A pedometer-based physical activity intervention for patients entering a maintenance cardiac rehabilitation program: a pilot study
Introduction
The health benefits of regular moderate-vigorous-intensity physical activity (MVPA) are substantial and well accepted as a means to prevent chronic disease development (1,2). It is also well known that exercise-based cardiac rehabilitation (CR) programs play an important role in secondary prevention (3,4). Consensus statements recommend 30-60 min/d of moderate-intensity physical activity (PA) on 7 days/week (minimum or 5 days/week) for secondary prevention in patients with established coronary disease (5). Despite the many benefits of increased daily PA for cardiac patients, it has been reported that only 40% of patients attending maintenance CR obtain recommended levels of PA (6). Recent studies of patients attending CR programs showed that although patients achieve recommended amounts of PA on days attending CR, they do not reach recommended PA levels on days they do not participate in CR programs (7-9).
A meta-analysis examining pedometer interventions provides clear evidence that pedometer-driven PA interventions effectively increase daily PA in previously sedentary or irregularly active populations (10). Pedometer-driven PA interventions have been shown to be superior to time-based PA recommendations in improving PA levels in previously inactive women (11). However, time-based recommendations (i.e. 30-60 min/d MVPA) are commonly provided to patients that participate in CR programs to encourage activity on days they do not attend CR. Recently, evidence has shown the potential for utilizing pedometers to help cardiac patients increase their daily PA levels. Ayabe et al. (12) found patients who had attended a maintenance CR program for >6 months could increase PA through the use of self monitoring with a pedometer over a 3-week time period. Similarly, Butler et al. (13) found cardiac patients obtained greater increases in PA after completion of a CR program through the use of pedometer feedback over a 6-week time period in conjunction with goal-setting and telephone follow-up. Presently, it is not known if using pedometers would increase PA levels of patients when first joining a CR program and if a pedometer approach would be superior to the typical time-based recommendations. Thus, the purpose of this pilot study was to determine if daily PA levels of patients during the first 8-weeks of a maintenance CR program would differ between those receiving individualized pedometer-feedback (PF) vs. a usual care (UC) approach of obtaining time-based PA recommendations, particularly on days they do not participate in CR. It was hypothesized that PF would result in greater amounts of daily PA (steps/day and MVPA minutes/day) on both days they participated and did not participate in CR, than the UC approach.
Methods
Subjects
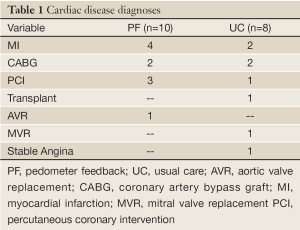
Subjects were recruited upon referral to the maintenance CR program. Eligibility and study inclusion criteria were inactive men and women joining the maintenance CR program with a primary diagnosis of either myocardial infarction, coronary artery bypass graft surgery, percutaneous coronary intervention, heart valve repair/replacement, stable angina, or heart transplant. Inactivity status was determined at the baseline assessment and defined as ≤7,500 steps/d, based on previous findings showing those classified as sedentary or low active were more responsive to increasing their PA compared to regularly active subjects (14). Exclusion criteria included a diagnosis of heart failure or other comorbidity with physician order to limit activity to below moderate-intensity, or inability to self-ambulate without assistive devices. All subjects signed an informed consent document previously approved by the Institutional Review Boards from Ball State University and Ball Memorial Hospital prior to participation. Figure 1 illustrates study recruitment and completion. A total of 18 subjects [PF n=10 (2 women), 53.3±8.1 yrs, 31.5±6.9 kg/m2; UC n=8 (2 women), 59.4±9.9 yrs, 32.4±6.2 kg/m2], participated in the study. Cardiac diagnoses for the subjects are provided in Table 1. There were no significant differences between groups at baseline for age (P=0.241) or body mass index (P=0.987).
