICRP 103 tissue-weighting factors with that calculated with previously published chest conversion factors (54). Their results showed that the use of chest conversion factors (0.014-0.017) significantly underestimated the effective dose when compared to the dose calculated using the conversion factor of 0.028. A conversion factor of 0.028 would give a better estimation of the effective dose from prospectively ECG-triggered coronary CT angiography. Appropriate conversion factors are needed to accurately estimate effective dose. A conversion factor of 0.014 or 0.017 is commonly used in many cardiac CT studies to estimate the effective dose associated with coronary CT angiography, thus, this could lead to variations in the reported effective dose. As a result, the DLP or CTDIvol is recommended to compare the radiation exposure of coronary CT angiography (33).
Most of the current studies on prospective ECG-triggering are performed by the same expert groups at a single academic centre, thus, further studies at multiple centres are needed before widespread implementation of this technique can be recommended.
Summary and conclusions
There is sufficient evidence to confirm that coronary CT angiography with prospective ECG-triggering results in high diagnostic image quality and is associated with a low radiation dose. Prospective ECG-triggered coronary CT angiography is regarded as a reliable alternative to retrospective ECG-gated coronary CT angiography in the assessment of coronary arteries in patients with a regular and low heart rate. It is important to note that the current effective doses from prospective ECG-triggered coronary CT angiography are at the same level or even lower than those acquired from invasive coronary angiography. Therefore, according to the currently available data in the literature, the achievements in radiation dose reduction in coronary CT angiography have been tremendous. Further studies based on large cohorts with inclusion of patients with different heart rate, and with focus on the diagnostic value are needed to confirm its clinical accuracy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Sun Z, Lin C, Davidson R, et al. Diagnostic value of 64-slice CT angiography in coronary artery disease: a systematic review. Eur J Radiol 2008;67:78-84.
- Vanhoenacker PK, Heijenbrok-Kal MH, Van Heste R, et al. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. Radiology 2007;244:419-28.
- Abdulla J, Abildstrom SZ, Gotzsche O, et al. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J 2007;28:3042-50.
- Mowatt G, Cook JA, Hillis GS, et al. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart 2008;94:1386-93.
- Stein PD, Yaekoub AY, Matta F, et al. 64-slice CT for diagnosis of coronary artery disease: a systematic review. Am J Med 2008;121:715-25.
- Sun Z, Ng KH. Coronary computed tomography angiography in coronary artery disease. World J Cardiol 2011;3:303-10.
- Raff GL, Gallagher MJ, O'Neill WW, et al. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 2005;46:552-7.
- Chao SP, Law WY, Kuo CJ, et al. The diagnostic accuracy of 256-row computed tomographic angiography compared with invasive coronary angiography in patients with suspected coronary artery disease. Eur Heart J 2010;31:1916-23.
- Rybicki FJ, Otero HJ, Steigner ML, et al. Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 2008;24:535-46.
- Dewey M, Zimmermann E, Deissenrieder F, et al. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 2009;120:867-75.
- Paul JF, Abada HT. Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 2007;17:2028-37.
- Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med 2007;357:2277-84.
- Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA 2009;301:500-7.
- Raff GL, Chinnaiyan KM, Share DA, et al. Radiation dose from cardiac computed tomography before and after implementation of radiation dose-reduction techniques. JAMA 2009;301:2340-8.
- Sun Z, Ng KH. Multislice CT angiography in cardiac imaging. Part III: radiation risk and dose reduction. Singapore Med J 2010;51:374-80.
- Sun Z, Choo GH, Ng KH. Coronary CT angiography: current status and continuing challenges. Br J Radiol 2012;85:495-510.
- Husmann L, Valenta I, Gaemperli O, et al. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J 2008;29:191-7.
- Herzog BA, Wyss CA, Husmann L, et al. First head-to-head comparison of effective radiation dose from low-dose 64-slice CT with prospective ECG-triggering versus invasive coronary angiography. Heart 2009;95:1656-61.
- Schoenhagen P. Back to the future: coronary CT angiography using prospective ECG triggering. Eur Heart J 2008;29:153-4.
- Shuman WP, Branch KR, May JM, et al. Prospective versus retrospective ECG gating for 64-detector CT of the coronary arteries: comparison of image quality and patient radiation dose. Radiology 2008;248:431-7.
- Pontone G, Andreini D, Bartorelli AL, et al. Diagnostic accuracy of coronary computed tomography angiography: a comparison between prospective and retrospective electrocardiogram triggering. J Am Coll Cardiol 2009;54:346-55.
- Huang B, Li J, Law MW, et al. Radiation dose and cancer risk in retrospectively and prospectively ECG-gated coronary angiography using 64-slice multidetector CT. Br J Radiol 2010;83:152-8.
- Stolzmann P, Goetti R, Baumueller S, et al. Prospective and retrospective ECG-gating for CT coronary angiography perform similarly accurate at low heart rates. Eur J Radiol 2011;79:85-91.
- Hong YJ, Kim SJ, Lee SM, et al. Low-dose coronary computed tomography angiography using prospective ECG-triggering compared to invasive coronary angiography. Int J Cardiovasc Imaging 2011;27:425-31.
- Lu B, Lu JG, Sun ML, et al. Comparison of diagnostic accuracy and radiation dose between prospective triggering and retrospective gated coronary angiography by dual-source computed tomography. Am J Cardiol 2011;107:1278-84.
- Maruyama T, Takada M, Hasuike T, et al. Radiation dose reduction and coronary assessability of prospective electrocardiogram-gated computed tomography coronary angiography: comparison with retrospective electrocardiogram-gated helical scan. J Am Coll Cardiol 2008;52:1450-5.
