Global progress in prevention of cardiovascular disease
Trends in cardiovascular disease (CVD)
An estimated 17.5 million died of CVD in 2012 accounting for 46% of all noncommunicable disease (NCD) deaths (1). Of these deaths, an estimated 7.4 million were due to coronary heart disease, 6.7 million due to stroke and the rest (3.4 million), due to heart failure and arrhythmias as a consequence of hypertension, rheumatic heart disease, other cardiac valve disease and cardiomyopathies. In most countries, the absolute number of deaths from CVD is increasing due to increased longevity and associated population ageing and deaths of people older than 70 years of age (2). If account is taken of population ageing, cardiovascular mortality rates have declined globally by 16% between 2000 and 2012 (1). A trend driven by declines in tobacco use, population-level blood pressure improvements and advances in treatment of CVD. Declines have been greater in high-income countries than in low- and middle-income countries (3,4). There are very few data on CVD trends from low-income countries and some middle-income countries because of lack of vital registration systems and incomplete information on causes of death.
Trends in behavioral risk factors of CVD
Tobacco, harmful use of alcohol, unhealthy diet and physical inactivity are the four behavioural risk factors that drive the global CVD epidemic. Tobacco use is responsible for 10% of all deaths from CVDs (5). The global prevalence of tobacco smoking among people aged 15 years and older is estimated to have declined from 27% in 2000 to 21% in 2013 (6). Globally, smoking prevalence declined in both men and women. Declines were largest (around 10%), for men in the high-income Organisation for Economic Co-operation and Development (OECD) countries, and in low, middle- and non-OECD high-income countries in the European Region and the Region of the Americas. However, the prevalence of smoking appears to be increasing in the African Region and the Eastern Mediterranean Region (6). In the European Region, the Western Pacific Region and the South-East Asia Region, prevalence of tobacco smoking is still high (6).
An estimated 780,381 cardiovascular deaths were attributable to alcohol consumption globally in 2012 (7). Alcohol consumption has declined in Southern Europe and a few countries in South America, for decades (8,9). In other western countries, trends have been downwards in the presence of alcohol control policies like taxes and regulations that increase prices and restrict access. Trends have been upwards where there has been little or no policy interventions. Alcohol use is rising steadily in many countries in Asia, due to the higher purchasing power combined with weak alcohol control policies (9).
The main dietary factors which impact on cardiovascular mortality include saturated fat, trans fat, salt and insufficient fruits and vegetables. Pooling of worldwide nutrition surveys and analysis of food availability data from the United Nations Food and Agricultural Organization (FAO) found that between 1990 and 2010, intakes of saturated fats and trans fats were stable at the global level, reflecting a decline in high-income countries and a rise in low- and middle-income countries. Intake of saturated fats nominally increased in Southern Sub-Saharan Africa, Tropical Latin America, Central Latin America and South Asia (10). Consumption of trans fat increased in six regions, largest in North Africa/Middle East and South Asia. Intakes nominally decreased in Southern Sub-Saharan Africa and Western Europe (11).
Insufficient intake of fruit and vegetables is estimated to cause around 11% of ischaemic heart disease deaths and about 9% of stroke deaths globally (12). Data are very limited on global trends in the consumption of fruits and vegetables. While consumption remains inadequate in most low- and middle-income countries it is increasing in some high-income western and Asian countries (13).
Reductions in population salt intake have been reported in Japan, Finland and the United Kingdom (14-17). In Finland, it is associated with lower deaths from stroke (15,16). Analyses of worldwide surveys have reported high salt intake, with little change over time, in many other countries (18,19).
Data are limited on global trends in physical inactivity. In 2010, 23% of adults aged 18 years and over were insufficiently physically active (5). The prevalence of physical inactivity in high-income countries (33%) was about double that in low-income countries (17%) (5).
