Current guidelines on prevention with a focus on dyslipidemias
Introduction
The purpose of a clinical guideline is to summarize all available evidence on a particular issue with the aim of assisting healthcare professionals in selecting the best management strategy for an individual patient with a given condition, taking account of the balance between likely benefit and risk. Guidelines offer guidance but not rules, since clinical decisions must be made in the light of the practicing physician’s knowledge, interpretation of the evidence and in the context of shared decision making taking into account patient preferences as well as local cultural and economic factors.
With regards to the management of cardiovascular risk and of dyslipidemias in particular, there are a plethora of guidelines available. In this paper, we focus on two of the most widely used guidelines for the management of dyslipidemia, those of the American College of Cardiology/American Heart Association (ACC/AHA) [2013] (1) and those of the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) [2016] (2). We place these in the context of the 2016 Joint European Guidelines on the Prevention of Cardiovascular Disease in Clinical Practice (3). These latter are, in all major aspects, compatible with the ESC/EAS guidelines on dyslipidemia.
The authors note that a number of substantive and detailed reviews have been published with regards to these guidelines (4-6). We do not intend to replicate these but rather focus on certain core issues that may be relevant to day-to-day clinical practice.
Evidence
All current guidelines require a grading of the evidence presented. The current American and European guidelines use an essentially similar format although there are differences in how many types of evidence were judged admissible. While logical, both pose a problem in that giving the highest evidence to randomized controlled trials (RCTs), while logical, inevitably means that drug treatments will receive a higher grading than lifestyle measures such as smoking cessation, which may indeed have a greater impact on health but are not amenable to RCTs. Also, is the grading system as scientific and objective as it appears, or is there a risk of pseudo-science by merely applying a number to an opinion? In fairness, both sets of guidelines use very exhaustive internal and external review processes so that improbable gradings should have been challenged.
As noted under “Process” below, the expert panel responsible for the ACC/AHA guidelines was constrained by the National Heart, Lung, and Blood Institute (NHLBI) “to evaluate higher quality RCT evidence for cholesterol-lowering drugs to reduce atherosclerotic cardiovascular disease (ASCVD) risk”. In considering this brief, the recommendations relate primarily to statins and were not intended to be a comprehensive set of guidelines for the management of dyslipidemia as a whole.
The ESC/EAS Task Force was not so constrained and felt it reasonable to consider evidence from all relevant disciplines including genetics, pathology, basic science, pharmacology and epidemiology, while fully acknowledging that advices relating to drug treatments should be primarily based on RCT evidence.
Process: ACC/AHA guideline
The ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults was published in Circulation in 2013 (1), as part of a portfolio of publications that also included separate guidelines on cardiovascular risk assessment, lifestyle change, and the management of overweight and obesity (7-9). The original Adult Treatment Panel guidelines for cholesterol had been produced under the auspices of the NHLBI with the most recent revision in 2004 (10), so the gestation was long and arduous and the guidelines were eagerly awaited.
It is particularly important that the ACC/AHA cholesterol guidelines be seen in the context of the other publications, especially those on cardiovascular risk assessment and lifestyle management. This is because the Expert panel was given a very specific, not to say limiting, charge by the NHLBI—“to evaluate higher quality RCT evidence for cholesterol-lowering drugs to reduce ASCVD risk”. Thus, to criticise the guidelines for their highly-focused approach (rather than a comprehensive guideline to dyslipidemia management) is unjust; the expert panel was given a specific and limited task. One may question then if this is a global lipid guideline; further it is possible that the approach of separate papers relating to the various aspects of CVD risk management militates against integrated patient care.
