Late mortality after cardiac interventions over 10-year period in two Cameroonian government-owned hospitals
Introduction
Cardiovascular diseases (CVDs) remain the leading cause of death worldwide (1), with its burden disproportionately affecting Sub-Saharan Africa (SSA) region (1-3). Some of these CVDs require surgical management, but resources to provide optimal care are still very limited (4,5). To overcome these challenges, medical evacuations and humanitarian missions have been carried out over many years in several SSA countries (4-8). Early mortality after open heart surgery (OHS) in SSA has been estimated between 0% to 16% depending on the indication (5-9). However, the long-term mortality after cardiac surgery in this setting is not well known. Yangni-Angate et al. reported an overall mortality of 8.7% 5 years after valvular surgery. Survival at 25 years were 78% and 97% respectively for ventricular septum defect and atrial septum defect (7). Cardiac surgery started in Cameroon since 1985, and most public hospitals still rely on humanitarian missions (10-12). The short-term mortality rates were respectively 3.6% (10), 9% (11), and 7.4% (12). Data on the late mortality are scarce in our setting. The aim of this work was to study the long-term mortality rate of cardiac surgery in Cameroon.
Methods
This retrospective descriptive and analytical study was carried out in the cardio-surgery and intensive care unit of the Douala and Yaoundé General Hospitals between January 2007 and December 2017. The two hospitals are tertiary health facilities located in the economic (Douala) and political (Yaoundé) capitals of Cameroon. All patients who underwent cardiac surgery during humanitarian missions were included in this study. From January 2018 to April 2018, all patients or their relatives were contacted through phone for a free of charges medical examination. Incomplete medical files, patients and families lost to follow-up were excluded. Data collected included demographics, presenting symptoms, indication for surgery, operative procedure and late mortality (mortality occurred later than 30 days after surgical procedure). Data were analyzed using the software Epi-info version 7.1 (Centers for Disease Control and Preventive, Atlanta, Georgia, USA). We present qualitative data as frequencies and percentages. The 5- and 10-year survivals were computed using Kaplan-Meier survival analysis. This study was approved by the Institutional Research and Ethics Committee of the Douala University and all participants provided written informed consent. We carried out this study in accordance with the declarations of Helsinki.
Results
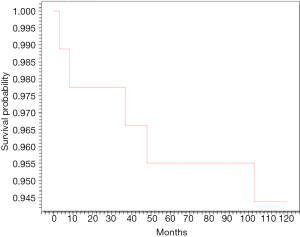
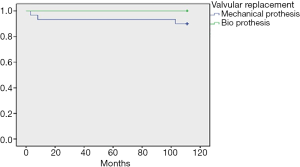
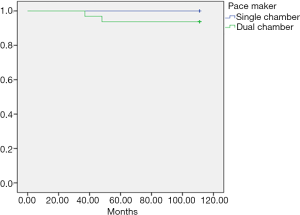
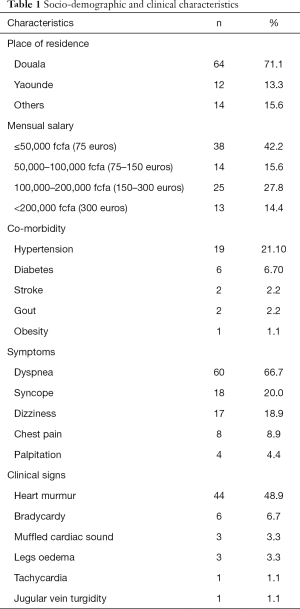
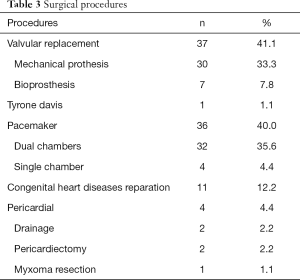
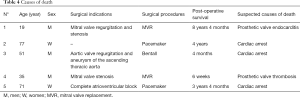
Demographics and clinical characteristics are shown in Table 1. Of a total of 98 patients operated during the study period, 8 (8.2%) were lost to follow-up. We finally included 90 patients (54.4% women; mean age 49±22 years). The majority of patients (71.1%) lived in Douala. Hypertension (21.1%) was the most frequent co-morbidity. Dyspnea was the most frequent presenting symptom (66.7%), and heart murmur (48.9%) the most frequent physical sign. The surgical indications are listed on Table 2. Valvular heart diseases were the most frequent condition (41.1%)—with isolated mitral in 59.4%, isolated