Full Table
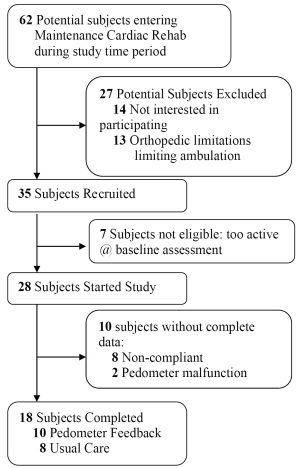
Subject recruitment and completion. Too Active >7,500/day at baseline. Non-compliant – attended CR
Cardiac disease diagnoses
PF, pedometer feedback; UC, usual care; AVR, aortic valve replacement; CABG, coronary artery bypass graft; MI, myocardial infarction; MVR, mitral valve replacement PCI, percutaneous coronary intervention
Study design
Subjects meeting inclusion criteria were alternately, in order of enrollment, assigned to either PF or UC. Subjects were stratified by gender by placing every other male and female in the PF group in an attempt to maintain equal gender distribution in both groups. The duration of the study was 8 weeks with the first week used to establish the baseline PA, and the following 7 weeks as the intervention period.
Physical activity assessment
PA was assessed with NL-1000 pedometers (New-Lifestyles, Inc. Lee’s Summit,
MO) which utilize a piezoelectric accelerometer strain gauge to measure
stepcounts and compute MVPA time. The standard NL-1000 intensity threshold
of
All subjects were encouraged to use ambulatory activities as the primary mode of PA during CR, however 7 subjects (PF, 4; UC, 3) used a recumbent stepper as a complementary mode. The steps accumulated on the stepper were added to the daily pedometer stepcount totals.
Physical activity intervention
All subjects, regardless of group, were given the same recommendation to obtain a minimum of 30-40 min/d MVPA, on days they did not attend CR. The CR program uses 30-40 minutes for all patients when first starting the program. Following baseline assessment, PF subjects received individualized daily stepcount goals to increase by 10% of baseline steps/d for weeks 2-8. For example, a PF subject with 4,000 steps/d at baseline had a weekly increment of 400 steps/d (e.g., weekly stepcount goals of 4,400, 4,800, 5,200, 5,600, 6,000, 6,400, and 6,800 steps/d for weeks 2-8). Daily stepcount goals ranged from 4,227-7,302 steps/d at week 2 to 6,533-11,286 steps/d at week 8, which reflects that on average subjects obtained their step goal on 5 of 7 weeks. To encourage compliance with the daily stepcount goals, PF subjects were instructed to obtain pedometer feedback by recording stepcounts at lunch, dinner, and bedtime. If stepcount goals were not achieved by dinnertime, subjects were encouraged to walk to achieve daily goals.
Statistical analysis
Quality control criteria for pedometer data to be included for analysis were: worn ≥4 d/week (including 1 weekend day), ≥8 hrs/d, ≥1,500 steps/d, and attended CR ≥2 d/week. Data analyses were performed using SPSS 19.0 for Windows (SPSS Inc., Chicago, IL). A 3-way analysis of variance (ANOVA) was performed with one between factor (group: PF vs. UC) and two within factors (time: baseline vs. 8 weeks and CR attendance: CR vs. NCR), along with a Shapiro-Wilk test of normality. Tests for normality were met for all distributions with the exception of MVPA for the UC group, which showed positive skew. Thus the 25th, 50th, and 75th percentile data were also reported. Significance was set at P
Results
During the 8-week study period, subjects attended CR≈3.3 d/week (PF, 3.0±0.7 sessions/week ; UC, 2.7±0.8 sessions/week, P=0.514). The 3-way interaction between group-time-CR attendance for steps/day approached significance, P=0.060, however was not significant for MVPA min/d (Table 2). There was a significant interaction between group and time for both steps/d and MVPA min/d, P<0.04 and P<0.01. PF subjects significantly increased from baseline to 8-weeks by 2,263 steps/d (39%) and 7.5 MVPA min/d (73%). There was no difference from baseline to 8-weeks for the UC group. There was a significant main effect for CR attendance in steps/d (CR: 7,770±1,432 vs. NCR: 4,779±1,371 steps/d, P<0.001).
