
Impact of non-invasive anatomical testing on optimal medical prescription in patients with suspected coronary artery disease
Introduction
Computed tomography (CT) systems were introduced in clinical care over 40 years ago. With technological advances such as multi-slice scanners in the early nineties, it was made possible to assess structures for which high temporal and spatial resolutions are necessary. With the introduction of 64-multidetector scanners, CT emerged as a non-invasive test for the assessment of the epicardial coronary arteries (1). In 2018, state-of-the art coronary CT is able to identify epicardial narrowing, quantify and characterize atherosclerotic plaque and evaluate the physiological component of coronary stenosis (2). The 2013 European Society of Cardiology (ESC) guidelines on the management of stable coronary artery disease (CAD), advocate coronary CT as a diagnostic alternative to stress imaging techniques or after non-conclusive exercise ECG in patients with a low to intermediate pre-test probability for stable CAD with a IIa recommendation level of evidence C (3). The 2016 National Institute for Health and Care Excellence (NICE) guidelines, recommended coronary CT angiography (CTA) as the first line non-invasive test for patients with suspected CAD due to its ability to accurately diagnose the presence of CAD and its cost-effectiveness compared to other non-invasive tests (4). Recently, the 2018 American Heart Association (AHA) Cholesterol guidelines recommend using CT derived calcium score in cases where there is an uncertainty in the decision to initiate statins (5).
The Scottish Computed Tomography of the HEART (SCOT-HEART) trial, provided further evidence of the clinical performance of coronary CTA in patients with suspected CAD (6,7). The 5-year follow of the SCOT HEART trial, which randomized 4,146 patients with stable chest pain to standard-of-care or coronary CTA showed that patients assigned to a coronary CTA diagnostic strategy had a reduction in the rate of death from coronary heart disease or nonfatal myocardial infarction compared to functional testing (2.3% CTA group vs. 3.9% in standard-of-care group). The SCOT-HEART investigators hypothesised that this difference was driven by the increased use of preventive medication (i.e., aspirin and statins) in patients evaluated with coronary CTA (8). We sought to investigate the impact of anatomical testing with luminal and plaque assessment on medical therapy prescription in consecutive patients undergoing clinical evaluation for suspected CAD in routine clinical practice, and to determine the agreement between physician on preventive therapy initiation.
Methods
Study design
Single-centre study including consecutive patients presenting with stable chest pain at a cardiology clinic who underwent functional non-invasive testing with cycloergometer and coronary CTA. For the present study, four clinical cardiologists reviewed each case based on clinical presentation, physical examination findings, electrocardiogram, lipid profile and risk assessment using the Framingham risk score. The assessment was complemented by a non-invasive test either exercise cycloergometer or coronary CTA. Physicians reviewed all cases using one non-invasive modality blinded to the alternative diagnostic strategy. Three weeks after the first assessment, the same group of physicians reviewed the cases using the alternative non-invasive test. Patient name and identification were blinded during case evaluation. Subsequently, the clinical cardiologists independently had to annotate in the electronic case report form (eCRF) a treatment management plan that included: request for an additional non-invasive test to clarify the diagnosis, referral to invasive coronary angiography, and the therapeutic management including the prescription of preventive medical treatment i.e., aspirin and/or statins. The indication for starting statins was based on individual baseline characteristics as recommended by the European Guidelines (3). Also, patients without statin recommendation but with abnormal non-invasive tests were candidates for statin prescription at the discretion of the cardiologist participating in the study. This study was approved by the Ethical Committee.
Non-invasive functional testing
All exercise tests were per protocol performed using the GE Ergometer Ebike Comfort, Ergoline, Germany. The test was continued until the development of limiting symptoms (angina, dyspnea, or fatigue), the appearance of heart rhythm or blood pressure abnormalities, the achievement of the maximal heart rate or marked ST-segment deviation (≥0.20 mV associated with typical angina). The executing cardiologist was blinded to the results of the coronary CTA.
