A comparison of Cornell and Sokolow-Lyon electrocardiographic criteria for left ventricular hypertrophy in a military male population in Taiwan: the Cardiorespiratory fitness and HospItalization Events in armed Forces study
Introduction
Left ventricular hypertrophy (LVH) measured by echocardiography or magnetic resonance imaging studies has been well regarded as a form of end-organ damage and an early sign of cardiac dysfunction in patients with hypertension or multiple metabolic abnormalities (1). Twelve-lead body surface electrocardiography (ECG) is a cost-effective tool, and several ECG voltage criteria for identifying LVH have been widely applied in clinical practice and for researches. Of these, both sex-independent Sokolow-Lyon and sex-specific Cornell voltage criteria are used most commonly (2,3). Moreover, the product of QRS duration and voltage based on the Sokolow-Lyon and Cornell criteria for detecting LVH has shown more accurately than the voltage criteria alone (4,5). Nevertheless, ECG-derived LVH has been associated with the occurrence of a wide range of cardiovascular disease (CVD) such as atrial fibrillation and stroke independent of echocardiographic LVH in the general population (6,7).
In contrast, professional military members have to take regular rigorous physical training including endurance and resistance exercise to maintain their outstanding fitness. Frequent exercise training and well physical fitness have been associated with lower risk of incident CVD and mortality in the general population (8,9). However, there were conflicting results with regard to the cardiovascular outcomes in those taking repetitive vigorous exercise (10,11). To our best knowledge, cardiac remodeling such as left ventricular muscle hypertrophy and chamber dilatation are commonly present in athletes (12). Whether these physiological cardiac adaptations to repetitive strenuous training on future CVD and mortality events remain unclear in armed forces. In addition, the prevalence of ECG-derived LVH in professional military male members in the East Asian and Jewish populations was estimated 15–20% (13,14), which was much lower than that of 45% in the elite White male athletes (15).
Although current guideline recommended that isolated ECG voltage criterion for LVH in athletes was considered as normal cardiac adaptations to exercise, evidence for the associations of each ECG criterion with LVH estimated by imaging studies was lacking in the military members, especially of the Asian male population. Therefore the aim of our study was to compare the Cornell criteria with the Sokolow-Lyon criteria for the echocardiographic LVH in a large military male cohort in Eastern Taiwan.
Methods
Study population
The Cardiorespiratory fitness and HospItalization Events in armed Forces (CHIEF) is a retrospective cohort consisting of 4,080 professional military members aged 18–50 years completing the annual health examination and undergoing any one of three exercise tests in eastern Taiwan during 2014. The study design has been described in detail previously (14). Of these, there were 620 subjects underwent cardiac examinations of ECG and echocardiography simultaneously for their promotions to senior rank and advanced training. Women (n=53) and those with hypertension (systolic blood pressure >140 mmHg, or diastolic blood pressure >90 mmHg, or receiving antihypertensive therapy) or ECG findings of bundle branch block (n=28) were excluded, leaving a sample of 539 male members for the final analyses.
Measurements of 12-lead body surface ECG
All standard 12-lead body surface ECGs (Philips PageWriter Trim III) recorded at 25 mm/sec paper speed and 1 mV/cm were prospectively performed by a well-experienced technician (Yun-Shun Yu). ECG variables including QRS duration, R-wave amplitudes in leads aVL, V5, and V6, and S-wave amplitudes in leads V1 and V3 were retrospectively measured twice by two well-trained technicians (Yun-Shun Yu and Felicia Lin), and confirmed by a cardiologist (Gen-Min Lin) at Hualien-Armed Forces General Hospital. The Sokolow-Lyon voltage criterion-based LVH was defined as a composite of amplitudes (SV1 or V2 + RV5 or V6) ≥35 mm, and the Cornell voltage criterion-based LVH was defined as RaVL+ SV3 ≥28 mm for men (2,3). In addition, the Sokolow-Lyon product criterion-based LVH was defined as a sum of QRS duration times the corresponding Sokolow-Lyon voltage ≥3,340 mm × ms, and the Cornell product criterion-based LVH was defined as QRS duration times the corresponding Cornell voltage ≥2,440 mm × ms (4,5).
