Cyanotic congenital heart diseases among Nigerian children
Introduction
The incidence and prevalence of cyanotic congenital heart diseases (CCHD) vary worldwide. It accounts for a third of the congenital heart disease (1). CCHD can be classified into:
- Cyanotic congenital heart disease (CCHD) due to right-to-left shunt with decreased pulmonary flow [tetralogy of Fallot (TOF), pulmonary atresia, right sided hypoplastic heart];
- Cyanotic congenital heart disease due to right-to-left shunt with decreased aortic flow (left-sided hypoplastic heart, interrupted arch, severe coarctation);
- Cyanotic congenital heart disease due to bidirectional shunt (TGA, DORV, TA etc.) (2).
The common CCHD include TOF, transposition of the great arteries (TGA), total anomalous pulmonary venous return (TAPVR), truncus arteriosus and tricuspid atresia (TA) (3). Less common variants include Ebstein’s anomaly, Hypoplastic left heart syndrome, pulmonary atresia and single ventricle. TOF has been widely documented as the most common of all the CCHD (4,5).
Children of all ages are affected by it. Although the defect occurs in-utero, timing of presentation may vary depending on the type of heart lesion, severity of obstruction in the heart and or pulmonary vasculature and associated cardiac anomalies. For example, TGA may present early in the neonatal period while cases with TOF may not present until the end of the first half of the year. In developing countries where the populace has poor health seeking behaviour and reduced access to quality health care, diagnosis may be further delayed until teenage age in some setting.
The exact etiology of CCHD is unknown despite long-standing interest in this disorder. However, some risk factors have been linked to some CCHD. Examples are chemical exposure (6,7), genetic, consanguinity and chromosomal syndromes such as Down syndrome, Turners syndrome and Noonan syndrome, (8,9), infections such as rubella in pregnancy and drug abuse in pregnancy (10-12).
The management of children with CCHD is multidisciplinary (13). Medical treatment may be combined with surgical correction of the defects. The cost implication is enormous and is shared by the family, hospital and the government. The cost of procuring medication and surgical treatment is usually more than anticipated (14-16).
There are limited published reports on CCHD among Nigerian and African Children. Most of the information on CCHD have been extractions from studies on congenital heart diseases. The current report aim to provide the most recent hospital based data on the distribution of CCHD in children less than 14 years of age as well as the demographic characteristics and risk factors identified over a 9 years 6 months’ period.
Methods
Study design
This was a prospective hospital based study.
Study setting
The study was part of a large study carried out in the Department of Paediatrics, Lagos State University Teaching Hospital, a tertiary hospital in South Western Nigeria. The study participant were recruited from January 2007 to June 2016.
Participant
All the participants were children aged 0–14 years of age who either presented for cardiac evaluation or who had echocardiography done within the study period.-The inclusion criteria for the study was based on an echocardiographic diagnosis of a CCHD The diagnosis of CCHD was based on standard echocardiographic definitions.
Study instrument
An Echocardiogram was the main instrument used. Echocardiography was performed using a 2-D echocardiography machine with facility for colored Doppler and M-mode is available (13).
Study protocol
All children who were referred for cardiac evaluation within and or outside the hospital were reviewed. History and physical examinations were obtained as necessary. Plain chest radiograph, electrocardiography and other ancillary investigations were done as required. Echocardiography was subsequently carried out on all the participant. Treatment was commenced as required based on standard protocol within the cardiology unit. Patients who required surgical treatment were referred for surgical correction outside Nigeria. All the patients were followed up in the cardiology unit.
Variables
The variable outcome was:
Ethical clearance for the study was obtained from the research and ethics committee of LASUTH.
- Types and distribution of cyanotic congenital heart disease;
- Mean age of the children;
- Clinical features and indication for echocardiography and cardiac evaluation.
Types and distribution of cyanotic congenital heart disease;
Mean age of the children;
Clinical features and indication for echocardiography and cardiac evaluation.
Data management
The source of the data were echocardiography reports and case notes of the patients. Details concerning the patient’s biodata, clinical presentation, diagnosis, treatment, follow-up and other relevant information were recorded prospectively. The data were analyzed using Statistical Package for Social Sciences (SPSS) version 20.