Coronary CTA
The coronary CT scans were performed using a Siemens Somatom Definition flash 128 slices CT scanner (Forchheim, Germany) and contrast solution Iomeron 350 mg/mL Bracco imaging Deutschland GmbH (Konstanz, Germany). All patients with heart rate >65 bpm was given IV metoprolol titrated at a dose of 5 mg until a maximum dose of 15 mg or a heart rate <55 bpm. All patients received sublingual nitro-glycerine spray before image acquisition. Cardiologists assessed independently the presence and number of luminal narrowing, presence of plaque and composition (e.g., calcified and non-calcified) and extension of atherosclerotic disease in the epicardial coronary vessels according the SCCT vessel segments. Epicardial lesions with visual diameter stenosis >50% were considered obstructive (9).
Statistical analysis
Continuous variables are presented as mean and standard deviation and binary variables as percentages. Continuous variable with normal distribution were compared using the t-test and binary variables with Chi-square test. Cohen’s kappa was used to assess the agreement between cardiologist treatment decisions and Light’s kappa to calculate the average kappa across all rater pairs. The study was powered to detect 10% difference in the prescription of statins and/or aspirin between pairs assessed either using functional or anatomical assessment (6-8). To achieve a power of 80% and a two-sided significance of 5% for detecting a difference of 0.10 between marginal proportions, the study would require a sample of 87 patients. All analysis were performed with MedCalc version 18.10.
Results
From 12/06/2018 to 29/08/2018, 113 consecutive patients underwent non-invasive testing with exercise test and coronary CTA for suspected CAD and were included in this study. Twenty-six patients were excluded due to motion artefacts in a mayor coronary vessel on coronary CTA. The majority of the artefact were located in the right coronary artery. The mean radiation dose was 2.5±2.2 mSv. All CT images were performed using prospective acquisition protocol. Eighty-seven patients were evaluated by each cardiologist assessing exercise test and coronary CTA.
The mean age was 56.7±11.5. Forty-eight percent were females and 6% of patients suffered diabetes mellitus (Table 1). The mean Framingham score was 6.4±6.7%. Using coronary CTA, 21.4% exhibited an obstructive epicardial stenosis, and 22.1% was referred to invasive coronary angiography. In 54.2% any type of atherosclerotic plaque, obstructive or non-obstructive, was detected (Figure 1). Using functional testing, 9.1% were categorized as positive tests and 6.6% were referred for invasive cardiac catheterization. In 37.6% an additional test was requested to confirm the diagnoses (Figure 2). Overall, 11 patients were referred for invasive coronary angiography and 7 underwent revascularization.
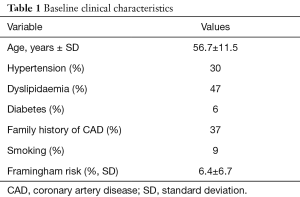
Full table
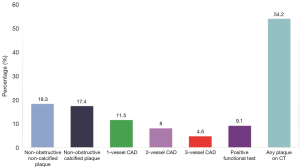
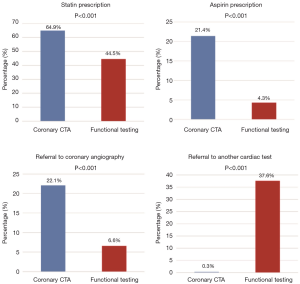
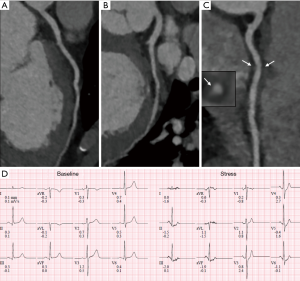
Use of coronary CTA as non-invasive test resulted in higher prescription of statin therapy (64.9% vs. 44.5%, P<0.001); higher prescription of aspirin (21.4% vs. 4.3%, P<0.001) and higher rate of referral for invasive coronary angiography (22.1% vs. 6.6%, P<0.001; Figure 2). Also, coronary CTA was associated with a reduced proportion of referral for additional non-invasive test (0.3% vs. 37.6%, P<0.001). A case example is shown in Figure 3.
The agreement between cardiologist for the assessment of the presence of atherosclerotic plaque was almost perfect reaching a mean Kappa coefficient of 0.81±0.03 whereas the agreement on the prescription of statins was substantial with a mean Kappa coefficient of 0.79±0.07.
At a median follow-up of 216 days (IQR 197 to 238), there were no deaths or myocardial infarctions. One patient had an acute coronary syndrome and underwent PCI.