Process: ESC/EAS guideline
The ESC approach to cardiovascular disease prevention is well defined. It is that specialist guidelines such as the ESC/EAS guidelines for the management of dyslipidemias (2) will be compatible with the ESC Joint Guidelines on CVD prevention in clinical practice (3). To this end, all the major “players” in CVD prevention are involved in the Joint Guidelines—the European Society of Cardiology, European Association of Preventive Cardiology, European Atherosclerosis Society, European Association for the Study of Diabetes, European Heart Network, European Society of Hypertension, European Stroke Organization, International diabetes federation, International Federation of Sports Medicine, International Society of Behavioral Medicine and World Organization of Family Doctors (WONCA) Europe, representing general practice.
While there will always be debate on the interpretation of evidence and a need to accommodate new knowledge, both the ESC and the EAS were determined that the categories of risk and the goals and goals for treatment, must be the same in the Joint and the Dyslipidemia guidelines. After considerable debate, this was achieved.
What is high risk?
Both the ACC/AHA and the ESC/EAS guidelines define risk on the basis of known disease, or in the case of apparently healthy persons, on the basis of a risk score.
The ACC/AHA task force developed new, sex-specific Pooled Cohort Equations (http://tools.acc.org/ASCVD-Risk-estimator/) to estimate the 10-year risk of a first fatal or non-fatal ASCVD event in those aged 40–79 and lifetime risk for those aged 20–59 (8). The cohorts included non-Hispanic whites and modest numbers of African-Americans. The system was criticized for over-estimating risks in some groups (11), but this may be inevitable—any system will over-estimate risk in low risk groups and under-estimate it in very high risk groups. For those with diabetes, a 10-year risk of >7.5% identifies those eligible for a high intensity statin (moderate intensity otherwise), and in primary prevention without diabetes a score of >7.5% either a moderate or high intensity statin. However, the calculator should not be used as an automatic prescription for a statin, but as a guide to be used in conjunction with the clinician-patient risk discussion about lifestyle, patient preferences, and risks and benefits of therapy.
The ESC/EAS guidelines retain the SCORE risk estimation system (12) which estimates the 10-year risk of fatal CVD based on ten diverse cohort studies. The use of mortality as opposed to total events was based on the fact that non-fatal events are subject to much variability depending on definitions, diagnostic criteria, methods of ascertainment and other factors, and more particularly because mortality charts can readily be re-calibrated for use in lower and higher risk populations. Recalibrations have been performed to produce many country-specific charts; these are available through the interactive version of SCORE, HeartScore (www.heartscore.org) Re-calibration for non-fatal events is challenging and only possible when very well defined and non-fatal event data are available. That said, re-calibration of the ACC/AHA pooled cohort equations for different American ethnic and social groups would overcome criticisms relating to over- or under-estimation of risk (11).
In the ACC/AHA Guideline, high risk is defined in terms of those in whom it is judged that the weight of the evidence suggests benefit from high intensity statin therapy:
- Those with ASCVD;
- Subjects with a low-density lipoprotein cholesterol (LDL-C) >4.9 mmol/L (190 mg/dL);
- Diabetics subjects aged 40–75 without CVD with an LDL-C of 1.8 mmo/L (70 mg/dL) to 4.9 mmol/L (190 mg/dL);
- Apparently healthy subjects aged 40–75 with an ASCVD risk of ≥7.5%. In addition, it is stated that statins should be considered in subject with an ASCVD risk of 5–7.4%.
The ESC/EAS guidelines define four categories of risk:
- Very high risk: objective evidence of ASCVD, diabetes with goal organ damage, severe chronic kidney disease (CKD) or a calculated SCORE risk of ≥10%;
- High risk: markedly elevated single risk factors, most other subjects with diabetes, moderate CKD or a SCORE risk of ≥ 5 and <10%;
- Moderate risk: SCORE risk ≥1 and <5%;
- Low risk: SCORE <1%.
Risk in younger persons
Communicating risk to younger people may be problematic because absolute risk may be low despite multiple risk factors but will increase rapidly as the person ages. The ACC/AHA guidelines do not address this issue. The ESC/EAS guidelines suggest two approaches to communicate to patients about this issue—the use of relative risk, and the estimation of risk age (13)—a young person with multiple risk factors may have the same risk as a person with optimal risk factor levels who is 20 or more years older. Thus, a 40-year-old may have a risk-age of 60 years or more.