Descriptive statistic was presented as percentages or means and standard deviation. Means of normally distributed variables were compared using the Student t test and proportions using Chi-square test. Skewed distribution were analyzed using appropriate non-parametric tests. Level of significance set at P<0.05.
Results
Demographic of study participant
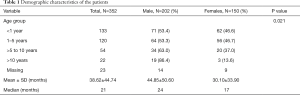
Between January 2007 and June 2016 a total of 352 children had CCHD. There were 202 males and 150 females with a male to female ratio of 1.34:1. The children were age 2 days to 14 years with a mean of 38.62±44.74 months and median of 21 months (3.22±3.73 and 1.75 in years respectively). The males and females were aged 44.85±59.60 with median of 24 months and 30.11±33.90 with median of 17 months respectively. The males were older than the females and the difference in the age of both gender was significant (P=0.003). The ages of the children were ranked in sub-groups as depicted in Table 1. The ranking demonstrates that the modal age at diagnosis was less than 1 year of age. By 5 years of age, approximately 72% of the children had been diagnosed. Less than 10% of the children were adolescents.
Full table
Types of CCHD
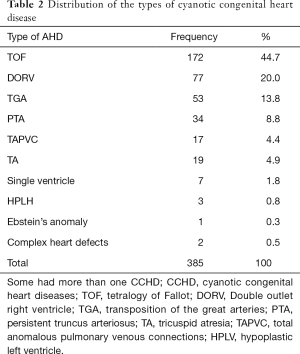
Of the 352 patients, there were 385 cases of CCHD. These were TOF, double outlet right ventricle (DORV), TGA, truncus arteriosus, TA, total anomalous pulmonary venous connections (TAPVC), hypoplastic left ventricle (HPLV) single ventricle and Epstein’s anomaly.
Of the 352 patients with CCHDs, there were 314 isolated defects and 74 cases with more than one defects. Most of the CCHD also had a co-existing ACHD connections. The most common type of CCHD (both isolated and multiple CCHD) was TOF followed DORV and TGA. Table 2 shows the types and frequency of all the CCHDs.
Full table
Clinical presentation and indication for cardiac evaluation
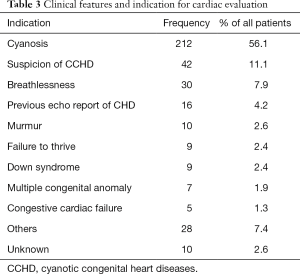
The children presented with various clinical features and some had more than one feature. The most common mode of presentation was cyanosis which occurred in more than half of the patients. Few patients were evaluated for cardiac anomaly based on a previous echocardiographic report of a congenital heart disease for other referral centers. Those cases represented less than 5% of the patients who had cardiac evaluation. The other clinical presentation and indication for cardiac evaluation are highlighted in Table 3.
Full table
Demographic characteristics of the various CCHDs
The demographics of the different subtypes of CCHD are highlighted in Table 4.

Full table
TOF
TOF was the most common CCHD, documented in 44.7% of the children with CCHD. There were a total of 172 cases of TOF, out of which 164 cases were isolated TOF (not in combination with other CCHD). Of the isolated cases, there were 98 males and 66 females with a male to female ratio of 1.5:1. The children were aged 1 month to 14 years. Most of the patients, (45.1%) were between 1 and 5 years of age at diagnosis with a mean of 51.00±46.00 months (4.3±3.8 years) and median of 3 years. Three quarter, 75% of the patients were cyanosed at presentation while two each had cerebral abscess and clinical features in keeping with Down syndrome.
DORV
A total of 77 cases of DORV were recorded. Of the 77 cases, 51 DORV occurred without other cyanotic heart lesions. TGA was the most common cyanotic congenital heart lesion that occurred with the DORV. All the patients with DORV had a co-existing intracardiac connection. The most common was a pulmonary stenosis. The children were aged 1 month to 14 years with a median age of 12 months, (Mean ± SD, 24.47±37.90). The males were almost twice the number of females, (57 males and 27 females) with a male to female ratio of 1.9:1. The age of the males and females were 32.37±43.28 (median of 12 months) and 19.85±21.81 (median of 11 months) respectively. The distribution of the age was the same across the gender, (P=0.658). Most of the children were diagnosed before one year of age. The most common presentation was cyanosis. Others presented with breathlessness, Down syndrome and other congenital disorders.
