
Effectiveness of health education-based conventional intervention method to reduce noncommunicable diseases risk factors among rural population
Introduction
The current world is facing a remarkable burden of Noncommunicable diseases (NCDs), mainly cardiovascular diseases, cancers, chronic respiratory diseases and diabetes that is the major public health challenge. Annually, NCDs are responsible for 70% of all global deaths and it is 67% in case of Bangladesh (1,2). Around 15 million premature deaths (aged between 30–69 years) occur due to NCDs, whereas 80% of its deaths occur in the low- and middle-income countries, like Bangladesh (1).
However, relationship of some of the behavioral risk factors (mainly tobacco use, physical inactivity, harmful use of alcohol, unhealthy diet and excessive dietary salt intake) has been established with the development of NCDs. These behavioral risk factors lead to four metabolic immediate risk factors (such as raised blood pressure, overweight/obesity, hyperglycemia and hyperlipidemia), and these eventually lead to various kinds of NCDs (1). Yearly, significant proportions of global deaths are attributed to these individual risk factors (3).
In Bangladesh, these behavioral risk factors have already been posed remarkably. In terms of prevalence, there are 44% tobacco users, 93% people intake insufficient fruit and vegetables (<5 servings/day), 38% adults found with low level of physical activity [<600 metabolic equivalent (MET)/week], and it has also been observed that 38% have at least three risk factors in together when clustering nature of the risk factors were examined (4). Again, 72% people are habituated with added salt use during their meal (5). Moreover, this scenario is more prominent among the Bangladeshi rural population (6).
This alarming circumstance indicates that appropriate cost-effective intervention programs are essential for Bangladeshi population intending to the prevention and control of NCD risk factors. As Bangladesh have the scarcity of resources, especially in rural area it is mandatory to take in consideration the cost-effective strategies and interventions like conventional methods with health education to avert NCD risk factors which wasn’t covered by any study. The present study aimed to assess the effectiveness of health education-based message using conventional methods to reduce the NCD risk factors in a selected rural area.
Methods
Study design and settings
It was a quasi-experimental study, conducted in Basulia in 2017. Basulia is a small village of Narayanganj district, about 18 kilometers away from the capital city Dhaka. The village was selected purposively. Around 350 adult people were living in the village. The whole village was divided into 4 clusters on the basis of imaginary lines, and finally 1 cluster was selected randomly. All of the adult people aged between 18–65 years of the selected cluster were recruited in this study, therefore the total participants were 81.
Pre-test, intervention and post-test
A baseline pre-test was done before intervention. The intervention was on health education in terms of awareness creating and warning messages on NCDs with their risk factors, given to the participants in a specific interval for the duration of 3 months. The health education messages were on the major NCDs with their burden, behavioral risk factors of NCDs such as tobacco use, harmful use of alcohol, unhealthy diet, physical inactivity and added salt intake, whereas the messages reflected the harmful consequences and healthy practices. The messages were built using the information and statistical data from the official website of World Health Organization and Bangladeshi national level documents. Weekly one leaflet (total 12) was provided to the participants by well-trained volunteers. The messages were translated into easily understandable Bengali language, moreover the volunteers clarified the messages especially to the illiterate participants. Among the 12 messages, 2 were on insufficient fruit and vegetables intake, 2 were on excessive dietary salt and high salt content processed food intake, 1 was on tobacco consumption (smoking and smokeless both), 1 was on alcohol consumption, 1 was on inadequate physical activity and remaining 5 were combined with all of these risk factors. The post-test was done after completion of intervention.
Data collection instrument and process
A semi-structured questionnaire was developed using WHO STEPS Instruments (version 3.1), which comprised of socio-demographic factors (age, sex, education and occupation) and behavioral risk factors of NCDs (tobacco use, harmful use of alcohol, unhealthy diet, physical inactivity and added salt intake). STEPS show-card was used to assess the fruit and vegetables intake servings (1 standard serving =80 grams) and to demonstrate the physical activity related questions. Physical activity was measured in MET following WHO standard method. Fruit and vegetables intake was defined as insufficient when it was <5 servings/day together and physical activity was defined as inadequate level when it was <600 MET/week (according to WHO recommendation of fruit and vegetables intake and physical activity). Data were collected by face-to-face interview.
Statistical procedures
SPSS software version-21 was used for data analysis. Descriptive statistics was used to illustrate the socio-demographic factors and behavioral risk factors and comparative statistics (paired sample t-test) was used to illustrate the significance of pre and post-test difference in terms of effectiveness of intervention.