Measurements of echocardiography
All procedures of echocardiography (iE33; Philips Medical Systems, Andover, MA, USA) were carried out by a well-experienced technician (Yun-Shun Yu) using a 1–5 MHz transducer and the reports were reviewed by a cardiologist (Gen-Min Lin) at Hualien-Armed Forces General Hospital. All study subjects were prepared in supine and left lateral positions and examined using parasternal long-axis and short-axis views and in the apical four and two-chamber views. On the basis of the recommendations of the American Society of Echocardiography (16), quantification of left ventricular chamber dimension (diastolic diameter) and wall thickness (interventricular septal and posterior wall) were measured approximately at the mitral valve tips and at the onset of the QRS complex of end diastole in parasternal long axis view. M-mode and two-dimensional measurements of left ventricular mass (LVM) used the leading edge-to-leading-edge method. LVM was calculated based on the corrected American Society of Echocardiography formula by Devereux et al. (17).
LVM = 0.8 × {1.04 × [(left ventricular end diastolic diameter (LVIDd) + end diastolic posterior wall thickness (PWTd) + end diastolic interventricular septal thickness (IVSTd)]3 − LVIDd3} + 0.6
LVM was respectively indexed for body surface area (LVM/BSA, g/m2), according to the Dubois formula, and for height2.7 (LVM/height2.7, g/m2.7) on the basis of the recommendation by de Simone et al. (18). The cut-off value for echocardiographic LVH was set as LVM/BSA ≥116 g/m2 and LVM/height2.7 ≥49 g/m2.7 in the military male population (19).
Statistical analysis
Baseline characteristics of the CHIEF military male cohort were reported as mean ± standard deviation or percent for continuous and categorical variables respectively. Pearson’s correlation coefficient (r) was used to determine the degree of correlation between each ECG criterion and the two LVM indexes, and compared by the Fisher’s z test. Receiver-operating characteristics (ROC) curves were used to compare the performance of each ECG criterion for the echocardiographic LVH over a range of specificities. Pairwise comparisons of the four ECG criteria for LVH were performed using differences between the areas under the curves (AUC). The sensitivity and specificity of each ECG criterion-derived cut-off value for echocardiographic LVH were compared. In addition, we also calculated the sensitivities and corresponding cut-off values for each criterion at fixed specificity levels of 90%, 95%, and 100% (20). A two-tailed value of P<0.05 was considered significant. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Ethic statement
This study was approved by the Institutional Review Board of the Mennonite Christian Hospital (No. 16-05-008) in Hualien, Taiwan. Informed consent was not required by the Board because of a retrospective study.
Results
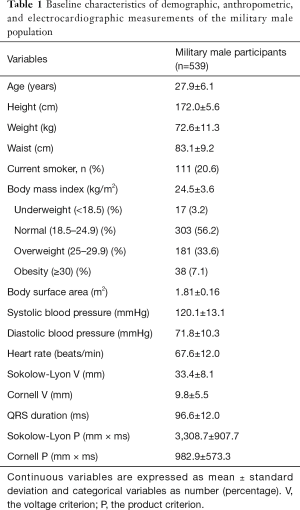
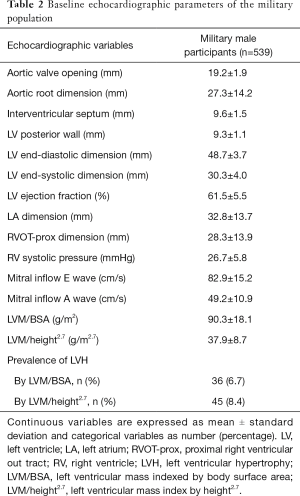
The baseline demographic, anthropometric, ECG, and echocardiographic characteristics of the military male cohort were shown in Table 1 and Table 2 respectively. Ages in the study subjects were between 18 and 50 years and more than 95% of them were less than 40 years. The prevalence of echocardiographic LVH was 6.7% as LVM/BSA ≥116 g/m2 and 8.4% as LVM/height2.7 ≥49 g/m2.7 respectively.