aortic valve in 32.5%, and aorto-mitral involvement in 8.1%. The other indications were cardiac rhythm disorders in 36 (40.0%) patients, congenital heart diseases in 11 (12.2%) cases, chronic constrictive pericarditis in 4 (4.4%) cases, and intra cardiac tumor in 1 (1.1%) case. Surgical procedures are summarized in Table 3. Valve replacement was the most common type of surgery carried out in 37 (41.1%) cases-mostly with mechanical prosthesis. Among the latter, one patient benefited from a mitral valve replacement redo surgery 6 years after a reparation. Pacemaker—mostly dual-chambers were implanted in 36 (40.0%) patients. The median follow-up was 26 months. The causes of death are listed in Table 4. The overall late mortality rate was 5.7%, and the overall survival rates at 5 and 10 years were 95.5% and 94.4% respectively (Figure 1). The overall survival rates at 5 and 10 years for mechanical valve prosthesis were 93.3% and 90% respectively, whereas the survival rate at 10 years was 100% for patients with bioprosthesis (Figure 2). The Survival rates at 10 years were 94.1% and 100% respectively for dual and single chamber pacemaker (Figure 3).
Full table
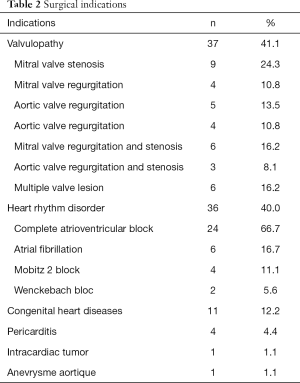
Full table
Full table
Full table
Discussion
The aim this work was to study the long-term mortality of patient operated in Cameroon during humanitarian missions. This is the first of its kind in our setting. It is important to emphasize at this point the role of “the Cameroonian association of patients who benefited from cardiac surgery” which is well organized, and helped us to contact many patients who were lost to follow-up.
Socio-demographics and clinical characteristics
Our data showed that patients who underwent cardiac surgery in Cameroon were young and predominantly female. Such figures have been reported by several authors. This can be explained by the presence of coronary heart disease (CHD) and valvular heart disease in our cohort (6-9). Valvular heart disease remains common among Cameroonians, mainly as a complication of rheumatic valvular heart disease (10-12). The patients presented late, when the valvular destruction is severe making any reparation quite impossible (7). As expected, valvular replacement was the most frequent surgical procedure. In a previous survey between 1985 and 1990, Kingue et al. reported a predominance of bioprosthesis implantation (10). The same policy was adopted in the earlier experience in Ivory Cost (7). These authors highlighted the difficulties associated with managing anticoagulants in SSA health settings (7,10). As this constraint is no longer the case in our setting, most patients benefited from mechanical valve implantation. Nevertheless, our findings stress the need of implementing primary and secondary preventive programmes of rheumatic heart disease (RHD), and improve early diagnosis in SSA (13,14). Not surprising, even if the population was young, the high rate of hypertension observed in our survey is in line with its growing burden faced by many SSA countries (1-3). Although pacemakers’ implantation has become a routine activity in three centers in Cameroon, some patients may benefit from cheaper operations during humanitarian mission (15). As previously reported by Tantchou Tchoumi et al. (16) in their survey from a private heart center located in North West Cameroon, complete atrioventricular block was the dominant indication, and dual-chamber the most implanted cardiac pacemaker in our series.