All of the ethical issues related to biomedical research involving human subjects relevant to this study were maintained accordingly. There was no invasive procedure. Ethical approval has been taken from the Ethical Review Committee of State College of Health Sciences (SCHS), Dhaka, Bangladesh. Both verbal and written informed consents were taken from each participant prior to data collection.
Results
One participant was dropped out from the intervention and follow-up; therefore, the total completed participants were 80. Among them, men were dominator (60%) and the mean age was 37.1±13.8 years. Majority of the participants were primary school passed (up to fifth class) and housewife (Table 1).
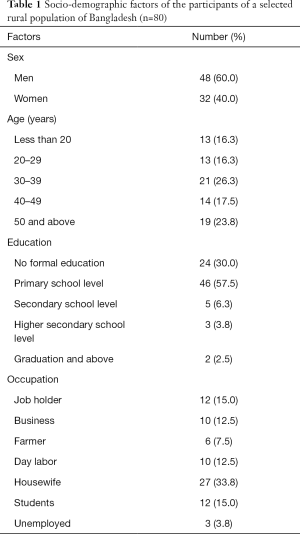
Full table
Current study found significant pre- and post-test differences for daily mean number of smoking tobacco sticks, daily mean frequency of smokeless tobacco use, daily mean servings of fruit and vegetables intake, daily mean amount added salt intake and weekly mean of total MET value (Table 2).
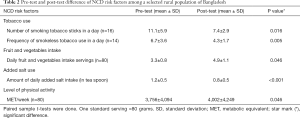
Full table
Moreover, the proportion of sufficient fruit and vegetables consumers was increased from 3.8% to 40.0%, the proportion of added salt users was decreased from 92.5% to 88.7%, the proportion of adequate level of physical activity performers was increased from 83.3% to 90.0%. However, the proportion of tobacco users (37.5%) was remained the same. Similar statistics was also found for the proportion of alcohol users (6.3%), although all were occasional users (not shown in table).
Discussion
Current study was a paradigm of cost-effective interventions with conventional method like health education-based leaflet to reduce the NCD risk factors among the rural population in low-resource settings of the world. Study evinced an excellent impact on increasing the proportion of sufficient fruit and vegetables consumers along with mean number of servings, which was similar to a study conducted with motivational interventions among African Americans (7). Although this study didn’t report significant impact on proportion of tobacco users likely to the study with effectiveness of health promotion campaigns for healthy lifestyle conducted in rural Vietnam (8), yet daily mean number of smoking tobacco sticks and mean frequency of smokeless tobacco use were significantly decreased. Study showed positive impact on lowering added salt use reflecting similar results from Vietnamese health promotion campaigns (8).
In a conclusion, health education-based intervention using leaflets as conventional method was effective to reduce NCD risk factors among the selected rural population of Bangladesh. This method can be recommended as a promising strategy in various health awareness programs to reduce NCD burden especially in the low-recourse settings. However, broad spectrum randomized control trials are also needed to assess the effectiveness more efficiently.
Acknowledgements
We acknowledge the respondents who participated in this important study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval has been taken from the Ethical Review Committee of State College of Health Sciences (SCHS), Dhaka, Bangladesh. Both verbal and written informed consents were taken from each participant prior to data collection.
References
- World Health Organization. Noncommunicable diseases fact sheets. Accessed on January 9, 2018. Available online: http://www.who.int/mediacentre/factsheets/fs355/en/
- World Health Organization. Noncommunicable diseases progress monitor 2017. Accessed on December 22, 2017. Available online: http://apps.who.int/iris/bitstream/10665/258940/1/9789241513029-eng.pdf
- GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659-724. [Crossref] [PubMed]
- Zaman MM, Bhuiyan MR, Karim MN, et al. Clustering of non-communicable diseases risk factors in Bangladeshi adults: An analysis of STEPS survey 2013. BMC Public Health 2015;15:659. [Crossref] [PubMed]
- Mondal R, Sarker RC, Banik PC, et al. Knowledge, attitude and behavior towards dietary salt intake among Bangladeshi population. SMU Med J 2017;4:170-8.
- Banik PC, Zaman MM, Ahmed J, et al. Prevalence of risk factors of non-communicable diseases in an adult population of rural Bangladesh. Cardiovasc J 2018;10:126-34. [Crossref]
- Resnicow K, Jackson A, Wang T, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life trial. Am J Public Health 2001;91:1686-93. [Crossref] [PubMed]
- Nguyen QN, Pham ST, Nguyen VL, et al. Effectiveness of community-based comprehensive healthy lifestyle promotion on cardiovascular disease risk factors in a rural Vietnamese population: a quasi-experimental study. BMC Cardiovasc Disord 2012;12:56. [Crossref] [PubMed]