TGA
There were 53 cases of TGA, comprising 13.3% of all the CCHD. All the study subjects had d-TGA. There were 37 males and 16 females with a male to female ratio of 2.3:1. The mean age of the children at presentation was 10.42±21.70 with a median age of 3.5 months and a bimodal age of 1 and 4 months. The mean age of the males was 10.48±24.14 months with a median of 3.5 months, while that of the females was 10.34±16.03 and a median of 4 months. The distribution of the age of the patients is the same across both sexes (P=0.565). Up to 80% of the patients were less than 12 months of age at presentation. One patient was 13 years of age at diagnosis. All but 5 patients were cyanosed at presentation.
Truncus arteriosus
There were 34 cases of truncus arteriosus comprising 8.8% of all the CCHD. There were 12 males and 22 females with a male to female ratio of 0.5:1. The children were aged 3 weeks to 13 years. Of these, majority, (55.9%) were less than 12 months of age at diagnosis and only one patient was 13 years of age at diagnosis. The ages of the males and females were 38.08±49.05 (median of 19.5) and 16.55±25.06 (median of 5.5) months respectively. There was no significant difference in the age of both gender, (P=0.565). All but 5 patients were cyanosed at presentation.
TA
A total of 19 cases of TA were seen. Those patients also had other CCHD. There were 13 males and six females with a male to female ratio of 2.2:1. The children were aged, 3 weeks to 12 years with a mean age and standard deviation of 38.87±53.08 months and median of 10 months. The age range for the males and females were 3 weeks to 12 years and 2 weeks to 50 months (4.2 years) respectively. The mean and median age for the males and females were 44.16±60.84 and 7 and 25.10±23.26 and 14.5 months respectively. There was no significant difference in the age at diagnosis across the gender, (P=0.512). More than half of the patients were less than one year at diagnosis. The most common mode of presentation amongst the patients was cyanosis.
TAPVC
TAPVC was documented in 17 patients. They were 8 and 9 males and females respectively. The children were aged 2 weeks to 7.2 years with a mean age of 18.34±26.26 months and a median of 3.5 months. The males were aged 27.5±36.38 months with a median age of 5 months. The females were aged 11.22±13.02 months with a median of 3 months. There was no significant difference in the age of both gender, (P=0.871). The modal age group at diagnosis of the children was less than 12 months of age. The patients had various modes of presentation on admission. A third of the patients were cyanosed while a quarter each had congestive cardiac failure and recurrent chest infections respectively.
Others
The rare forms of CCHD were also documented. They include HPLH, Single Ventricle, Epstein’s anomaly and complex CCHD (those patients with more than four combination of CCHD). There were a total of 13 cases of the rare CCHD comprising six male and seven females. They were aged 1 month to 5 years with a mean age of 20.72±21.74 months and a median of 12 months.
Discussion
The present study has documented a recent report on the clinical profile of children with cyanotic congenital heart disease in a tertiary hospital in a developing country. There are limited reports on cyanotic congenital heart disease in Nigeria and Africa. Most of the reports are of congenital heart disease and information about cyanotic heart lesions are extracted from those studies (17-26). While the present study provides a report of CCHD over a 9year period, most of the earlier reports were 5 years and less (17,18,20,21).