Causes of death
Since pathological autopsy is very rare in our setting and only reserved in forensic audit, the probable cause of death was determined by interviewing the caregivers, the family, and consulting the death certificate. This process called verbal autopsy has been developed in many countries to reduce the lack of reliable information on the causes of death (17). In two cases (patients 1 and 4), the death occurred in the hospital. Patient 1 died following a septic choc due to a prosthetic mitral valve endocarditis documented by echography and bacteriology analysis. In case n°4, the patient who was not compliant to anticoagulation after haven been discharged from hospital developed a mitral valve thrombosis documented by echography. Despite the initiation of thrombolytic, the patient died few hours after his admission. For the three remaining cases, death occurred at home, and the cause encoded as “cardiac arrest” could be hazardous. Family interview reported that death occurred during sleep in patient 2 and a sudden collapse in patients 3 and 5. Our small series emphasizes the need for reliable strategy to improve the recording of the causes of death.
Mortality trend
Post hospitalization mortality is not easy to establish in SSA. Geographical distribution and financial constraints, the lack of national or local level outcome metrics are often mentioned as possible reasons (18,19). As a consequence, outcomes data are often focused on short-term results making the present study useful (5-9). After a median follow-up period of 26 months, the overall mortality was 5.7%, which is consistent with other series in SSA even if they didn’t include cardiac pacing cases (7,20). The 5 years and 10 years survival rates were respectively 93.3% and 90% for mechanical valve, and 100% for bioprosthesis. Edwin et al. in Ghana mentioned a 98.1%, 97% and 94% actuarial survival respectively at 5, 10 and 15 years after mechanical valve replacement in children (20). Yangni-Angate et al. reported survival rates of 100%, 100% and 100% at 5, 10 and 15 years respectively for mechanical mitral valve replacement or repair versus 95%, 95%, and 85% for mitral valve replacement with bioprosthesis. For aortic valve replacement with bioprosthesis, survival at 5, 10, and 15 years were 85%, 82%, and 82% at 5, 10 and 15 years respectively versus 82%, 70% and 70% for mechanical prosthesis (7). In the last study, the rate of loss to follow up was up to 20% making our results acceptable. Furthermore, Mirabel et al. in Mozambique reported a mortality rate of 9.65% after a median follow-up of 23 months of 518 patients operated for miscellaneous indications (19). For cardiac pacing, after a median follow-up of 26 months, the pacemaker related death was 2%, and the pacemaker non-related death was 9.8% in a Nigeria experience (21). Mayosi et al. reported 17% of death after a median follow-up of 104 months in South Africa (22).
Limitations
The main limitation of this survey is its small sample size and its retrospective design, calling for large-scale prospective study on the same topic.
Conclusions
Long-term outcome of cardiac surgery in Cameroonian governmental hospitals are acceptable, with a low mortality rate. However, outcome metrics beyond mortality should be implemented for a prospective data collection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Institutional Research and Ethics Committee of the Douala University (ID: 1340CEI-UDo/03/2018/T) and all participants provided written informed consent. We carried out this study in accordance with the declarations of Helsinki.
References
- World Health Organization. Cardiovascular diseases (CVDs). WHO Fact sheet N° 317. Available online: http://www.who.int/mediacentre/factsheets/fs317/fr/
- Cappuccio FP, Miller MA. Cardiovascular disease and hypertension in sub-Saharan Africa: burden, risk and interventions. Intern Emerg Med 2016;11:299-305. [Crossref] [PubMed]
- Mensah GA, Roth GA, Sampson UK, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr 2015;26:S6-10. [Crossref] [PubMed]
- Edwin F, Tettey M, Aniteye E, et al. The development of cardiac surgery in West Africa--the case of Ghana. Pan Afr Med J 2011;9:15. [Crossref] [PubMed]
- Yankah C, Fynn-Thompson F, Antunes M, et al. Cardiac surgery capacity in sub-saharan Africa: quo vadis?. Thorac Cardiovasc Surg 2014;62:393-401. [Crossref] [PubMed]
- Swain JD, Sinnott C, Breakey S, et al. Ten-year clinical experience of humanitarian cardiothoracic surgery in Rwanda: Building a platform for ultimate sustainability in a resource-limited setting. J Thorac Cardiovasc Surg 2018;155:2541-50. [Crossref] [PubMed]
- Yangni-Angate KH, Meneas C, Diby F, et al. Cardiac surgery in Africa: a thirty-five year experience on open heart surgery in Cote d'Ivoire. Cardiovasc Diagn Ther 2016;6:S44-63. [Crossref] [PubMed]
- Salami MA, Akinyemi OA, Adegboye VO. Early results of open-heart surgery for acquired heart diseases in Ibadan, Nigeria. Nig J Cardiol 2018;15:14-9.