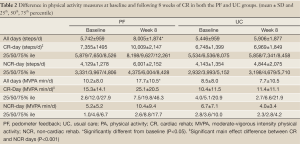
Full Table
Discussion
This is the first study to employ an individualized pedometer-driven PA intervention with patients beginning a maintenance CR program. The main study findings reveal that subjects in the PF group increased daily stepcounts by 42% (2,297±1,606 steps/d, P=0.001) from the first to the 8th week of CR, while no significant changes were found for UC subjects during the intervention period. Our results are similar to those from Hultquist et al. (11) who studied the efficacy of a 10,000 steps/d recommendation compared to 30 min/d MVPA in sedentary middle-aged women. At the end of the 4-week intervention, subjects in their pedometer group were accumulating significantly greater stepcounts than the time-based group (10,159±292 vs. 8,270±354 steps/d, P
All patients starting maintenance CR are prescribed 30-50 min/d of exercise during CR sessions, which can be observed by the ~3,000 steps/d difference between CR and NCR days at baseline in both groups. In addition to increases in overall daily stepcounts, the PF group in the present study significantly increased daily stepcounts during CR days over the course of the intervention by 36% (2,654±2,089 steps/d, P=0.003) and NCR days by 45% (1,872±2,026 steps/d, P=0.017). There were no significant changes in stepcounts for the UC group on CR days. This suggests the progressively increasing stepcount goal (adding 10% of baseline each week) encouraged the PF group to increase their PA more even more than they achieved during CR on days they attended CR.
Previous reports have showed that patients participating in a CR program
accumulate significantly greater stepcounts on days patients attend CR
compared to NCR days (7-9). Consistent
with these reports, subjects in the present study were observed to have
accumulated greater stepcounts on CR compared to NCR days. The 3-way
interaction between group-time-CR attendance for steps/day was not
significant, P=0.060 which suggests no advantage for the PF
group on NCR days. However, it is worth noting that the PF group had a 45%
increase in steps/d on NCR days by week 8 compared to an increase of only
17% in steps/d for the UC group. It is noteworthy to recognize that the PF
subjects averaged only 10.4±9.4 min of MVPA by week 8 on NCR days, which is
far short of the minimal goal of 30 min/d of MVPA. Thus, while using
pedometers with goals appear efficacious in increasing both steps/d and time
spent in MVPA, it is clear that greater efforts are necessary to further
increase PA levels of cardiac patients, especially on days they do not
attend CR programs. Although the subjects in the PF group increased the time
spent in MVPA, the 17.7±10.5 min/d at 8 weeks was still far short of the 30
min/d goal. Future efforts should explore if self-monitoring with pedometers
for longer than 8 weeks would be successful in patients reaching
Ayabe et al. (12) conducted the only other known pedometer intervention study in a maintenance CR program, by examining the effects using goals of either ≥10,000 steps/d or ≥30 min/d of MVPA. Both groups used pedometers to provide feedback and were instructed to accumulate either the targeted amount of steps or time of MVPA, and to monitor and record either the stepcounts or time. Both groups had significant increases in daily stepcounts throughout the 3-week intervention period, (step goal: 11,517±3,383 to 12,809±2,479, P=0.04; time goal: 10,810±3,211 to 13,355±3,498, P=0.004), however only the group monitoring the time spent in MVPA increased daily time spent in MVPA (36±11 to 52±15 min/d, P=0.008). Thus, it appears that using low-cost PA monitors, with capabilities to provide feedback to individuals, can be important tools to help cardiac patients increase their PA levels. Whereas, the Ayabe et al. (12) study cohort showed this in CR patients who already had an established maintenance CR program (attended maintenance CR ≥6 months and were obtaining ≥10,000 steps/d), the present study demonstrated the usefulness of PA monitoring feedback for helping patients beginning a maintenance CR program to increase their PA levels.