Older persons
The ACC/AHA guidelines have been criticised for the age cut off of 75 years with regards to statin usage. This is inappropriate because what the guideline actually says is “fewer people >75 years of age were included in the statin RCTs reviewed. RCT evidence does support the continuation of statins beyond 75 years of age in persons who are already taking and tolerating these drugs. A larger amount of data supports the use of moderate-intensity statin therapy for secondary prevention in individuals with clinical ASCVD >75 years of age. However, the few data available did not clearly support initiation of high-intensity statin therapy for secondary prevention in individuals >75 years” (1). Furthermore, older persons have a higher absolute risk and therefore greater absolute risk benefit from statins, which must be balanced against any polypharmacy issues in the treatment decision.
The ESC/EAS guidelines (2) suggest that older persons should be treated the same as younger, with the caveat that the starting dose should be lower and titrated with caution
Treat to goal or statins for all at high risk?
This is probably the area that has caused most controversy. The ACC/AHA guideline defined four high-risk groups in whom they felt that high intensity statin therapy should be recommended, but rejected the treat to goal or to the lowest achievable cholesterol level approaches because:
- Treat to goal—this strategy has been the most widely used the past 15 years but there are three problems with this approach. First, current clinical trial data do not indicate what the goal should be and were never designed to test a specific goal, but instead a given statin intensity as the guidelines have supported. Second, we do not know the magnitude of additional ASCVD risk reduction that would be achieved with one goal lower than another. Third, it does not take into account potential adverse effects from multidrug therapy that might be needed to achieve a specific goal. Thus, in the absence of these data, this approach is less useful than it appears. It is possible that future clinical trials may provide information warranting reconsideration of this strategy.
- Lowest is best—this approach was not taken because it does not consider the potential adverse effects of multidrug therapy with an unknown magnitude of ASCVD event reduction. Ongoing RCTs of new LDL-C lowering drugs in the setting of maximal statin therapy may address this question (1).
It will be noted that there is to date no direct RCT evidence for the blanket use of statins, regardless of baseline cholesterol level, in the four high risk categories defined in the ACC/AHA guideline, logical though this approach may be. Nevertheless the Cholesterol Treatment Trialists (CTT) Collaboration data does show a similar (if not greater) relative risk reduction regardless of the baseline LDL-C level (14).
It not reasonable to characterise the ACC/AHA guidelines as focusing only on a global high risk approach, a point that was developed in a thoughtful editorial by one of the lead authors, Jennifer Robinson (14). She states “As we enter the era of personalized medicine, treatment decisions can, and should, be tailored to an individual patient’s level of risk, LDL-C level, and the anticipated benefits and adverse effects from added therapy. This ‘net benefit’ approach was introduced in the 2013 ACC/AHA cholesterol guideline and expanded upon in a subsequent European Heart Journal publication evaluating the results of IMPROVE-IT by this author”. She goes on to illustrate how decision-making can be based on net benefit estimated from the number-needed-to-treat (NNT) for 20% and 50% reductions in LDL-C at different baseline LDL-C levels (15).
Despite these considerations, the recommendation for the “blanket” use of statins in high risk persons regardless of baseline LDL-C generated lively debate (16-19) with considerable reservations about this approach.
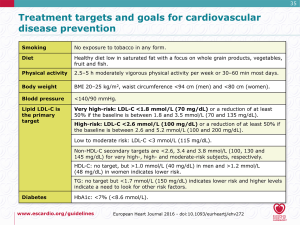
The ESC/EAS Guidelines Task Force was not constrained to consider RCT evidence alone, but was prepared to also consider evidence from genetics (including studies based on Mendelian randomization), basic science, pathology, clinical observation, epidemiology as well as RCTs and high quality systematic reviews. Particular consideration was given to systematic reviews confirming a dose-dependent, linear reduction in CVD with LDL-C lowering (20). No level of LDL-C below which benefit ceases or harm occurs has been defined, and the benefits associated with LDL-C reduction are not specific to statin therapy. While it is accepted that statin usage in all high-risk subjects is likely to reduce risk, most clinicians are more comfortable with an individualised approach based on both baseline LDL-C or total cholesterol level and total risk, and with a defined goal to be achieved, particularly since there is considerable variability in the response of LDL-C to both diet and drug treatments (21). Figure 1 summarizes the ESC/EAS recommended goals.
