Caseous calcification of the mitral annulus
Introduction
Caseous calcification is typically benign and most commonly involves the posterior mitral annulus. We present a case of an atypically located mitral annular calcification. The patient underwent clinical workup, echocardiography and computed tomography (CT). An isoechoic mass with peripheral hyper-attenuation identified in echocardiography was unspecific, supplementary cardiac CT could exclude potential differential diagnosis and avert cardiac surgery.
Case report
A 61-year-old asymptomatic woman was referred for echocardiography for the evaluation of recently detected systolic murmur on her physical examination. Transthoracic echocardiography (TTE, Figure 1A) revealed an oval 17 mm × 23 mm echodense obstructive mass in the left ventricular outflow tract (LVOT) of unclear origin. The mass demonstrated a peripheral echogenic rim, central hypoechoic foci and posterior acoustic shadow in the transesophageal echocardiography (TEE, Figure 1B).
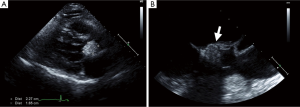
The left ventricular Doppler imaging study showed moderate diastolic dysfunction with increased filling pressure and (at least trivial) aortic and mitral regurgitation (Figure 1A). Because of the suspicion of the intracardiac calcified tumor and encroachment on the LVOT, surgical opinion was sought and surgical resection was recommended as a treatment approach.
Contrast-enhanced cardiac CT showed a well-defined lobulated mass with homogeneous attenuation adherent to the intervalvular fibrosa and the anterior mitral valve leaflet (Figure 2A). The attenuation was comparable to the blood pool but had curvilinear peripheral hyperattenuation along the margin of the mass suggestive of calcification. Differential diagnosis included calcified thrombus, tumor, pseudoaneurysm complicating infective endocarditis and vegetation.
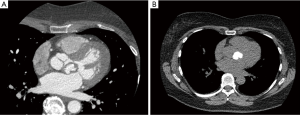
The non-enhanced scout view on CT revealed marked hyper-attenuation of the mass confirming diffuse calcification (Figure 2B). Based on the CT findings, a diagnosis of caseous calcification of the anterior mitral annulus was established and further diagnostic studies were not pursued.
Caseous calcification is typically benign, and most commonly involves the posterior portion of the mitral annulus with rare reports of involvement of the anterior mitral annulus noted in the literature. Our patient displayed an atypical location of the exuberant type of mitral annular calcification. Rarely, but when extensive, caseous calcification of the mitral annulus has been reported to result in mitral valve regurgitation and can rarely cause mitral stenosis (1-3). Although mitral annular calcification (MAC) has been reported to cause atrial fibrillation, conduction system disease and adverse cardiovascular events (4), no studies have been conducted to assess the implication of the caseous variant of MAC.
Given the CT findings and the absence of left ventricle dysfunction, surgery was deferred and conservative management was chosen. Our patient remains well without interval major adverse cardiac events (MACE) in over 18 months of follow up.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Alkadhi H, Leschka S, Prêtre R, et al. Caseous calcification of the mitral annulus. J Thorac Cardiovasc Surg 2005;129:1438-40. [PubMed]
- Pozsonyi Z, Tóth A, Vágó H, et al. Severe mitral regurgitation and heart failure due to caseous calcification of the mitral annulus. Cardiology 2011;118:79-82. [PubMed]
- Minardi G, Manzara C, Pulignano G, et al. Caseous calcification of the mitral annulus with mitral regurgitation and impairment of functional capacity: a case report. J Med Case Rep 2008;2:205. [PubMed]
- Fox CS, Vasan RS, Parise H, et al. Mitral annular calcification predicts cardiovascular morbidity and mortality: the Framingham Heart Study. Circulation 2003;107:1492-6. [PubMed]


