
Integrating the development agenda with noncommunicable disease prevention in developing countries: a quasi-experimental study on inter-sectoral action and its impact on self-reported salt consumption—the INPARD study
Introduction
Noncommunicable diseases (NCDs) are the most common cause of death globally and deaths attributed to NCDs are continuing to increase at an alarming rate (1). According to the WHO in 2016, NCDs caused 71% of deaths worldwide, ranging from 37% of total deaths in low-income countries to 88% in high-income countries. All but one of the 10 leading causes of death in high-income countries were NCDs. In terms of absolute number of deaths, over 80% of global NCD deaths occurred in low- and middle-income countries (2,3). Of these NCDs, cardiovascular diseases (CVD) are responsible for the greatest number of deaths, around 17.9 million worldwide in 2015, demonstrating a 12.5% rise since 2005 (1). CVD mortality is of particular concern in South Asian countries, in which deaths from CVD have increased at a higher rate than in other global regions (4,5).
This global burden of NCDs has been recognized at many high level meetings. Within the Global Action Plan on NCDs (GAP), adopted in 2011, countries of the United Nations agreed to reduce premature mortality due to NCDs by 25% by 2015 (6). The GAP focuses on four main NCDs: cardiovascular diseases, cancers, chronic respiratory diseases and diabetes (6), calling for reductions in their modifiable risk factors, which include tobacco and alcohol use, salt intake, obesity and raised blood pressure (7). In support of this, the Sustainable Development Goals (SDGs), set by the United Nations in 2015 to succeed the Millennium Development Goals, included a target (SDG 3.4.l) of a 30% reduction of premature mortality due to NCDs by 2030 under Goal 3 ‘Good Health and Wellbeing’ (8).
Achieving these targets is currently thought to be difficult in many parts of the world (9). Reductions in these modifiable risk factors, that are either unhealthy behaviours or occur as a result of them, need to be supported by changes to the environments which created them. For example, changes to dietary intake on a population level, would require environmental modifications that encourage and enable individuals to make healthy choices. Such modifications could include improving the affordability of healthy foods and reducing the availability of unhealthy items, amongst many others. Such modifications commonly lie outside of health sector responsibility and can only be sustained through changes in the socio-economic environment (10). Such change will require working with a range of sectors other than health, such that modifications can occur throughout the policy and social environment. Understanding how to work with agriculture, rural development and local industries, amongst other sectors, is therefore essential in achieving SDG 3.4 l.
One such diet related risk factor is hypertension, which is recognized as one of the most important modifiable NCD risk factors as it leads to many macrovascular complications, including atherosclerotic heart disease and cerebrovascular disease (11,12). Reductions in salt consumption have consistently been shown to reduce blood pressure among both healthy and hypertensive individuals (13,14). In order to prevent hypertension, the World Health Organization (WHO) recommends that individuals consume no more than 5 grams of salt each day (15). However, more recent data suggest that most populations appear to have mean sodium intakes well in excess of 100 mmol per day, which is roughly equal to one teaspoon full of salt (table salt 6.1 g per day). Sodium intake in men is greater than in women, most likely reflecting the higher food consumption among men, although it appears to be slightly lower above the age of 50 years (16).
These high levels of salt consumption are particularly common in Asian countries. The average daily intake of salt in Sri Lanka in 2012 was estimated to be 11.4 g of salt per person (17). Salt is added to many Sri Lankan dishes at the time of preparation. In addition, dried and salted fish, canned fish, traditional pickles and sambols which contain large amounts of salt, are widely consumed. Some dietary habits, common throughout Sri Lanka, such as adding salt to rice also increase salt consumption. It is little surprise, therefore, that hypertension within Sri Lanka is also found to be high. A population survey of cardiovascular risk factors in the country in 1998–2002 found that the age-standardized prevalence rate for hypertension (defined as systolic blood pressure ≥140 mmHg and diastolic pressure ≥90 mmHg) was 19%, with little difference between men and women (18). A national survey by Katulanda et al. in 2005–2006 reported a national prevalence of hypertension in adults of 13% in men and 14% in women (19).
The current Sri Lankan economic development policy aims to lay the foundation to establish a more sustainable economic strategy in the country. The World Bank, International Monetary Fund, the Asian Development Bank, as well as other donor agencies in Europe, Japan, and the United States of America have come forward once again to extend loans at concessional interest rates to the Sri Lankan Government, with the aim of expanding and strengthening the economy (20,21). These initiatives will improve the individual and national economy. However, for this development to be sustainable, it is important to have a healthy workforce. This will require minimizing the negative consequences of economic development and urbanization. Evidence and strategies are required to promote health, including dietary modification, in this era of rapid economic development in the country. These lessons could also be useful for many other low and middle-income countries which are going through a similar process.