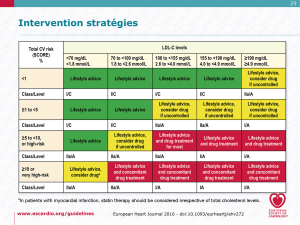
The suggested management process in the ESC/EAS guidelines is graduated by both total risk and baseline LDL-C level, and is shown in Figure 2.
It has been suggested that the ACC/AHA approach focuses on the treatment “process”, whereas the European approach focuses on the treatment “result”. There is no RCT evidence to indicate if the end result would be different, although a recent paper from the Copenhagen General Population Study suggests that, for the primary prevention of ASCVD, the ACC/AHA guidelines more accurately assign therapy to those who would benefit compared with the ESC/EAS guidelines (22). It should be noted that this was not an outcomes study.
A key point with regards to the ESC/EAS guidelines is that the goal for all very high risk subjects is an LDL-C of <1.8 mmol/L (<70 mg/dL), or lower (50% reduction) if the baseline LDL-C is between 1.8 and 3.5 mmol/L (70–135 mg/dL). This was felt by the Task Force to be compatible with current meta-analyses (20) with the addition of the results of the IMPROVE-IT study (23) and offer to every treated patient at least 50% reduction of LDL-C.
These considerations raise the issue of the advisability of using statin therapy for a substantial proportion of the general, apparently healthy population. In this regard, it is noteworthy that the ACC/AHA guidelines devote six lines out of 85 pages to lifestyle issues and only refer to total risk in the context of risk estimation as opposed to management. The critical importance of smoking cessation and blood pressure control were outside their brief. Again, it must be stressed that these issues are addressed in detail in the companion guidelines on cardiovascular risk assessment, lifestyle change, management of overweight and obesity, and hypertension (7-9).
Common ground?
The differences between the ACC/AHA and the ESC/EAS guidelines lie more in the approach to their development and the way of presenting the findings than in the basic principles. Both stress the need for total risk assessment and the assignment of more intensive measures to those at highest risk. They differ in the risk estimation systems offered, in the re-calibration of the ESC/EAS risk system to suit countries with higher or lower mortalities, and in that an individualized, goaled approach is favored in Europe. In fairness, this is by no means precluded in the ACC/AHA guidelines, but receives less prominence. The format of the ESC/EAS guidelines may make it easier for the reader to appreciate the need for a comprehensive approach to all risk factors, although simpler tabular formats for both guidelines are available.
Communication and implementation
Both the ACC/AHA and ESC/EAS guidelines are detailed, dense and may not be at all attractive to practicing physicians. Perhaps they should be regarded primarily as resource documents. The ongoing development of pocket guidelines, summary cards, interactive learning tools and interactive Apps is therefore to be applauded. Similarly, ongoing efforts to allow timely updates without generating confusion are to be supported.
Conclusions
- ASCVD is, in most people, the product of a number of risk factors, notably tobacco exposure, hyperlipidemia, hypertension, inactivity, overweight and diabetes;
- Risk calculators can help in the assessment of risk in apparently healthy persons;
- Persons with established ASCVD and many with diabetes or renal impairment are at high to very high risk and warrant intensive risk factor advice;
- The AHA/EAS guidelines favor the universal use of statins in all high-risk subjects;
- The ESC/EAS guidelines favor a goaled approach based on total risk and baseline LDL-C level;
- Perhaps the most important challenge is in simplifying communications with both healthcare professionals and the public.