Full table
Full table
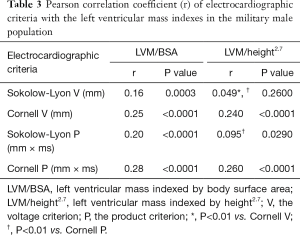
Correlation of each ECG criterion with the LVM indexes
Table 3 shows that all four ECG criteria were correlated with the LVM/BSA index (r=0.217−0.507). However, the Sokolow-Lyon voltage criterion was not correlated with the LVM/height2.7 index. The correlation coefficients of the Cornell criteria were higher than that of Sokolow-Lyon criteria, but this result was significant only for the LVM/height2.7 index. In addition, there were similar correlations between the ECG voltage and the product criterion with the LVM indexes.
Full table
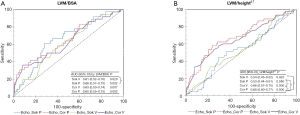
Performance of the four ECG criteria for the echocardiographic LVH using ROC curve and traditional cut-off value
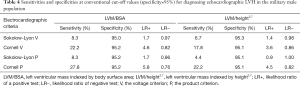
Figure 1A shows similar AUC (range, 0.61–0.66) among the four ECG criteria for the LVM/BSA ≥116 g/m2 except that the AUC of the Sokolow product criterion was modestly higher than that of the Sokolow voltage criterion (0.66 vs. 0.61). In contrast, Figure 1B shows that the Cornell voltage and product criteria had higher AUC (0.66 and 0.68 respectively) than those of Sokolow-Lyon criteria (0.54 and 0.53 respectively) for the LVM/height2.7 ≥49 g/m2.7. The differences between the Cornell and the Sokolow-Lyon criteria were almost significant except the difference in the voltage criteria. Table 4 shows that the sensitivities for the traditional cut-off values were generally low, especially using the Sokolow-Lyon voltage and product criteria for the LVM/BSA ≥116 g/m2 and LVM/height2.7 ≥49 g/m2.7 indexes of LVH (6.7–8.3% and 4.4–8.3% respectively). The test-negative likelihood ratio was estimated from 0.76 to 0.98 due to the low sensitivities of the four ECG criteria for the echocardiographic LVH.
Full table
Performance of the four ECG criteria using revised cut-off values
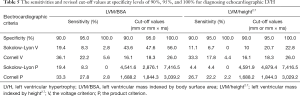
Since the specificities were all around 95% using traditional cut-off values, the sensitivity of cut-off value for each ECG criterion at a fixed specificity level of 95% was unchanged (Table 5). Notably, the sensitivities remained the lowest, using the Sokolow-Lyon criteria for the LVM/height2.7 ≥49 g/m2.7 (4.4–11.1%) at a fixed specificity level of 90%.
Full table
Discussion
Our principal finding was that both of the Cornell voltage and product ECG criteria performed superior to the Sokolow-Lyon criteria in the correlation with the echocardiographic LVM/height2.7 defined LVH and the AUC of the ROC in a young military male population in Taiwan. Another important finding was that there was no difference between the Cornell voltage and the product criteria in the performance for detecting the echocardiographic LVH. In addition, the Cornell voltage and product ECG criteria showed better sensitivity than the Sokolow-Lyon criteria under a fixed specificity of 95%.
Most previous studies investigating the performance of different ECG criteria for LVH evaluated by echocardiography or magnetic resonance imaging were conducted in hypertensive patients of the Western countries (21,22). Some studies have shown that there was ethnical difference between hypertensive Whites and African Americans in the ECG diagnostic performance (23,24). In summary, the Sokolow-Lyon voltage criterion had better sensitivity in African American patients, but in contrast the Cornell voltage criterion was superior in White patients. However, there were few studies for the association of ECG criteria with LVH in the Asian populations. In Chinese patients with hypertension (25), Xie et al. uncovered that the Cornell voltage and product criteria had better sensitivity to detect echocardiographic LVH than other criteria in men and women. In Korean patients, Park et al. demonstrated that the Cornell product criterion was superior in woman, but the Sokolow-Lyon product criterion had better sensitivity in men (20).