The aim of this study was to investigate whether a multisectoral approach to nutrition promotion could be integrated into a rural development programme within Sri Lanka. Throughout the paper we describe the methods and results of the Integrating Nutrition Promotion and Rural Development (INPARD) programme which was implemented in the country, alongside a large World Bank funded rural development programme called the Re-Awakening Project (RaP). The key intervention of this study was to facilitate collaboration between a number of government organizations to integrate NCD prevention approaches in the RaP project. In this paper we discuss the outcomes with regards to the impact on self-reported salt consumption.
Methods
INPARD project
At the inception, the INPARD project organized workshops with national level stakeholders to develop an interventional strategy and identify national and ground level stakeholders. These stakeholders included the Ministries of Health, Nutrition and Indigenous Medicine; Economic Development and Education; the Department of Agriculture; the National Nutrition Secretariat of Sri Lanka and partner universities; amongst others. Meetings were also held at district and divisional levels to develop local collaboration between sectors and stakeholders.
Village Development Organizations (VDOs) were selected as the focal points to coordinate INPARD activities in intervention areas. These VDOs were formed as part of the RaP project, with the participation of the residents of each village and were facilitated by the Economic Development Ministry (EDM). VDOs are micro-finance organization that are owned by the villagers and fund small-scale industries on a low-interest loan basis. The RaP project facilitates this process by providing technical assistance, developing marketing strategies and directing those receiving the loans to relevant agencies or ministries.
Community lead intervention
The INPARD team used data from recently completed studies in intervention areas, along with baseline survey data collected by INPARD researchers, to identify health promotion priorities. To supplement this quantitative data, INPARD team members also met with stakeholders at village and district levels, conducting workshops, focus groups and interviews with key stakeholders. Findings from this process were reviewed with national and regional level experts to prioritize key themes for interventions. These key themes included promoting multisectoral actions, training multisectoral teams at village, district, provincial and national levels. Nutritional priorities identified by stakeholders and data collection included increasing consumption of fruits and vegetables, reducing consumption of unhealthy bakery products and sweets and increasing the proportion of protein rich food in diets. A key focus, identified in one district, Ampara, was to reduce salt consumption.
Members of local communities and VDOs identified local priorities. Each village, through the VDO and with multisectoral stakeholders, created an action plan with activities feasible and relevant to their priorities. Actions were identified, planned and implemented by the local communities and thus individualized to the local needs. Examples of activities included cooking sessions conducted to reduce salt in daily cooking, use of locally available but not commonly utilized plant based products; changing foods available in school canteens; training residents to create small businesses producing healthy foods to be supplied to school canteen and local shops; promoting home and school gardening and working with fishery societies to increase the availability of fish in local villages. Individuals who had received multisectoral support, through training or other means and whose business plan was seen to target the local nutrition needs were then prioritized by the VDO to receive micro-finance loans. Multisectoral stakeholders guided these individuals to establish and operate the businesses. They were provided with assistance to register their business and obtain other clearance and certificates. Finally they were supported in to distributing and marketing the product.
Evaluation
This study adopted a cluster randomized controlled quasi-experimental approach with a follow up period of 1 year, conducted in three rural districts of Sri Lanka: Monaragala, Ampara and Kurunegala. Sampled clusters were villages (also called Grama Niladhari Areas) which are the smallest administrative divisions in Sri Lanka. The RaP project was active in select villages in two districts, Monaragala and Ampara. From each of these districts 20 intervention villages, which were part of the RaP project were selected for this study, along with 10 control villages, which were not included in the RaP project for controls. A total of 10 villages were also selected in Kurunegala to act as controls. The RaP project was not active in this region and villages were also selected here to control for any contamination of the RaP project between villages in districts in which RaP was active.
An evaluation was carried out to investigate the inputs, outputs, outcomes and impacts of the intervention using the logic model (22). Both quantitative and qualitative assessments of dietary practices, lifestyle and health awareness were carried out. In this paper we report results of the quantitative surveys focusing on dietary salt consumption.