Discussion
The main findings of the present study can be summarized as: (I) non-invasive testing with coronary CTA was associated with a higher prescription of statin and aspirin compared to functional testing; (II) use of coronary CTA resulted in higher referral for invasive coronary angiography; (III) atherosclerotic coronary plaques were observed in more than half of the patients; (IV) the agreement of physicians on the assessment of the presence of atherosclerotic plaques based on coronary CTA and prescription of optimal medical therapy was high.
Coronary CTA has been associated with an increase in the prescription of preventive medical therapy (10). The detection of atherosclerotic disease may trigger cardiologists to initiate or intensify medical therapy even in absence of luminal obstruction or ischemia. We found that in consecutive patients from routine clinical practice, use of coronary CTA was associated with an 45% increase in the prescription of statins and five times more prescription of aspirin compared to a functional non-invasive test strategy. Our findings are in line with the prospective, multicenter, randomized SCOT-HEART trial which investigated the utility of coronary CTA in the diagnosis and management of patients with suspected stable angina. In patients assigned to CTA, initiation of preventive measures was higher. At 5-year follow-up, 50.6% of the patients assigned to CTA were on antiplatelet therapy and 59.0% were on statin treatment whereas 40.5% and 50.3% of patients assigned to functional testing were on antiplatelet and statins, respectively. The clinical benefit of a CTA-guided diagnostic strategy was not observed in the PROMISE trial (11). It can be hypothesized that the reduction in myocardial infarction observed in SCOT-HEART might has been the result of a suboptimal stress testing comparator. In the SCOT-HEART trial, the rate of non-obstructive CAD was 38% and obstructive CAD was observed in 25% (8). In the present study, similar rates of disease prevalence were observed (35.7% non-obstructive and 24.1% obstructive) supporting the generalizability of these findings. Nonetheless, in comparison with SCOT-HEART, in the present study we found a higher prescription of statin and a lower prescription of antiplatelet therapy.
According to the 2018 AHA guidelines on hypercholesterolemia, statins are always indicated in the primary prevention in high risk patients (≥20% 10-year risk for atherosclerotic cardiovascular disease). In patients with an intermediate risk (7.5% to <20% 10-year risk for atherosclerotic cardiovascular disease), coronary calcium scoring should be considered to reclassify risk identification of patients who will potentially benefit from statin therapy (level of recommendation IIa). If the coronary calcium score is >1 it is reasonable to start statin therapy (5). Mitchell et al. (in year 2018) have shown that in patients with calcium score equal to zero, no benefit from statin treatment on clinical outcomes was observed in 9.4 years of follow-up. In contrast, a reduction in the cumulative rate of adverse events in patients treated with statins that had a calcium score >100 was found suggesting the potential of coronary CT to risk stratify and tailor statin therapy (12). Also, statin therapy has shown to improve plaque-risk profile by reducing adverse plaque components such as low-attenuation plaque volume, a surrogate of necrotic core and associated with unstable plaques prone to rupture (13,14).
The evidence of the benefit of aspirin in addition to a treatment with statins is less clear. Recently, the ASpirin in Reducing Events in the Elderly (ASPREE) trial showed that Aspirin use in healthy elderly persons did not prolong disability-free survival over a period of 5 years but led to a higher rate of major hemorrhage than placebo (15). Also, ASCEND trial (A Study of Cardiovascular Events iN Diabetes) showed that Aspirin prevented serious vascular events in persons who had diabetes and no cardiovascular disease, but it also caused an increase in major bleeding events (16). Use of aspirin for primary prevention should be personalized based on patients’ risk profile accounting for bleeding risk associated with chronic aspirin therapy. CTA-derived information such as disease localization, plaque composition and extent may also aid tailoring antiplatelet therapy. Nevertheless, further investigation is required.