Acknowledgements
The authors wish to thank Dr. Angela Pirillo for editorial help.
Footnote
Conflicts of Interest: IM Graham has received speaker fees confined to talks on the content of the guidelines and on risk estimation from MSD and Pfizer. AL Catapano has received speaker/consulting fees from Aegerion, Abbot, Amgen, BMS, Eli Lilly, Genzyme, Kowa, Merck, Novartis, Pfizer, Recordati, Roche, Sanofi and Sigma-Tau. ND Wong has received research support thorough his institution from Amgen, Regneron and Gilead, and speaker/consulting fees from Amgen, Merck, Pfizer, Sanofi and Regeneron.
References
- Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S1-45. [Crossref] [PubMed]
- Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur Heart J 2016;37:2999-3058. [Crossref] [PubMed]
- Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315-81. [Crossref] [PubMed]
- Ray KK, Kastelein JJ, Boekholdt SM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J 2014;35:960-8. [Crossref] [PubMed]
- Giner-Galvan V, Esteban-Giner MJ, Pallares-Carratala V. Overview of guidelines for the management of dyslipidemia: EU perspectives. Vasc Health Risk Manag 2016;12:357-69. [Crossref] [PubMed]
- Lee JC, Zdrojewski T, Pencina MJ, et al. Population Effect of Differences in Cholesterol Guidelines in Eastern Europe and the United States. JAMA Cardiol 2016;1:700-7. [Crossref] [PubMed]
- Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S76-99. [Crossref] [PubMed]
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:S49-73. [Crossref] [PubMed]
- Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation 2014;129:S102-38. [Crossref] [PubMed]
- Grundy SM, Cleeman JI, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation 2004;110:227-39. [Crossref] [PubMed]
- Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet 2013;382:1762-5. [Crossref] [PubMed]
- Conroy RM, Pyorala K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987-1003. [Crossref] [PubMed]
- Cooney MT, Vartiainen E, Laatikainen T, et al. Cardiovascular risk age: concepts and practicalities. Heart 2012;98:941-6. [Crossref] [PubMed]
- Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet 2010;376:1670-81. [Crossref] [PubMed]
- Robinson JG. Lower might be better - It matters how you get there, and in whom. Eur Heart J 2016;37:1380-3. [Crossref] [PubMed]
- EAS (2013) Comment by the EAS Guidelines Committee. New guidelines in USA: 2013 ACC/AHA Guidelines on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk: How do they compare with the EAS/ESC guidelines for the management of dyslipidaemia? Available online: www.cardioprogress.ru/downloads/c2m0i18/КонфликтИнтересов_ENG2.pdf
- Ioannidis JP. More than a billion people taking statins?: Potential implications of the new cardiovascular guidelines. JAMA 2014;311:463-4. [Crossref] [PubMed]
- Statins for millions more? Lancet 2014;383:669. [Crossref] [PubMed]
- Keaney JF Jr, Curfman GD, Jarcho JA. A pragmatic view of the new cholesterol treatment guidelines. N Engl J Med 2014;370:275-8. [Crossref] [PubMed]
- Mihaylova B, Emberson J, Blackwell L, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 2012;380:581-90. [Crossref] [PubMed]
- Boekholdt SM, Hovingh GK, Mora S, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol 2014;64:485-94. [Crossref] [PubMed]
- Mortensen MB, Nordestgaard BG, Afzal S, et al. ACC/AHA guidelines superior to ESC/EAS guidelines for primary prevention with statins in non-diabetic Europeans: the Copenhagen General Population Study. Eur Heart J 2017;38:586-94. [PubMed]
- Blazing MA, Giugliano RP, Cannon CP, et al. Evaluating cardiovascular event reduction with ezetimibe as an adjunct to simvastatin in 18,144 patients after acute coronary syndromes: final baseline characteristics of the IMPROVE-IT study population. Am Heart J 2014;168:205-12.e1. [Crossref] [PubMed]