As compared with the correlations of the ECG criteria with the LVM index in middle-aged male patients with hypertension, we found that the correlation coefficients were much less in the young military male cohort free of hypertension in Taiwan (30–50% vs. 15–30%) (20,25). In line with previous reports, use of the ECG criteria in the diagnosis of LVH is limited in the male military population as well because of the low sensitivity of the method (26). As is known, the prevalence of ECG-defined LVH was high in professional military members undergoing regular rigorous exercise training, however the prevalence of echocardiographic LVH was relatively low which was less than 10% in the present study and in the Israeli Air Force study (13). As a result, the correlations of the ECG criteria with the LVM index may be decreased in the military male cohort free of hypertension. In addition, the sensitivity of a combined Sokolow-Lyon and Cornell voltage criterion for LVH in the Israeli Air Force study was higher than that in the present study (55% vs. 30%). This might be explained by a more strict definition of echocardiographic LVH in the Israeli study, which was set as the LVM/BSA index ≥132 g/m2.
The Sokolow-Lyon voltage and product criteria had poor correlations with the LVM/height2.7 and the AUC of the ROC for the index in the present study. This finding was unexpected and not consistent with the Cornell ECG criteria. The reason could be explained in part by that unlike the Cornell criteria using frontal lead RaVL amplitude, the Sokolow-Lyon criteria used precordial leads amplitudes only and might be affected much if the LVM was indexed for height raising to an exponential power of 2.7. Therefore the application of the Sokolow-Lyon criteria for echocardiographic LVH should be cautious in the young fit male subjects for the LVM/height2.7 index.
There were several limitations in our study. First, the study population included only male subjects, making it difficult to apply the results to the female subjects. Second, the military members were considered to be a healthy cohort and the results could not be applied to the general populations who have multiple comorbidities. Third, we compared the Sokolow-Lyon with the Cornell-based criteria for echocardiographic LVH and the accuracy of other ECG criteria needs further investigation. Fourth, a small number of patients with hypertrophic cardiomyopathy might be included in the LVH group. Finally the present male cohort accounted for only 15% of the overall CHIEF male cohort, which might result in a selection bias despite that the baseline characteristics were similar to that of the overall CHIEF male cohort. In conclusion, the Cornell voltage and product criteria for echocardiographic LVH had better performance than the Sokolow-Lyon ECG criteria in a young military male cohort in Taiwan. In addition, the Sokolow-Lyon criteria should be cautiously used to correlate the index of LVM/height2.7 in this population.
Acknowledgements
Funding: The study was supported by the Research Grants from the Hualien-Armed Forces General Hospital (805-C105-10) and the Ministry of National Defense-Medical Affairs Bureau (MAB-106-124).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Review Board of the Mennonite Christian Hospital (No. 16-05-008) in Hualien, Taiwan. Informed consent was not required by the Board because of a retrospective study.