Country commitments to prevention
To prevent CVD, policies are required to reduce exposure of populations to behavioural risk factors as well as for individual prevention through early detection and treatment of people, who are already at high cardiovascular risk due to years of exposure. In response to the commitments made at the 2011 UN high-level meeting on NCDs, countries have agreed on a set of global voluntary targets to address both requirements (Table 1) (20). There are targets for tobacco and alcohol use, physical activity and salt intake to be attained by 2025 (targets 2, 3, 4 and 5). Global voluntary target 8 and 9 focus country action on individual prevention through early detection and treatment including through better access to medicines. Targets 6 and 7 are two additional targets on raised blood pressure and glucose and obesity. The overarching target is to reduce premature mortality from major NCDs including CVD by 25% from 2010 levels by 2025 (target 1). Modeling has shown that achieving the risk factor targets (aimed at strengthening prevention), can contribute substantially towards meeting the premature mortality target at the global and regional levels (21,22).
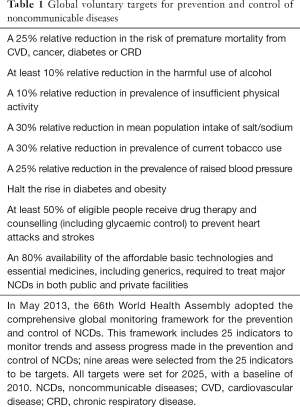
Full table
Progress since the United Nations high level meeting
Since the United Nations high level meeting on NCD prevention and control in September 2011, significant progress has been made by countries in prevention of NCD/CVD (23). Sixty-six percent of countries, have established NCDs units within Ministries of Health and 37% (61/166) have started to develop national action plans. Eighty-one percent (135/166) of countries have an operational action plan, in line with the World Health Organization (WHO) Framework Convention on Tobacco Control to reduce the burden of tobacco use. Sixty-seven percent (111/166) have an operational action plan to reduce harmful use of alcohol. Seventy-two percent (119/166) of countries are taking action to reduce physical inactivity and promote physical activity. Policies to reduce unhealthy diet have been operationalized in 74% (123/166) countries. Twenty-nine percent (48/166) of countries had a NCD surveillance and monitoring systems in place to enable reporting against the nine voluntary global NCD targets.
According to the results of the most recent WHO Country capacity survey (23), downward trends are seen in several outcome indicators when compared to 2010 levels. Unconditional probability of dying between ages of 30 and 70 from CVDs, cancer, diabetes or chronic respiratory diseases has declined from 20% to 19%. Prevalence of current tobacco smoking use among adults has declined from 23.1% to 21.8%. Total alcohol per capita consumption within a calendar year has reduced from 6.4 to 6.3 litres of pure alcohol. Age-standardized prevalence of raised blood pressure in adults has reduced from 23% to 22%. However, both the age standardized prevalence of obesity and diabetes showed an upward trend; 11% to 13% and 8% to 9% respectively.
Measuring the progress in prevention of CVDs
In July 2014, the United Nations General Assembly conducted a review to assess progress in implementing the 2011 Political Declaration, and recognized the progress achieved at national level summarized above. Recognizing also that progress made was insufficient and highly uneven, and that continued and heightened efforts are essential, the members of the United Nations committed themselves to a set of measures within four priority areas—governance, prevention, health care, and surveillance and monitoring (24). These time-bound measures include setting national NCD targets consistent with global targets, developing national NCD multisectoral plans by 2015, and starting implementation of those plans by 2016, in order to achieve the national targets. Progress achieved in the implementation of the four time-bound commitments will be reported to the United Nations General Assembly in 2017 by the WHO using 10 progress indicators (Table 2) (2), in preparation for the third high-level meeting in 2018. All these indicators measure progress in implementation of very cost effective population wide and individual prevention interventions (WHO best buys) (25). This recognizes the fact that prevention has a cost although it is less expensive than treatment and that certain prevention interventions are affordable to all countries (25).

Full table
Barriers to prevention of CVDs
The current rate of success in prevention of NCD/CVD is insufficient to attain the global voluntary targets by 2025 and bolder measures are required to strengthen population wide prevention and individual prevention. Such measures need to influence the coherence of public policies in sectors such as trade, taxation, agriculture, urban development and food production which have a bearing on tobacco and alcohol use, consumption of unhealthy food and physical inactivity. These types of policy responses are complex and challenging to implement as they are based on multisectoral consultation and multistakeholder collaboration. This is key reason why there is limited success in the implementation of policies to reduce exposure to behavioural risk factors. Another key reason is globalization of marketing and trade, which offers unprecedented opportunities for companies to promote products leading to tobacco use, harmful use of alcohol and consumption of unhealthy food. Yet another reason is poorly managed urbanization which brings with it many risks that have negative implications for prevention of CVD and NCDs. Notably increased urban air pollution and sedentary lifestyles resulting in rising obesity trends. Additional barriers to prevention are on the individual prevention front. Namely, weak health systems including weak health care financing which delay progress in improving coverage of people at risk of heart attacks and stroke and the attainment of global target 8. Further, fragile governance and accountability frameworks, inadequate civic engagement and vested commercial interests, compound the difficulties of responding to all these challenges and barriers. Low and middle income countries particularly, have limited capacity to address them. It is also evident that these challenges and barriers cannot be overcome through narrow approaches limited to the health sector.