Results from the present study provide further support that short-term pedometer interventions can increase daily PA among overweight and older adults (15,18,19) and in those with clinical diagnoses (coronary artery disease, osteoarthritis, diabetes, and etc.) (16,20-22). The research design employed in the current study is similar to that of Croteau et al. (23), who provided subjects with individualized stepcount goals ranging from 5-10% above baseline values during an 8-week study. Subjects in that study averaging ≤8,000 steps/d at baseline were instructed to increase stepcounts each week by 10%, those averaging 8,000-10,000 steps/d were instructed to increase stepcounts each week by 5%, and those subjects averaging ≥10,000 steps/d were instructed to maintain current PA habits (19). Croteau et al. (23) reported that subjects instructed to increase daily stepcounts each week by 10% demonstrated the greatest increase in daily stepcounts 39.9% (2,272±1,473 steps/d) while subjects in the group instructed to increase daily stepcounts each week by 5% increased daily stepcounts by 24.9% (2,532±1,780 steps/d). Croteau et al.’s findings, combined with the present study’s results, suggest that increasing daily stepcount goals by 10%/week is an effective approach for increasing PA levels with individuals who are insufficiently active. Further research is warranted to assess if gender, clinical diagnoses (i.e. myocardial infarction, transplant, heart failure, and etc.) or other characteristics may influence this response. Although PA levels of subjects in the present study were increased more in the group using pedometers for feedback, it is important to recognize these patients were still not accumulating PA amounts suggested in national recommendations. Thus, for secondary prevention of coronary disease, it is important for healthcare professionals to recommend cardiac patients accumulate 30-60 minutes of MVPA daily and they should encourage patients to use pedometers.
Study limitations
While the present study provides evidence that a short-term pedometer-intervention may increase daily PA, the following limitations are noted. The PA intervention used in this study was relatively short (8 weeks). Although significant increases in PA levels were observed in the PF group, these patients were still not reaching PA goals on NCR days. The usefulness of pedometers can also be questioned since 27 of the patients eligible for the study either couldn’t use (orthopedic issues limiting ambulation) or were not interested in participation. The lack of interest could have been due, in part, to the daily requirement to wear a pedometer on their waistband. Additionally, of the 28 subjects eligible for study inclusion, 8 were not compliant with the protocol. Other known limitations associated with pedometers are that they do not measure non-ambulatory forms of PA and only models with an accelerometer mechanism can access time spent in MVPA. Finally, this pilot study had a relatively small sample suggesting the interpretation of the results warrant appropriate caution. Future studies with larger sample sizes, in multiple CR programs, and for longer time periods are needed.
Conclusions
Data from the present study provides further support of the benefits of pedometer use as a tool to help people increase their PA levels, including patients beginning a maintenance CR program. Pedometer-interventions can generally be administered with limited staff involvement and at little cost. CR programs should consider providing pedometers, with individualized stepcount goals, to patients entering a CR program to help them increase PA and ultimately meet recommendations for secondary prevention.
Acknowledgements
Thank you to the cardiopulmonary rehabilitation team at IU Health - Ball Memorial Hospital and research staff at Ball State University’s Human Performance Laboratory for their assistance in subject recruitment and data collection.
Disclosure: The authors declare no conflict of interest.