The age at diagnosis of CCHD depends on the type of heart lesion and other associated factors such as severity of the lesion, other co-morbidity and where the children reside (western countries or under-developed regions of the world). It was observed that the children with TGA, TAPVC, TA, Truncus Arteriosus and DORV were diagnosed earlier than the patients with TOF. However, the overall age at diagnosis herein reported was in keeping with findings from previous report (17,19,21,27). The difference lies in the study design. While the present study is strictly on CCHD, the previous reports were on congenital heart diseases as a whole. There were no reports on CCHD alone. The finding in this regard shows that most diagnosis are made in the first 12 months of life and by their 5th birthday most children with CCHD had been diagnosed. A possible explanation for more diagnosis been made in the first year may be because of increasing availability of facilities and expertise in the diagnosis of heart disease. Compared to reports in sub-Saharan Africa, in western countries, the diagnosis of CHD as a whole is made early in-utero or during the neonatal period. The reverse is the case in under developed and developing countries where most cases are not diagnosed until late in infancy. Some cases are not even diagnosed until school age and early adolescent. Possible reasons for the late presentation and diagnosis includes difficulty in assessing specialized care, poverty and poor health seeking behavior (28-30).
In the present study, there was a male predominance in the CCHD in totality. A few studies documented a similar report (20,21). While other investigators reported and equal distribution across both gender (17,18,25,27). A possible explanation for the conflicting reports may be because the study methods and designs were different across the studies. For example, there were differences in the age of the study subjects, duration of those studies and subjects’ selection criteria. While the present study was over a nine years’ six-month period, with a focused on CCHD the other studies included acyanotic with cyanotic heart lesions and were largely ≤5 years.
Concerning the distribution of the different types of cyanotic heart lesions, TOF was the most common defect. The finding in this regard is not surprising given that it has been widely established that TOF is the most common CCHD (31-33). It therefore implies that despite difference in geographic location and genetic makeup, the distribution of some congenital heart disease remains the same across regions. The second and third most common CCHD were DORV and TGA. The common trend observed from earlier reports have been TOF followed by TGA (31-33). The prevalence of DORV was higher than TGA in the present study because the calculations included the isolated cases and combined cardiac lesions with DORV. This is because the number of isolated DORV were a little less than the TGAs. Other researchers have documented far less cases of DORV compared to the present study. The reason for the sizeable number in the present study is not clear. Possibilities are the longer duration of the present study and the diagnostic expertise of the Physician who reviewed the patients. Again these are speculations. Significant number of cases of Truncus Arteriosus, TA and TAPVC were reported in the present study compared with previous reports. A plausible explanation may be because the present study was over a longer duration compared with the earlier ones. Other less common defects such as Single Ventricle, Hypoplastic left Heart Syndrome and Ebstein’s anomaly were also noted.
The most common mode of presentation and reason for cardiac evaluation was cyanosis. This is in keeping with expectation considering that all the patients had a CCHD. However, some children were a cyanosed and a suspicion of an ACHD was mode from history and clinical exam. Furthermore, less than 5% of children presented with an echocardiograph report from outside sources with conflicting results and required a review by a Paediatric Cardiologist. In the present study, various clinical presentations were noted. Some patients presented with cerebral abscess, stroke, easy fatigability and the others as highlighted in Table 3. It is known that children with CHDs in general have protean clinical features and sometimes a high index of suspicion is required to make a diagnosis.
The present study also provided report on the different sub-types of CCHD. TOF was the most common CCHD documented in a little under 50% of all the CCHD. It had a male predominance and more than half of the children were cyanosed at presentation. The most common age subgroup at diagnosis was between 1 and 5 years of age. Previous investigators have also documented a male predominance in TOF (23,25,29,34,35). The age at presentation is similar to report by Kennedy et al. in Malawi (36). This is late considering that diagnosis is made in-utero and much earlier in infancy in developed countries. The children with DORV, like those TOF, had a male predominance and cyanosis was the most common mode of presentation. But contrary to that of TOF, most of the children were less than one year of age at diagnosis. Similar to the patients with DORV, the cases of TGA and TA had a male predominance, cyanosis was the most common mode of presentation and most of the cases were less than one year at diagnosis. TGA was different from all three cases because it had the least mean age at diagnosis. This is not surprising given that TGA is the most common cyanotic congenital heart disease in the neonatal period and most cases are diagnosed in-utero and during the neonatal period (2,31). There was a slight difference between Truncus Arteriosus and TA with the other major CCHD. The cases of Truncus Arteriosus had a female predominance while TA had an equal representation of the males and females. But similar to the case of DORV most of the children with Truncus Arteriosus and TA were diagnosed before one year of age and cyanosis was the most common presentation.
