Intraarticular extravasation, an unusual complication of computed tomographic angiography performed with intraosseous needle intravenous access
Introduction
Intraosseous needle (ION) intravenous access (IVA) is a rapid and safe alternative for central venous access that is frequently utilized by paramedics and emergency medicine personnel for patients in shock. This is particularly useful in patients with obesity or chronic intravenous drug use that make conventional peripheral venous access more difficult (1). Many of the patients who receive ION require computed tomographic angiography (CTA) during the course of their emergency medical care. There is an increasing awareness on the use of ION IVA for contrast media (CM) injection during CTA, predominantly from animal studies or small case series (2-9). Until now, there have been no complications of this technique reported. However, complications, such as the one discussed herein, related to new procedures are important to report, so that recommendations and procedural techniques can be modified to ensure that they are a rare occurrence.
Case presentation
A 66-year-old obese female presented to the emergency department after a traumatic fall and was found to have signs and symptoms of an acute stroke. Both trauma protocol and stroke protocol imaging were requested. Multiple attempts to achieve IVA via peripheral access veins failed and an intrahumeral IVA was subsequently achieved with an ION (Arrow® EZ-IO® Intraosseous Vascular Access System, Teleflex Medical, Limerick, Pennsylvania, USA).
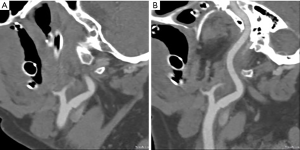
Prior to use of ION IVA for CM injection, the needle position was confirmed by non-contrast computed tomography (Figure 1). Suitability of the access was further assessed with a 40 mL saline flush at 3.5 mL/sec. Subsequently, CTA of the head, neck, thorax, abdomen, and pelvis was performed with a Somatom Definition Edge scanner (Siemens Healthcare, Forchheim, Germany); 80 mL of Iohexol 350 (Omnipaque, General Electric Healthcare, Little Chalfont, United Kingdom) CM was injected at 3.5 mL/sec for the CTA of the head and neck, and 100 mL for the thorax, abdomen, and pelvis. Significant acute traumatic injury was ruled out, and the arterial circulation was free of stenosis or thrombus (Figure 1).
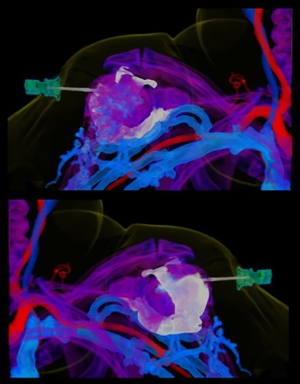
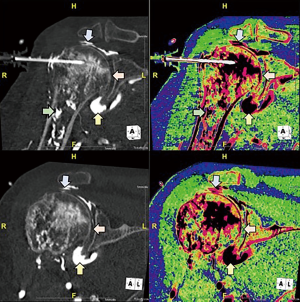
Curiously, at the time of scanning approximately 20 mL (approximated with voxel-based morphometry) of CM was seen within the glenohumeral joint. During further off-line analysis (Aquarius Intuition, Terarecon, Foster City, CA, USA) CM could be seen passing a small distance retrograde along the path of the ION into the subdeltoid bursa, moderately distending the bursa and joint capsule (Figures 2-4). Fortunately, the patient denied post procedural pain, and physical exam failed to reveal a neurological or vascular deficit, either immediately after the scan, the following day or at 1-week follow-up.
Discussion
In this case report, we describe contrast extravasation into the glenohumeral joint and associated bursae as a newly identified complication from ION. We believe that this unusual complication occurred because humeral ION can pass through the subdeltoid bursa during placement. Contrast passing retrograde along the ION tract could then enter the joint space via its connection to the bursa. However, in this case a cause for the retrograde flow could not be ascertained by inspection of the CT data, as needle position appeared to be optimal on both a scout pre-contrast scan and on the CTA. One possible explanation is that a subtle change occurred in the orientation of the needle driver during ION placement. This could have resulted in widening of the needle tract (at least microscopically) without damaging the needle. If so, then it becomes even more important for operators to maintain a straight course during ION placement to reduce the risk for this complication. Another possible explanation is that contrast passed directly into the joint space through an interruption in the periarticular bone. As the patient’s bone appears intact and its mineralization appears to be normal, we believe this is a less likely etiology.
To conclude, we believe this intraarticular extravasation of CM during CTA examinations may be unique to ION IVA. Now that it has been reported, others can recognize it and a greater understanding of the incidence can be ascertained. We hope this complication will prove to be rare and simply a curiosity. However, as ION IVA for CTA is becoming more routine, imaging specialists should be aware of this risk and monitor patients who experience it for both short term and delayed adverse sequelae, such as joint space infection or adhesive bursitis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: For this case report, which utilizes deidentified radiographic images, the authors’ institutional review board did not require informed consent.
References
- Petitpas F, Guenezan J, Vendeuvre T, et al. Use of intra-osseous access in adults: a systematic review. Crit Care 2016;20:102. [Crossref] [PubMed]
- Günal I, Köse N, Gürer D. Compartment syndrome after intraosseous infusion: an experimental study in dogs. J Pediatr Surg 1996;31:1491-3. [Crossref] [PubMed]
- Cohen J, Duncan L, Triner W, et al. Comparison of Computed Tomography Image Quality Using Intravenous vs. Intraosseous Contrast Administration in Swine. J Emerg Med 2015;49:771-7. [Crossref] [PubMed]
- Winkler M, Talley C, Woodward C, et al. The use of intraosseous needles for injection of contrast media for computed tomographic angiography of the thoracic aorta. J Cardiovasc Comput Tomogr 2017;11:203-7. [Crossref] [PubMed]
- Baadh AS, Singh A, Choi A, et al. Intraosseous Vascular Access in Radiology: Review of Clinical Status. AJR Am J Roentgenol 2016;207:241-7. [Crossref] [PubMed]
- Schobinger RA. Intra-osseous Venography. New York: Grune & Stratton, 1960.
- Knuth TE, Paxton JH, Myers D. Intraosseous injection of iodinated computed tomography contrast agent in an adult blunt trauma patient. Ann Emerg Med 2011;57:382-6. [Crossref] [PubMed]
- Ahrens KL, Reeder SB, Keevil JG, et al. Successful computed tomography angiogram through tibial intraosseous access: a case report. J Emerg Med 2013;45:182-5. [Crossref] [PubMed]
- Budach NM, Niehues SM. CT angiography of the chest and abdomen in an emergency patient via humeral intraosseous access. Emerg Radiol 2017;24:105-8. [Crossref] [PubMed]
- Winkler M, Issa M, Lowry C, et al. Volume rendered cine clip utilizing pseudocolor multimasking of right shoulder showing the intraosseous needle, CM within the intramedullary space, and contrast within the glenohumeral joint capsule. Asvide 2018;5:679. Available online: http://www.asvide.com/article/view/26385