- Bori Bata AK, Ciss AG, Diop MS, et al. Mitral Valve Replacement in Senegal (West Africa): Indication and Short-Term Outcomes. Cardiology and Cardiovascular Research 2018;2:15-8. [Crossref]
- Kingue S, Ngodjoum N, Muna W, et al. The Cameroon experience of Cardiac surgery: a report of 83 cases operated between 1985 – 1990. Cardiol Trop 1994;20:5-11.
- Ngatchou W, Lemogoum D, Ménanga AP, et al. Cardiac surgery in Cameroon. Results at one year of the pilot phase. Rev Med Brux 2011;32:14-7. [PubMed]
- Kamdem F, Ngatchou W, Hamadou B, et al. Cardiac surgery in subSaharan Africa: a report of 3-year experience at the Douala General Hospital. J Xiangya Med 2017;2:67. [Crossref]
- Diarra MB, Ba HO, Sanogo KM, et al. The cost of evacuations for cardiovascular diseases and the needs for surgical and interventional treatment in Mali. Cardiol Trop 2006;32:66-8.
- Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 2007;357:470-6. [Crossref] [PubMed]
- Bonny A, Ngantcha M, Jeilan M, et al. Statistics on the use of cardiac electronic devices and interventional electrophysiological procedures in Africa from 2011 to 2016: report of the Pan African Society of Cardiology (PASCAR) Cardiac Arrhythmias and Pacing Task Forces. Europace 2018;20:1513-26. [Crossref] [PubMed]
- Tantchou Tchoumi JC. Permanent cardiac pacing activities in a tertiary sub-Saharan centre. J Xiangya Med 2017;2:62. [Crossref]
- Baiden F, Bawah A, Biai S, et al. Setting international standards for verbal autopsy. Bull World Health Organ 2007;85:570-1. [Crossref] [PubMed]
- Weiser TG, Gawande A. Chapter 16 Excess Surgical Mortality: Strategies for Improving Quality of Care. Debas HT, Donkor P, Gawande A, et al. editors. Essential Surgery: Disease Control Priorities, 3rd edition (Volume 1). Washington (DC): The International Bank for Reconstruction and Development/The World Bank, 2015 Apr 2.
- Mirabel M, Lachaud M, Offredo L, et al. Cardiac surgery in low-income settings: 10 years of experience from two countries. Arch Cardiovasc Dis 2017;110:82-90. [Crossref] [PubMed]
- Edwin F, Aniteye E, Tettey MM, et al. Outcome of left heart mechanical valve replacement in West African children--a 15-year retrospective study. J Cardiothorac Surg 2011;6:57. [Crossref] [PubMed]
- Falase B, Sanusi M, Johnson A, et al. Analysis of a five year experience of permanent pacemaker implantation at a Nigerian Teaching Hospital: need for a national database. Pan Afr Med J 2013;16:16. [Crossref] [PubMed]
- Mayosi BM, Little F, Millar RN. Long-term survival after permanent pacemaker implantation in young adults: 30 year experience. Pacing Clin Electrophysiol 1999;22:407-12. [Crossref] [PubMed]