Data collection
We collected data at baseline and post intervention, 1 year apart, in 20 households selected randomly from the electoral lists in all sampled villages. Data were collected from two adults in each household, using trained interviewers. Two questionnaires were completed with each participant: (I) The World Health Organization (WHO) STEPwise survey (23) included basic demographic and health information, along with anthropometric measurements, that has been validated and adapted for the Sri Lankan population in previous data collections; and (II) a food frequency questionnaire (FFQ) which is validated for use with Sri Lankan adults (24). Measures of salt consumption were obtained from the FFQ, general questions on habits that increase salt consumption and the monthly salt consumption in the household were collected in the WHO STEPS survey. This study was approved by the Ethics Review Committee (ERC) of the University of Colombo Faculty of Medicine (UCFM), Sri Lanka.
Analysis
Data were analyzed using the statistical program STATA version 13 (StataCorp. 2013. Stata Statistical Software. Release 13. College Station, TX: StataCorp LP). Unless stated otherwise, an overall P<0.05 was considered significant. Chi squared test was used to compare dichotomous and categorical variables. Student’s t test was used to compare continuous variables. For logistic regression analysis we used high salt intake as a dichotomous outcome variable. This was defined as having a mean daily consumption of more than 5 grams of salt a day and was calculated from FFQ data. We calculated five regression models: Model (I) univariable baseline, (II) multivariable baseline, (II) univariable follow-up, (IV) multivariable follow-up and (V) multivariable follow-up controlling for baseline high salt consumption. We report odds ratios with 95% CIs, reference categories, where not explicitly described are the binary opposition, i.e., for unemployed the reference category is all employed measures aggregated.
Results
Out of the 1,628 participants, more than 60% were female in both intervention and control areas, with more than 80% aged between 20 and 60 years. Over two thirds had reached secondary school grade 10 level or above and the mean BMI was just under 23 kg/m2. Dyslipidemia was the most common CVD risk factor, and more than 20% of the total sample reported to have had more than one CVD. Over 10% of the sample in intervention and control areas reported to have hypertension (Table 1).
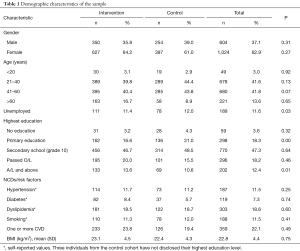
Full table
Around 14% of individuals added salt at time of eating, with this increasing in control areas only. Over 90% of individuals added salt to rice whilst preparing it pre-intervention, with decreases in this in both control and intervention areas post-intervention. There was an increase in the consumption of high salt processed foods over this time, although the relative increase was less in intervention areas. The average salt consumption was 13.3 g/day in control areas and 14.3 g/day in interventional areas at baseline. With slight decreases in both post intervention. Reduced mean levels were still more than twice the recommended 5 g/day of salt (Table 2).
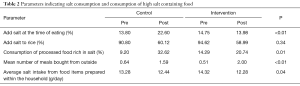
Full table
In baseline univariable models, individuals who were older than 50 years (OR =1.5; 95% CI=1.2, 1.8) and those living in Ampara district (OR =1.6; 95% CI =1.3, 2.0) had higher odds of salt consumption compared to those younger than 50 years and those residing in Kurunegala respectively. Those with a higher education had lower odds of consuming more than five grams of salt a day. These associations remained significant in baseline multivariable models, when controlling for all variables.
Models using post-intervention high salt intake as an outcome found that those living in Ampara had significantly lower odds of high salt consumption, in all models: univariable, multivariable and multivariable controlling for baseline salt intake (OR =0.6; 95% CI =0.4, 0.9). Those who were unemployed had significantly higher odds of high salt intake in all post-intervention models (Table 3).
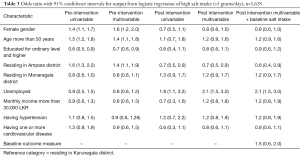
Full table
Discussion
This paper describes a quasi-experimental real world study, on a community led multisectoral intervention for nutrition promotion. The key findings indicate a reduction in high salt consumption in communities that identified it as an issue pre-intervention. This is one of the first published studies presenting evidence of the benefits of a multisectoral approach. Many community groups in Ampara district identified high salt intake as a primary concern and salt reduction was given more emphasis in multisectoral nutrition promotion in that area. It is interesting to note that the association of poor educational status with high salt consumption that was seen in baseline data disappeared after the intervention, however, those without employment were more likely to consume high levels of salt compared to those in employment post intervention, despite no significant association found by employment status in baseline models. It is possible that confounding has occurred here, with income and employment being strongly linked, but future work should consider the differing impact of these approaches on those with different employment, education and income status.