References
- US Department of Health and Human Services. 2008 physical activity guidelines for Americans. 2008. Available online: http://www.health.gov/PAGuidelines
- Hallal PC, Lee IM. Prescription of physical activity: an undervalued intervention. Lancet 2013;381:356-7. [PubMed]
- Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation 2005;111:369-76. [PubMed]
- European Association of Cardiovascular Prevention and Rehabilitation Committee for Science Guidelines; EACPR, Corrà U, et al. European Association of Cardiovascular Prevention and Rehabilitation Committee for Science Guidelines; EACPR, Corrà U, et al. Secondary prevention through cardiac rehabilitation: physical activity counselling and exercise training: key components of the position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur Heart J 2010;31:1967-74. [PubMed]
- Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 2011;124:2458-73. [PubMed]
- Wofford TS, Greenlund KJ, Croft JB, et al. Diet and physical activity of U.S. adults with heart disease following preventive advice. Prev Med 2007;45:295-301. [PubMed]
- Jones NL, Schneider PL, Kaminsky LA, et al. An assessment of the total amount of physical activity of patients participating in a phase III cardiac rehabilitation program. J Cardiopulm Rehabil Prev 2007;27:81-5. [PubMed]
- Savage PD, Ades PA. Pedometer step counts predict cardiac risk factors at entry to cardiac rehabilitation. J Cardiopulm Rehabil Prev 2008;28:370-7; quiz 378-9. [PubMed]
- Ayabe M, Brubaker PH, Dobrosielski D, et al. The physical activity patterns of cardiac rehabilitation program participants. J Cardiopulm Rehabil 2004;24:80-6. [PubMed]
- Bravata DM, Smith-Spangler C, Sundaram V, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007;298:2296-304. [PubMed]
- Hultquist CN, Albright C, Thompson DL. Comparison of walking recommendations in previously inactive women. Med Sci Sports Exerc 2005;37:676-83. [PubMed]
- Ayabe M, Brubaker PH, Mori Y, et al. Self-monitoring moderate-vigorous physical activity versus steps/day is more effective in chronic disease exercise programs. J Cardiopulm Rehabil Prev 2010;30:111-5. [PubMed]
- Butler L, Furber S, Phongsavan P, et al. Effects of a pedometer-based intervention on physical activity levels after cardiac rehabilitation: a randomized controlled trial. J Cardiopulm Rehabil Prev 2009;29:105-14. [PubMed]
- Carr LJ, Bartee RT, Dorozynski CM, et al. Eight-month follow-up of physical activity and central adiposity: results from an Internet-delivered randomized control trial intervention. J Phys Act Health 2009;6:444-55. [PubMed]
- Schneider PL, Bassett DR Jr, Thompson DL, et al. Effects of a 10,000 step per day goal in overweight adults. Am J Health Promo 2006;21:85-9.
- Marsh AP, Vance RM, Frederick TL, et al. Objective assessment of activity in older adults at risk for mobility disability. Med Sci Sports Exerc 2007;39:1020-6. [PubMed]
- Furber S, Butler L, Phongsavan P, et al. Randomised controlled trial of a pedometer-based telephone intervention to increase physical activity among cardiac patients not attending cardiac rehabilitation. Patient Educ Couns 2010;80:212-8. [PubMed]
- Richardson CR, Newton TL, Abraham JJ, et al. A meta-analysis of pedometer-based walking interventions and weight loss. Ann Fam Med 2008;6:69-77. [PubMed]
- Strath SJ, Swartz AM, Parker SJ, et al. A pilot randomized controlled trial evaluating motivationally matched pedometer feedback to increase physical activity behavior in older adults. J Phys Act Health 2011;8:S267-74. [PubMed]
- Richardson CR, Mehari KS, McIntyre LG, et al. A randomized trial comparing structured and lifestyle goals in an internet-mediated walking program for people with type 2 diabetes. Int J Behav Nutr Phys Act 2007;4:59. [PubMed]
- Talbot LA, Gaines JM, Huynh TN, et al. A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: a preliminary study. J Am Geriatr Soc 2003;51:387-92. [PubMed]
- de Blok BM, de Greef MH, ten Hacken NH, et al. The effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: a pilot study. Patient Educ Couns 2006;61:48-55. [PubMed]
- Croteau KA. A preliminary study on the impact of a pedometer-based intervention on daily steps. Am J Health Promot 2004;18:217-20. [PubMed]