The management of children with CCHD is multidisciplinary (13). Medical treatment may be combined with surgical correction of the defects. The cost implication is enormous and is shared by the family, hospital and the government. The cost of procuring medication and surgical treatment is usually more than anticipated (14-16). For most cases, surgical corrections is needed. The needed definitive surgical correction for most of the subjects is not available in Nigeria (Bode and TA ref). At best some palliative surgeries such as a Blalock-Taussig shunt is performed for subjects with TOF. In recent times however, few cases of TOF had intracardiac repair done in Nigeria with the support of experts from abroad (TA). Cardiac surgeries for congenital heart diseases is still generally at infancy stage in Nigeria (Open heart). Most subjects still have to travel abroad to earn the required surgery; this is not within reach of an average Nigerian citizen (37).
Conclusions
Cyanotic congenital heart disease is common among Nigerian children. Males are more affected. Diagnosis is still made late in most of the cases. Definitive surgical correction is not readily available. TOF constituted up to 50% of the subjects. Cyanosis is the most common mode of presentation. Clinical features are protean; thus a high index of suspicion is required to make an early diagnosis.
Acknowledgements
The subjects who participated in the study, their caregivers and other staff involved in their care are gratefully acknowledged.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by research and ethics committee of LASUTH (No. NHREC04/04/2008).
References
- Shah GS, Singh MK, Pandey TR, et al. Incidence of congenital heart disease in tertiary care hospital. Kathmandu Univ Med J (KUMJ) 2008;6:33-6. [PubMed]
- Allen HD, Driscoll DJ, Shaddy RE, et al. Moss and Adams’ Heart disease in Infants, Children and Adolescents: including the Fetus and Young Adults, 7th ed. Baltimore: William and Wilkins. 2008.
- Rao PS. Diagnosis and management of cyanotic congenital heart disease: part I. Indian J Pediatr 2009;76:57-70. [Crossref] [PubMed]
- Grech V. The evolution of diagnostic trends in congenital heart disease: a population-based study. J Paediatr Child Health 1999;35:387-91. [Crossref] [PubMed]
- van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systemic review and meta-analysis. J Am Coll Cardiol 2011;58:2241-7. [Crossref] [PubMed]
- Gorini F, Chiappa E, Gargani L, et al. Potential effects of environmental chemical contamination in congenital heart disease. Pediatr Cardiol 2014;35:559-68. [Crossref] [PubMed]
- Snijder CA, Vlot IJ, Burdorf A, et al. Congenital heart defects and parental occupational exposure to chemicals. Hum Reprod 2012;27:1510-7. [Crossref] [PubMed]
- Richards AA, Garg V. Genetics of Congenital Heart Disease. Curr Cardiol Rev 2010;6:91-7. [Crossref] [PubMed]
- Geis N, Seto B, Bartoshesky L, et al. The prevalence of congenital heart disease among the population of a metropolitan cleft lip and palate clinic. Cleft Palate J 1981;18:19-23. [PubMed]
- Campbell M. Place of maternal rubella in the aetiology of congenital heart disease. Br Med J 1961;1:691-6. [Crossref] [PubMed]
- Polani PE, Campbell M. An aetiological study of congenital heart disease. Ann Hum Genet 1955;19:209-30. [Crossref] [PubMed]
- Shawky RM, Elsayed SM, Zaki ME, et al. Consanguinity and its relevant to clinical genetics. Egyptian Journal of Medical Human Genetics 2013;14:157-64. [Crossref]
- Radu S, Floria M, Baroi GL, et al. Heart Team in cardiovascular disease – between utility and limits. Rom J Cardiol 2016;26:440-9.