The findings emphasize the importance of addressing the underlying environmental and behavioural factors that lead to an unhealthy behaviour. As in this study, an intervention on salt reduction should not only include education on salt reduction but also address cooking skills along with reducing the local availability of high salt food in places like school canteens. Minimizing salt content in the entire food supply is critical to facilitate consumers to have a lower salt consumption. Engaging with a range of stakeholders and the community is also key to such multisectoral approaches.
Population health and nutrition are influenced by a wide spectrum of social determinants that lie outside of the health sector. It is crucial therefore that a range of sectors consider the health of the nation in their policies, this includes but is not limited to education, agriculture and development (25). The international development agenda has been strongly supported globally, but until recently it did not consider health as a primary agenda, despite the health of the population being essential for the development of a country’s socioeconomic environment. The SDGs, published in 2015, not only set health as one of the 17 goals, including targets for infectious and NCDs along with health system capacity, it also called for global and local multi-stakeholder partnerships to achieve success. Although such multisectoral approaches have been widely discussed, there is a limited amount of data available in the scientific literature to support such an approach, with the evidence of any successful working often limited to case examples (26). These include those advocating for multisectoral approaches to encourage healthy and sustainable nutrition (27).
The present study supports the move to consider health within the development agenda; it also provides support for involving development and other sectors in population and community-level health promotion. Such a principle, although increasingly accepted, is yet to be streamlined into the planning and evaluation of development policies and programmes, especially in LLMICs, such as Sri Lanka. It is hoped that as the evidence base on the effectiveness and practicality of such approaches improves, that they become central to both development and health policies.
Limitations
Despite the study having a number of strengths, it also had a number of limitations, many of which highlight the difficulties in conducting pragmatic trials in real world settings. As INPARD was community led, the multi-sectoral interventions were heterogeneous between communities. It is therefore difficult to identify which aspects of the intervention were effective in improving health outcomes. In addition we report behaviour associated with high salt intake and an estimate of salt consumption per person based on self-report responses to the STEPwise survey and a FFQ respectively. These proxy measures are not as accurate as objective measurements of urinary salt concentration, which although more accurate are difficult to employ at community level interventions. Although accuracy of self-reported dietary data is questioned (28) many authors have established a satisfactory correlation between actual salt consumption and self-reported values (29,30). The FFQ used in this study, although validated was not specifically tested for estimated salt levels against urinary salt concentrations. It is possible that the results of this study may be influenced by factors such as increasing self-awareness, leading to report bias in participants. Finally as this study evaluated an intervention in a real world setting, the results may be susceptible to contamination both between intervention and control groups and by other interventions in the regions in which the study was carried out. The duration of the study also meant we were limited to assessing short and medium term outcomes such as dietary salt intake, rather than cardiovascular disease outcomes.
Conclusions
The importance of working with the development sector to promote NCDs has been recognized for a long period of time. The Global Action Plan for the Prevention and Control of NCDs recognized this approach under its first objective. Yet, there has been very little published literature on evaluating such approaches in the real world. This paper demonstrates that it is feasible to work alongside rural development projects to address NCD risk factors and prevent NCDs. In this study, we demonstrated that community level inter-sectoral actions can have an impact on self-reported salt consumption. The key elements of the interventions are community empowerment to establish a multisectoral team, community driven problem identification and development and implementation of multisectoral actions. This study shows that rural development programmes can collect such data (salt consumption and NCD relevant data) when they are provided with appropriate protocol, guidance and training. Therefore future development projects can have specific aims to address diet and NCD risk factors with a strong framework for monitoring and evaluation.
Acknowledgements
This work was funded by the South Asia Food and Nutrition Security Initiative (SAFANSI) of the World Bank. The INPARD investigators would like to thank the staff of the INPARD program including the program coordinator Mr. Chamil Senaviratne, staff of the ministry of the Economic Development and Re-awakening project, Ministry of Health Nutrition and welfare, Ministry of Agriculture, district secretariats or Ampara, Monaragala and Kurunegala and Grama Sewaka Niladhari officers of study areas.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Ethics Review Committee (ERC) of the University of Colombo Faculty of Medicine (UCFM), Sri Lanka.