Cardiovascular prevention and sustainable development goals (SDGs)
In September 2015, the 2030 Agenda for Sustainable Development was adopted in a United Nations General Assembly (26). This agenda includes 17 SDGs that all Member States have agreed to achieve by 2030 (Table 3). SDG 3, is to “ensure healthy lives and promote well-being for all ages” NCDs including CVD has been included as a specific target in SDG goal 3. This offers an unparalleled prospect for countries to overcome barriers to prevention through integration of the national NCD/CVD response within the broader sustainable development agenda (26). SDG target 3.4 calls for a one third reduction in premature mortality from NCDs by 2030, and is an extension of the global voluntary NCD mortality target. Other SDG targets relevant to cardiovascular prevention include: target 3.A on improvements in tobacco control; target 3.5 on substance abuse, including harmful use of alcohol; target 3.B on supporting research and development of vaccines and medicines for NCDs that primarily affect developing countries, as well as providing access to affordable essential medicines and vaccines for NCDs; and target 3.9 on deaths and illnesses related to hazardous chemicals, as well as air, water and soil pollution and contamination. Finally, target 3.8 addresses universal health coverage, which has important implications for a wide range of CVD prevention and control interventions.
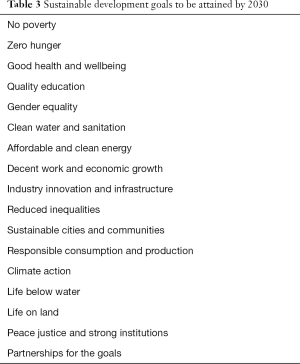
Full table
The other goals of the Sustainable Development Agenda of the United Nations focus on, poverty, hunger, education, gender equality, water and sanitation, energy, economic growth and employment, industry, innovation and infrastructure, sustainable cities, consumption and production, climate change, marine resources, terrestrial ecosystems, peace, justice and accountability and global partnership for sustainable development. There are mutually reinforcing relationships between cardiovascular health and these social, economic and environmental issues which are integral for sustainable development. In this context, the objective of the Geneva Learning Foundation is to address inequalities in all spheres including education and health by connecting people to innovate novel approaches to teaching and learning, using modern information technologies where appropriate.
The 2030 Sustainable Development Agenda offers an extraordinary opening to galvanize progress in cardiovascular prevention for at least three reasons. First, because reducing NCD/CVD mortality is a specific SDG target, cardiovascular prevention activities can be integrated and resourced in the national action plans to attain the SDGs. Second, the SDG agenda is addressing obstacles to CVD prevention such as poverty, inequity and environmental pollution. Finally, many of the challenges which need to be overcome to achieve the health goal of SDGs are common to CVD prevention (27). For example, both CVD prevention and the attainment of the health goal of SDGs require: leadership and collaboration from ministries other than health; reforms in the health governance architecture; locally driven, globally supported approaches to manage the commercial determinants of ill health; specific efforts to elevate social justice and human rights as underlying principles; civil society engagement in all aspects of planning and monitoring including to hold policy makers at all levels accountable for progress and results. The SDGs offer the world a truly global agenda with shared responsibilities. It is an unprecedented opportunity to improve the health and wellbeing of all people, including their cardiovascular health.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author worked in the World Health Organization (WHO) which is a specialized agency of the United Nations that is concerned with international public health for 20 years. She currently serves as an adviser in an honorary capacity, in the Geneva Learning Foundation which is a non-profit organization.