In the present study, when patients were assessed using coronary CTA, they were 3.3 times more likely to be referred for an invasive procedure. The SCOT-HEART and PROMISE CTA trials, also showed an increased rate in referral for invasive coronary angiography (6,11). Visual assessment of epicardial stenosis using coronary CTA has been shown to overestimate disease severity compared to invasive coronary angiography, particularly in calcified lesions where the blooming artefact interferes with luminal analysis. In these cases, physicians have less certainty in the diagnosis and opt for an invasive investigation to clarify the diagnoses (17). The adjunction of a non-invasive physiological evaluation using fractional flow reserve derived from CT (FFRCT) has demonstrated to reduce the number of patients referred to the catheterization laboratory. Moreover, use of FFRCT also reduced the number of coronary angiographies showing no obstructive coronary disease increasing the positive predicted value of coronary CTA (18). Several studies have found that deferral of invasive procedures based on FFRCT is safe and despite the increased cost of the analysis the overall cost on a population basis is reduced (19,20). Clinical trials are ongoing and will better define the clinical benefit of an FFRCT diagnostic strategy on clinical outcomes.
Patients without CAD have an excellent prognosis. In contrast, the presence of non-obstructive CAD assessed by coronary CT is associated with higher rate of major adverse cardiovascular events. Andreini et al. stratified 1,196 consecutive patients with suspected CAD undergoing coronary CTA according to the presence of atherosclerotic plaque and degree of obstruction. Patients without CAD experienced no events during a 52-month follow-up. Of note, the presence of non-obstructive coronary disease was associated with a similar rate of events compared to patients with obstructive CAD (21). Further risk stratification assessing plaque characteristics and composition have identified the presence of positive remodeling, low-attenuation plaque, napkin-ring sign and spotty calcification as predictors of plaque rupture and acute coronary syndromes (22,23). The identification of non-obstructive plaques, or adverse plaque characteristics should prompt the treating physician to initiate or intensify medical therapy (24). Furthermore, in addition to qualitative plaque evaluation, quantitative plaque assessment has been shown to discriminate patients at risk and allowed to assess the impact of statins on plaque volume. Intensive statin treatment has been associated with changes in plaque composition (25,26). In the present study, clinical cardiologist evaluated the presence of non-obstructive plaques as part of the comprehensive CTA evaluation. We observed a high inter-observer agreement between cardiologists in the detection of non-obstructive plaques and initiation of medical therapy.
Limitations
The present study has several limitations. First, the data were acquired from routine clinical care; however, all cases were analyzed prospectively. Second, the study was designed to assess the differences in optimal medical therapy prescription thus no information concerning further testing or follow-up is available. Third, although participating physicians come from different university hospitals, all the cardiologist were trained in one European country which may have homogenized the medical management. Fourth, several sub-groups as diabetes patients are underrepresented in the present population; therefore, caution should be exercised when extrapolating these results to patients with a higher clinical profile. Fifth, the sample size of the population is relatively small and the single center nature of this study.
Conclusions
In this consecutive series of patients, epicardial atherosclerotic disease was found in half of the population. Assessment of patients with suspected CAD with coronary CTA resulted in an increase prescription of preventive therapies such as statins and aspirin compared to functional testing.
Acknowledgments
None.
Footnote
Conflicts of Interest: C Collet reports receiving research grants from Heartflow Inc., Biosensors and Abbott Vascular and consultancy fees from Philips. J Spapen has been supported by a research grant provided by the Cardiopath PhD Program. B De Bruyne declares that the Cardiovascular Center Aalst receives on his behalf grant support from Abbott, Boston Scientific, Biotronik, and St. Jude Medical and consulting fees from St. Jude Medical, Opsens, and Boston Scientific. He is a shareholder for Siemens, GE, Bayer, Philips, Heartflow, Edwards LifeSciences, Sanofi, and Omega Pharma. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics committee of 2019/010 No. B126201939544 and informed consent was taken from all the patients.
References
- Hurlock GS, Higashino H, Mochizuki T. History of cardiac computed tomography: single to 320-detector row multislice computed tomography. Int J Cardiovasc Imaging 2009;25 Suppl 1:31-42. [Crossref] [PubMed]
- Kolossvary M, Szilveszter B, Merkely B, et al. Plaque imaging with CT-a comprehensive review on coronary CT angiography based risk assessment. Cardiovasc Diagn Ther 2017;7:489-506. [Crossref] [PubMed]
- Task Force M, Montalescot G, Sechtem U, et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. European heart journal 2013;34:2949-3003. [Crossref] [PubMed]
- National Institute for Health and Clinical Excellence. Chest pain of recent onset: assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin (update). CG95. London: National Institute for Health and Clinical Excellence, 2016.