References
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-544. [Crossref] [PubMed]
- Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart 2016;11:393-7. [Crossref] [PubMed]
- World Health Organization. Fact Sheets - Noncommunicable Diseases. 2018. Available online: http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
- Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ 2004;328:807-10. [Crossref] [PubMed]
- Misra A, Tandon N, Ebrahim S, et al. Diabetes, cardiovascular disease, and chronic kidney disease in South Asia: current status and future directions. BMJ 2017;357:j1420. [Crossref] [PubMed]
- Organization WH. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013. Geneva: World Health Organization, 2015.
- Kontis V, Mathers CD, Rehm J, et al. Contribution of six risk factors to achieving the 25× 25 non-communicable disease mortality reduction target: a modelling study. Lancet 2014;384:427-37. [Crossref] [PubMed]
- Griggs D, Stafford-Smith M, Gaffney O, et al. Policy: Sustainable development goals for people and planet. Nature 2013;495:305. [Crossref] [PubMed]
- Kontis V, Mathers CD, Bonita R, et al. Regional contributions of six preventable risk factors to achieving the 25×25 non-communicable disease mortality reduction target: a modelling study. Lancet Global Health 2015;3:e746-57. [Crossref] [PubMed]
- Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science 1998;280:1371-4. [Crossref] [PubMed]
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-324. [Crossref] [PubMed]
- Carey RM, Whelton PK. The 2017 American College of Cardiology/American Heart Association Hypertension Guideline: A Resource for Practicing Clinicians. Ann Intern Med 2018;168:359-60. [Crossref] [PubMed]
- Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117-24. [Crossref] [PubMed]
- Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3-10. [Crossref] [PubMed]
- Campbell NR, Lackland DT, Lisheng L, et al. The World Hypertension League: where now and where to in salt reduction. Cardiovasc Diagn Ther 2015;5:238. [PubMed]
- Elliot P, Brown I. Sodium Intakes Around the World: Background Document Prepared for the Forum and Technical Meeting on Reducing Salt Intake in Populations. Geneva: World Health Organization, 2006.
- Mohan S, Prabhakaran D. editors. Review of salt and health: situation in South-East Asia Region. Background paper for the expert meeting on population. Sodium reduction strategies for prevention and control of noncommunicable diseases in the South-East Asia Region. New Delhi: World Health Organization, Regional Office for South-East Asia, 2012.
- Wijewardene K, Mohideen M, Mendis S, et al. Prevalence of hypertension, diabetes and obesity: baseline findings of a population based survey in four provinces in Sri Lanka. Ceylon Med J 2005;50:62-70. [Crossref] [PubMed]
- Katulanda P, Ranasinghe P, Jayawardena R, et al. The prevalence, predictors and associations of hypertension in Sri Lanka: a cross-sectional population based national survey. Clin Exp Hypertens 2014;36:484-91. [Crossref] [PubMed]
- Duma N. Sri Lanka's sources of growth. International Monetary Fund, 2007.
- Dundar H, Millot B, Savchenko Y, et al. Building the skills for economic growth and competitiveness in Sri Lanka. Sri Lanka: The World Bank, 2014.
- McLaughlin JA, Jordan GB. Logic models: a tool for telling your programs performance story. Evaluation and Program Planning 1999;22:65-72. [Crossref]
- World Health Organization. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance, 2005.
- Jayawardena R, Swaminathan S, Byrne NM, et al. Development of a food frequency questionnaire for Sri Lankan adults. Nutr J 2012;11:63. [Crossref] [PubMed]
- Marmot M, Wilkinson R. Social determinants of health. Oxford: Oxford University Press, 2005.
- Rantala R, Bortz M, Armada F. Intersectoral action: local governments promoting health. Health Promot Int 2014;29:i92-i102. [Crossref] [PubMed]
- James SW, Friel S, Lawrence MA, et al. Inter-sectoral action to support healthy and environmentally sustainable food behaviours: a study of sectoral knowledge, governance and implementation opportunities. Sustainability Science 2018;13:465-77. [Crossref]
- Subar AF, Freedman LS, Tooze JA, et al. Addressing Current Criticism Regarding the Value of Self-Report Dietary Data. J Nutr 2015;145:2639-45. [Crossref] [PubMed]
- Lee H, Cho HJ, Bae E, et al. Not salt taste perception but self-reported salt eating habit predicts actual salt intake. J Korean Med Sci 2014;29 Suppl 2:S91-6. [Crossref] [PubMed]
- Murphy JK, Alpert BS, Stapleton FB, et al. Self-reports of salt intake by 10- to 18-year-olds: relationship to urinary sodium excretion. J Am Diet Assoc 1990;90:424-6. [PubMed]