References
- Global Health Estimates: Deaths, disability-adjusted life year (DALYs), years of life lost (YLL) and years lost due to disability (YLD) by cause, age and sex, 2000–2012. Geneva: World Health Organization. Available online: http://www.who.int/healthinfo/global_burden_disease/estimates/en/
- Moran AE, Forouzanfar MH, Roth GA, et al. Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study. Circulation 2014;129:1483-92. [Crossref] [PubMed]
- Di Cesare M, Bennett JE, Best N, et al. The contributions of risk factor trends to cardiometabolic mortality decline in 26 industrialized countries. Int J Epidemiol 2013;42:838-48. [Crossref] [PubMed]
- Ezzati M, Obermeyer Z, Tzoulaki I, et al. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol 2015;12:508-30. [Crossref] [PubMed]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva: World Health Organization, 2013.
- World Health Organization. WHO global report on trends in tobacco smoking 2000-2025. Available online: http://www.who.int/tobacco/publications/surveillance/reportontrendstobaccosmoking/en/
- Rehm J, Shield KD, Roerecke M, et al. Modelling the impact of alcohol consumption on cardiovascular disease mortality for comparative risk assessments: an overview. BMC Public Health 2016;16:363. [Crossref] [PubMed]
- Allamani A, Prina F. Why the Decrease in Consumption of Alcoholic Beverages in Italy between the 1970s and the 2000s? Shedding Light on an Italian Mystery. Contemporary Drug Problems 2007;34:187-197.
- World Health Organization. Global status report on alcohol and health 2014. Geneva: WHO, 2014.
- Wolmarans P. Background paper on global trends in food production, intake and composition. Ann Nutr Metab 2009;55:244-72. [Crossref] [PubMed]
- Micha R, Khatibzadeh S, Shi P, et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys. BMJ 2014;348:g2272. [Crossref] [PubMed]
- World Health Organization. Global Health Risks. Mortality and burden of disease attributable to selected major risks. Geneva: WHO Press, 2009.
- Diet, nutrition and the prevention of chronic diseases. Report of the joint WHO/FAO expert consultation. WHO Technical Report Series, No. 916 (TRS 916). Available online: http://www.who.int/dietphysicalactivity/publications/trs916/en/
- Ikeda N, Gakidou E, Hasegawa T, et al. Understanding the decline of mean systolic blood pressure in Japan: an analysis of pooled data from the National Nutrition Survey, 1986-2002. Bull World Health Organ 2008;86:978-88. [Crossref] [PubMed]
- Tuomilehto J, Geboers J, Joossens JV, et al. Trends in stomach cancer and stroke in Finland. Comparison to northwest Europe and USA. Stroke 1984;15:823-8. [Crossref] [PubMed]
- Vartiainen E, Laatikainen T, Peltonen M, et al. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol 2010;39:504-18. [Crossref] [PubMed]
- He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4:e004549. [Crossref] [PubMed]
- Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. [Crossref] [PubMed]
- Brown IJ, Tzoulaki I, Candeias V, et al. Salt intakes around the world: implications for public health. Int J Epidemiol 2009;38:791-813. [Crossref] [PubMed]
- World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. Geneva: WHO Press, 2013.
- Kontis V, Mathers CD, Bonita R, et al. Regional contributions of six preventable risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modelling study. Lancet Glob Health 2015;3:e746-57. [Crossref] [PubMed]
- Sacco RL, Roth GA, Reddy KS, et al. The Heart of 25 by 25: Achieving the Goal of Reducing Global and Regional Premature Deaths From Cardiovascular Diseases and Stroke: A Modeling Study From the American Heart Association and World Heart Federation. Circulation 2016;133:e674-90. [Crossref] [PubMed]
- World Health Organization. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2015 global survey. Geneva: WHO Press, 2016.
- Outcome document of the high-level meeting of the General Assembly on the comprehensive review and assessment of the progress achieved in the prevention and control of non-communicable diseases. Available online: http://www.mccabecentre.org/downloads/outcome-document.pdf
- From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. Available online: http://www.who.int/nmh/publications/best_buys_summary.pdf
- Transforming our world: the 2030 Agenda for Sustainable Development. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld
- Buse K, Hawkes S. Health in the sustainable development goals: ready for a paradigm shift? Global Health 2015;11:13. [Crossref] [PubMed]