References
- Bluemke DA, Kronmal RA, Lima JA, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (Multi-Ethnic Study of Atherosclerosis) Study. J Am Coll Cardiol 2008;52:2148-55. [Crossref] [PubMed]
- Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 1949;37:161-86. [Crossref] [PubMed]
- Devereux RB, Casale PN, Eisenberg RR, et al. Electrocardiographic detection of left ventricular hypertrophy using echocardiographic determination of left ventricular mass as the reference standard. Comparison of standard criteria, computer diagnosis and physician interpretation. J Am Coll Cardiol 1984;3:82-7. [Crossref] [PubMed]
- Okin PM, Roman MJ, Devereux RB, et al. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol 1995;25:417-23. [Crossref] [PubMed]
- Alfakih K, Walters K, Jones T, et al. New gender-specific partition values for ECG criteria of left ventricular hypertrophy: recalibration against cardiac MRI. Hypertension 2004;44:175-9. [Crossref] [PubMed]
- Kohsaka S, Sciacca RR, Sugioka K, et al. Additional impact of electrocardiographic over echocardiographic diagnosis of left ventricular hypertrophy for predicting the risk of ischemic stroke. Am Heart J 2005;149:181-6. [Crossref] [PubMed]
- Chrispin J, Jain A, Soliman EZ, et al. Association of electrocardiographic and imaging surrogates of left ventricular hypertrophy with incident atrial fibrillation: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2014;63:2007-13. [Crossref] [PubMed]
- Wei M, Kampert JB, Barlow CE, et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA 1999;282:1547-53. [Crossref] [PubMed]
- Lee DC, Sui X, Artero EG, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation 2011;124:2483-90. [Crossref] [PubMed]
- Schnohr P, O’Keefe JH, Marott JL, et al. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol 2015;65:411-9. [Crossref] [PubMed]
- Armstrong ME, Green J, Reeves GK, et al. Frequent physical activity may not reduce vascular disease risk as much as moderate activity: large prospective study of women in the United Kingdom. Circulation 2015;131:721-9. [Crossref] [PubMed]
- Spirito P, Pelliccia A, Proschan MA, et al. Morphology of the “athlete’s heart” assessed by echocardiography in 947 elite athletes representing 27 sports. Am J Cardiol 1994;74:802-6. [Crossref] [PubMed]
- Grossman A, Prokupetz A, Koren-Morag N, et al. Comparison of usefulness of Sokolow and Cornell criteria for left ventricular hypertrophy in subjects aged <20 years versus >30 years. Am J Cardiol 2012;110:440-4. [Crossref] [PubMed]
- Lin GM, Li YH, Lee CJ, et al. Rationale and design of the cardiorespiratory fitness and hospitalization events in armed forces study in Eastern Taiwan. World J Cardiol 2016;8:464-71. [Crossref] [PubMed]
- Sharma S, Whyte G, Elliott P, et al. Electrocardiographic changes in 1000 highly trained junior elite athletes. Br J Sports Med 1999;33:319-24. [Crossref] [PubMed]
- Sahn DJ, DeMaria A, Kisslo J, et al. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 1978;58:1072-83. [Crossref] [PubMed]
- Devereux RB, Alonso DR, Lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986;57:450-8. [Crossref] [PubMed]
- de Simone G, Kizer JR, Chinali M, et al. Normalization for body size and population-attributable risk of left ventricular hypertrophy: the Strong Heart Study. Am J Hypertens 2005;18:191-6. [Crossref] [PubMed]
- Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440-63. [Crossref] [PubMed]
- Park JK, Shin JH, Kim SH, et al. A comparison of cornell and sokolow-lyon electrocardiographic criteria for left ventricular hypertrophy in korean patients. Korean Circ J 2012;42:606-13. [Crossref] [PubMed]
- Truong QA, Ptaszek LM, Charipar EM, et al. Performance of electrocardiographic criteria for left ventricular hypertrophy as compared with cardiac computed tomography: from the Rule Out Myocardial Infarction Using Computer Assisted Tomography Trial. J Hypertens 2010;28:1959-67. [Crossref] [PubMed]
- Okin PM, Devereux RB, Jern S, et al. Regression of electrocardiographic left ventricular hypertrophy by losartan versus atenolol: The Losartan Intervention for Endpoint reduction in Hypertension (LIFE) Study. Circulation 2003;108:684-90. [Crossref] [PubMed]
- Okin PM, Wright JT, Nieminen MS, et al. Ethnic differences in electrocardiographic criteria for left ventricular hypertrophy: the LIFE study. Losartan Intervention For Endpoint. Am J Hypertens 2002;15:663-71. [Crossref] [PubMed]
- Chapman JN, Mayet J, Chang CL, et al. Ethnic differences in the identification of left ventricular hypertrophy in the hypertensive patient. Am J Hypertens 1999;12:437-42. [Crossref] [PubMed]
- Xie L, Wang Z. Correlation between echocardiographic left ventricular mass index and electrocardiographic variables used in left ventricular hypertrophy criteria in Chinese hypertensive patients. Hellenic J Cardiol 2010;51:391-401. [PubMed]
- Devereux RB, Reicheck N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977;55:613-8. [Crossref] [PubMed]