- Stolzmann P, Leschka S, Scheffel H, et al. Dual-source CT in step-and-shoot mode: noninvasive coronary angiography with low radiation dose. Radiology 2008;249:71-80.
- Roberts WT, Bax JJ, Davies LC. Cardiac CT and CT coronary angiography: technology and application. Heart 2008;94:781-92.
- Achenbach S, Marwan M, Ropers D, et al. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J 2010;31:340-6.
- Lell M, Marwan M, Schepis T, et al. Prospectively ECG-triggered high-pitch spiral acquisition for coronary CT angiography using dual source CT: technique and initial experience. Eur Radiol 2009;19:2576-83.
- Alkadhi H, Stolzmann P, Desbiolles L, et al. Low-dose, 128-slice, dual-source CT coronary angiography: accuracy and radiation dose of the high-pitch and the step-and-shoot mode. Heart 2010;96:933-8.
- Morin RL, Gerber TC, McCollough CH. Radiation dose in computed tomography of the heart. Circulation 2003;107:917-22.
- Sun Z, Ng KH. Prospective versus retrospective ECG-gated multislice CT coronary angiography: A systematic review of radiation dose and diagnostic accuracy. Eur J Radiol 2012;81:e94-e100.
- Hendel RC, Budoff MJ, Cardella JF, et al. ACC/AHA/ACR/ASE/ASNC/HRS/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SIR 2008 Key Data Elements and Definitions for Cardiac Imaging A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Clinical Data Standards for Cardiac Imaging). J Am Coll Cardiol 2009;53:91-124.
- Bongartz G, Golding SJ, Jurik AJ, et al. European guidelines for multislice computed tomography: report EUR 16262 EN 2004. Luxembourg: European Commission,2004.
- Morin RL. Monte Carlo simulation in the radiological sciences. Boca Raton, FL: CRC Press; 1988.
- von Ballmoos MW, Haring B, Juillerat P, et al. Meta-analysis: diagnostic performance of low-radiation-dose coronary computed tomography angiography. Ann Intern Med 2011;154:413-20.
- Sun Z, Ng KH. Diagnostic value of coronary CT angiography with prospective ECG-gating in the diagnosis of coronary artery disease: a systematic review and meta-analysis. Int J Cardiovasc Imaging 2012 Jan 4.
- Hosch W, Heye T, Schulz F, et al. Image quality and radiation dose in 256-slice cardiac computed tomography: comparison of prospective versus retrospective image acquisition protocols. Eur J Radiol 2011;80:127-35.
- Zhang C, Zhang Z, Yan Z, et al. 320-row CT coronary angiography: effect of 100-kV tube voltages on image quality, contrast volume, and radiation dose. Int J Cardiovasc Imaging 2011;27:1059-68.
- DeFrance T, Dubois E, Gebow D, et al. Helical prospective ECG-gating in cardiac computed tomography: radiation dose and image quality. Int J Cardiovasc Imaging 2010;26:99-107.
- Stolzmann P, Scheffel H, Leschka S, et al. Influence of calcifications on diagnostic accuracy of coronary CT angiography using prospective ECG triggering. AJR Am J Roentgenol 2008;191:1684-9.
- Sun ML, Lu B, Wu RZ, et al. Diagnostic accuracy of dual-source CT coronary angiography with prospective ECG-triggering on different heart rate patients. Eur Radiol 2011;21:1635-42.
- Freeman A, Learner R, Eggleton S, et al. Marked reduction of effective radiation dose in patients undergoing CT coronary angiography using prospective ECG gating. Heart Lung Circ 2011;20:512-6.
- Hoe J, Toh KH. First experience with 320-row multidetector CT coronary angiography scanning with prospective electrocardiogram gating to reduce radiation dose. J Cardiovasc Comput Tomogr 2009;3:257-61.
- Labounty TM, Leipsic J, Min JK, et al. Effect of padding duration on radiation dose and image interpretation in prospectively ECG-triggered coronary CT angiography. AJR Am J Roentgenol 2010;194:933-7.
- Xu L, Yang L, Zhang Z, et al. Low-dose adaptive sequential scan for dual-source CT coronary angiography in patients with high heart rate: comparison with retrospective ECG gating. Eur J Radiol 2010;76:183-7.
- Buechel RR, Husmann L, Herzog BA, et al. Low-dose computed tomography coronary angiography with prospective electrocardiogram triggering: feasibility in a large population. J Am Coll Cardiol 2011;57:332-6.
- Hlaihel C, Boussel L, Cochet H, et al. Dose and image quality comparison between prospectively gated axial and retrospectively gated helical coronary CT angiography. Br J Radiol 2011;84:51-7.
- Feng Q, Yin Y, Hua X, et al. Prospective ECG triggering versus low-dose retrospective ECG-gated 128-channel CT coronary angiography: comparison of image quality and radiation dose. Clin Radiol 2010;65:809-14.
- Duarte R, Fernandez G, Castellon D, et al. Prospective Coronary CT Angiography 128-MDCT Versus Retrospective 64-MDCT: Improved Image Quality and Reduced Radiation Dose. Heart Lung Circ 2011;20:119-25.
- Qin J, Liu LY, Meng XC, et al. Prospective versus retrospective ECG gating for 320-detector CT of the coronary arteries: comparison of image quality and patient radiation dose. Clin Imaging 2011;35:193-7.
- The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 2007;37:1-332.
- Gosling O, Loader R, Venables P, et al. Cardiac CT: are we underestimating the dose? A radiation dose study utilizing the 2007 ICRP tissue weighting factors and a cardiac specific scan volume. Clin Radiol 2010;65:1013-7.
- Einstein AJ, Elliston CD, Arai AE, et al. Radiation dose from single-heartbeat coronary CT angiography performed with a 320-detector row volume scanner. Radiology 2010;254:698-706.


