Warfarin and aspirin for primary prevention in patients with heart failure in sinus rhythm
Lala and co-workers (1) have argued that “while aspirin therapy decreases incident cardiovascular events, it also increases risk of major bleeding and hemorrhagic stroke”, and so “the benefit to risk ratio for aspirin use in primary prevention of cardiovascular events is less clear”. Heart failure (HF) in sinus rhythm is thought to be an indication for primary prevention not only with aspirin but also with warfarin, but this point has not been addressed in Lala’s article. Since aspirin and warfarin for patients with HF in sinus rhythm are an important therapeutic option particularly in the framework of individualized approaches, we have expanded the analysis of the evidence available in this area.
According to a meta-analysis based on 4 studies (2), aspirin and warfarin are equi-effective in reducing mortality in patients with HF in sinus rhythm. However, as compared with aspirin, the therapeutic profile of warfarin is more “unbalanced” because warfarin reduces to a greater extent than aspirin the incidence of ischemic stroke, but increases major bleedings. As a result, aspirin might be more appropriate in patients with high risk of bleeding, whereas warfarin could be preferred in patients with high thromboembolic risk.
To better define the place in therapy of these two agents, conducting further studies comparing warfarin vs. aspirin in unselected patients has been proposed (2); however, an open question remains on whether new studies in unselected patients can still be useful or, conversely, other comparative designs based on more selective enrolment criteria can be better. Therefore, we have addressed this issue by applying trial sequential analysis (TSA) (3,4).
Our TSA included the same 4 trials examined by Rengo et al. (2) Our assumptions included two-sided testing, type 1 error =5%, power =80%. With respect to death rate from any cause, the intervention effect was set at relative risk reduction =15% with respect to 21% absolute event rate in the controls (equal to overall rate in the 4 aspirin arms). As usual, the main result of TSA was expressed through the graph of cumulative z-curve; the boundaries for concluding superiority or inferiority or futility in this graph were calculated according to the O’Brien-Fleming alpha-spending function. All calculations were carried out using a specific statistical software (TSA, User Manual for TSA, Copenhagen Trial Unit 2011, software downloadable at www.ctu.dk/tsa).
Our results are shown in Figure 1. Although the analysis estimated that 4,953 patients would be needed to conclusively demonstrate superiority or inferiority or futility, at the cumulative number of 3,663 patients (i.e., those enrolled in the 4 trials) the curve had already crossed the green boundaries and was in the futility area.
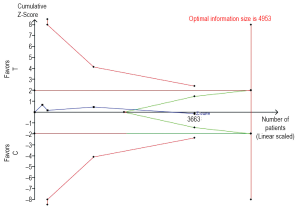
This finding is a sound proof that the results by Rengo et al. (2) are conclusive, but-more importantly-specific clues can be obtained from our results about the optimal design of future trials in this area. In fact, further comparative studies in unselected patients seem to be useless because of this statistical demonstration of futility; on the other hand, there seems to be the need for further comparative studies based on the enrolment of select subpopulations (e.g., those with high risk of bleeding or with high thromboembolic risk). In this framework, appropriate comparators might include not only warfarin and aspirin, but also the novel oral anticoagulants because of their potential advantages in patient management (5).
In conclusion, designing new trials in this area is becoming increasingly complex, and so the identification of futile designs for future primary prevention studies can be of value. On the other hand, if future studies in primary prevention are aimed (as indicated by our analysis) at more selective uses of known agents, this approach will also contribute to improve individualisation of treatments in this area.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lala A, Hiatt WR, Berger JS. Aspirin in primary prevention: can we individualize care? Cardiovasc Diagn Ther 2012;2:169-72.
- Rengo G, Pagano G, Squizzato A, et al. Oral anticoagulation therapy in heart failure patients in sinus rhythm: a systematic review and meta-analysis. PLoS One 2013;8:e52952. [PubMed]
- Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 2008;61:64-75. [PubMed]
- Wetterslev J, Thorlund K, Brok J, et al. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol 2009;9:86. [PubMed]
- Gheorghiade M, Vaduganathan M, Fonarow GC, et al. Anticoagulation in heart failure: current status and future direction. Heart Fail Rev 2012. [Epub ahead of print]. [PubMed]