- Grundy SM, Stone NJ, Bailey AL, et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018.2018. [Epub ahead of print].
- SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 2015;385:2383-91. [Crossref] [PubMed]
- Williams MC, Hunter A, Shah ASV, et al. Use of Coronary Computed Tomographic Angiography to Guide Management of Patients With Coronary Disease. J Am Coll Cardiol 2016;67:1759-68. [Crossref] [PubMed]
- Newby DE, Adamson PD, Berry C, et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N Engl J Med 2018;379:924-33. [Crossref] [PubMed]
- Leipsic J, Abbara S, Achenbach S, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2014;8:342-58. [Crossref] [PubMed]
- Hulten E, Bittencourt MS, Singh A, et al. Coronary artery disease detected by coronary computed tomographic angiography is associated with intensification of preventive medical therapy and lower low-density lipoprotein cholesterol. Circ Cardiovasc Imaging 2014;7:629-38. [Crossref] [PubMed]
- Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 2015;372:1291-300. [Crossref] [PubMed]
- Mitchell JD, Fergestrom N, Gage BF, et al. Impact of Statins on Cardiovascular Outcomes Following Coronary Artery Calcium Scoring. J Am Coll Cardiol 2018;72:3233-42. [Crossref] [PubMed]
- Takata K, Imaizumi S, Zhang B, et al. Stabilization of high-risk plaques. Cardiovasc Diagn Ther 2016;6:304-21. [Crossref] [PubMed]
- Bittencourt MS, Cerci RJ. Statin effects on atherosclerotic plaques: regression or healing? BMC Med 2015;13:260. [Crossref] [PubMed]
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med 2018;379:1519-28. [Crossref] [PubMed]
- ASCEND Study Collaborative Group, Bowman L, Mafham M, et al. Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus.
- Andrew M, John H. The challenge of coronary calcium on coronary computed tomographic angiography (CCTA) scans: effect on interpretation and possible solutions. Int J Cardiovasc Imaging 2015;31 Suppl 2:145-57. [Crossref] [PubMed]
- Douglas PS, Pontone G, Hlatky MA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 2015;36:3359-67. [Crossref] [PubMed]
- Benton SM Jr, Tesche C, De Cecco CN, et al. Noninvasive Derivation of Fractional Flow Reserve From Coronary Computed Tomographic Angiography: A Review. J Thorac Imaging 2018;33:88-96. [PubMed]
- Hlatky MA, De Bruyne B, Pontone G, et al. Quality-of-Life and Economic Outcomes of Assessing Fractional Flow Reserve With Computed Tomography Angiography: PLATFORM. J Am Coll Cardiol 2015;66:2315-23. [Crossref] [PubMed]
- Andreini D, Pontone G, Mushtaq S, et al. A long-term prognostic value of coronary CT angiography in suspected coronary artery disease. JACC Cardiovasc Imaging 2012;5:690-701. [Crossref] [PubMed]
- Szilveszter B, Celeng C, Maurovich-Horvat P. Plaque assessment by coronary CT. Int J Cardiovasc Imaging 2016;32:161-72. [Crossref] [PubMed]
- Ferencik M, Mayrhofer T, Bittner DO, et al. Use of High-Risk Coronary Atherosclerotic Plaque Detection for Risk Stratification of Patients With Stable Chest Pain: A Secondary Analysis of the PROMISE Randomized Clinical Trial. JAMA Cardiol 2018;3:144-52. [Crossref] [PubMed]
- Cury RC, Abbara S, Achenbach S, et al. CAD-RADS: Coronary Artery Disease - Reporting and Data System: An Expert Consensus Document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Radiology (ACR) and the North American Society for Cardiovascular Imaging (NASCI). Endorsed by the American College of Cardiology. J Am Coll Radiol 2016;13:1458-66.e9. [Crossref] [PubMed]
- Stuijfzand WJ, Chow B, Lin F, et al. The role of plaque morphology in discriminating early versus late occurring acute coronary syndrome: the iconic trial. J Am Coll Cardiol 2018;71:A1630. [Crossref]
- Lee SE, Chang HJ, Sung JM, et al. Effects of Statins on Coronary Atherosclerotic Plaques: The PARADIGM Study. JACC Cardiovasc Imaging 2018;11:1475-84. [Crossref] [PubMed]