- Falase B, Sanusi M, Majekodunmi A, et al. The cost of open heart surgery in Nigeria. Pan Afr Med J 2013;14:61. [PubMed]
- Czosek RJ, Anderson JB. Congenital heart disease and the cost of mortality. Open Heart 2016;3:e000448. [Crossref] [PubMed]
- Hoffman JIe. The global burden of congenital heart disease. Cardiovasc J Afr 2013;24:141-5. [Crossref] [PubMed]
- Otaigbe BE, Tabansi PN. Congenital heart disease in the Niger Delta region of Nigeria: a four-year prospective echocardiographic analysis. Cardiovasc J Afr 2014;25:265-8. [Crossref] [PubMed]
- Chinawa JM, Eze JC, Obi I, et al. Synopsis of congenital cardiac disease among children attending University of Nigeria Teaching Hospital Ituku Ozalla, Enugu. BMC Res Notes 2013;6:475. [Crossref] [PubMed]
- Ibadin MO, Sadoh WE, Osarogiagbon W. Congenital heart diseases at the University of Benin Teaching Hospital. Niger J Paediatr 2005;32:29-32.
- Asani M, Aliyu I, Kabir H. Profile of congenital heart defects among children at Aminu Kano Teaching Hospital, Kano, Nigeria. J Med Trop 2013;15:131-4. [Crossref]
- Sani MU, Mukhtar-Yola M, Karaye KM. Spectrum of Congenital Heart Disease in a Tropical Environment: An Echocardiography Stud. J Natl Med Assoc 2007;99:665-9. [PubMed]
- Jaiyesimi F, Antia AU. Congenital heart disease in Nigeria: a ten year experience at UCH, Ibadan. Ann Trop Paediatr 1981;1:77-85. [Crossref] [PubMed]
- Kapoor R, Gupta S. Prevalence of congenital heart disease, Kanpur, India. Indian Pediatr 2008;45:309-11. [PubMed]
- Bhardwaj R, Rai SK, Yadav AK, et al. Epidemiology of congenital heart disease in India. Congenit Heart Dis Dis 2015;10:437-46. [Crossref] [PubMed]
- Wanni KA, Shahzad N, Ashraf M, et al. Prevalence and spectrum of congenital heart disease in children. Hear India 2014;2:76-9. [Crossref]
- Alabdulgader AA. Congenital heart disease in Saudi Arabia: current epidemiology and future projections. East Mediterr helth J 2006;12 Suppl 2:S157-67.
- Sadoh WE, Uzodimma CC, Daniels Q. Congenital Heart Disease in Nigerian Children. World J Pediatr Congenit Heart Surg 2013;4:172-6. [Crossref] [PubMed]
- Chew C, Halliday JL, Riley MM. Population based study of antenatal detection of congenital heart disease by ultrasound examination. Ultrasound Obstet Gynecol 2007;29:619-24. [Crossref] [PubMed]
- Khadim J, Issa S. Spectrum of congenital heart disease in Basra: an echocardiography study. Med J Basra Univ 2009;27:15-8.
- Animasahun A, Kehinde O, Falase O, et al. Caregivers of children with congenital heart disease: dose socioeconomic class have any effect on their perceptions? Congenit Heart Dis 2015;10:248-53. [Crossref] [PubMed]
- Mitchell SC, Korones SB, Berendes HW. Congenital heart disease in 56,109 births. Incidence and natural history. Circulation 1971;43:323-32. [Crossref] [PubMed]
- Allen HD, Driscoll DJ, Shaddy RE, et al. Moss and Adams’ heart disease in infants, children and Adolescents. Including the fetusand young adults. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 2013.
- Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890-900. [Crossref] [PubMed]
- O’Brien P, Marshall AC. Cardiology patient page. Tetralogy of Fallot. Circulation 2014;130:e26-9. [Crossref] [PubMed]
- Poon LC, Huggon IC, Zidere V, et al. Tetralogy of Fallot in the fetus in the current era. Ultrasound Obstet Gynecol 2007;29:625-7. [Crossref] [PubMed]
- Kennedy N, Miller P. Spectrum of paediatric cardiac disease presenting to an outpatient clinic in Malawi. BMC Res Notes 2013;6:53. [Crossref] [PubMed]
- Animasahun BA, Madise-Wobo AD, Gbelee HO, et al. Children with transposition of the great arteries: Should they actually be born in Nigeria? World J Cardiol 2017;9:277-82. [Crossref] [PubMed]


