Higher event rate in patients with known CAD despite a normal myocardial perfusion scan
Introduction
The myocardial perfusion imaging (MPI) using gated single photon emission computerized tomography (GSPECT) has been on the horizon of clinical cardiology of last four decades. The primary reasons for this popularity are its high diagnostic capability and ability to provide prognostic information useful in risk stratification and clinical decision making (1). There is a large body of data from various part of world indicating very high negative predictive value (NPV >99%) in patients with a normal SPECT MPI study (2,3). Gated MPI being a functional imaging modality is useful in ascertaining the hemodynamic significance of an anatomical lesion seen on coronary angiogram and allows risk stratification and guides about optimal management (4). Due to this very high NPV of a normal SPECT MPI, it has been considered as an efficient gatekeeper to catheterization laboratory (5). In recent years development in medical therapy and revascularization strategies have resultedin a growing number of patients with normal MPI who have a history of coronary artery diseases (CAD). Assessment of negative predictive of a normal MPI in this group of patients is important but currently data is limited with varied outcomes, depending upon duration of follow-up in different studies (4,6,7). This certainly creates ambiguities in decision making in this clinical scenario. The aim of this study was to find out negative predictive value of normal GMPI in patients with history of CAD.
Methods
Study design and patients’ demographic
The was a prospective study conducted at Nuclear Cardiology Department of Karachi Institute of Heart Diseases (KIHD), Karachi, Pakistan. Consecutive patients were accrued from December 2008 till December 2011 and followed till December 2013. The study was duly approved by the ethical committee of institute. We included 428 consecutivepatients with a history of CAD, which was defined as a healed myocardial infarct (MI) and/or previous coronary revascularization, who had a normal stress Tc-99m-MIBI (99mTechnetium Methoxy IsoBytyl Isonitrile) GSPECT MPI. Dynamic exercise on treadmill was used (using Bruce or modified Bruce protocol) in 255 (60%) patients while pharmacological stress using dipyridamole (0.142 mg/kg/min for 4 minutes) was adopted in 173 (40%). All patients were referred (272 inside and 156 outside referrals) for assessment of ischemia (179 patients asymptomatic; 249 patients with typical/atypical chest pain/dyspnea) Mean time interval between MPI and myocardial infarction (MI) was 3.2±4.6 years (118 patients) and revascularization was 1.9±3.2 years (310 patients). Patients with abnormal MPIs or MPI done within 60 days of coronary intervention or those with normal MPI but lost to follow-up were not included.
Stress protocol
Dynamic exercise (either Bruce or Modified Bruce protocol) was performed using treadmill and exercise was considered adequate when patient achieved 385% of age predicted target heart rate (220-age) or developed typical angina or dyspnea or >2 mm ST depressions in two or more leads. Beta blockers, calcium blocker and long acting nitrate were stopped 24-48 hours prior the test. Dipyridamole intervention was performed (0.567 mg/kg for 4 minutes) in patients who were unable to perform dynamic exercise or having left bundle branch block (LBBB) on resting ECG or specifically asked by the referring physicians due to limited exercise capacity. Tea, coffee and xanthine derivatives were stopped 24 prior in patients scheduled for dipyridamole test. A rise in 310 beats (from baseline) or drop of 310 mmHg of systolic blood pressure with or without symptoms or ST changes were considered as adequate response to dipyridamole. Tc-99m MIBI was given 1 minute before terminating exercise or 3-4 minutes after dipyridamole infusion.
Gated SPECT myocardial perfusion imaging
All patients underwent same day (rest-stress or stress-rest) myocardial perfusion GSPECT using Tc-99m MIBI. 10-15 mCi (370-555 MBq) of Tc-99m MIBI was administered intravenously for first study (rest in rest-stress or stress in stress-rest protocol) and 25-30 mCi (925-1,110 MBq) for second study (stress in rest-stress or rest in stress-rest protocol). Gated stress and non-gated rest SPECT acquisitions were performed using dedicated dual head cardiac (Cardio MD, Philips) gamma camera with low energy all purpose (LEAP) collimator, 32 projections around a 180-degree arc, a 64×64 matrix and 16 frames per cardiac cycle. Image reconstruction and LV functional parameters [EF, EDV, ESV and wall motion (WM)] were contemplated by using commercially available Astonish® and Autoquan® software packages respectively. An EF 350%, ESV ≤70 mL and WM score of zero (in a 17 segment model) were considered normal. Similarly, GMPI with SSS, SRS and SDS <2 were considered as normal. As per department protocol, to ensure optimal quality of scan, fatty meal with a glass of water prior the imaging was used to minimize sub-diaphragmatic activity and use of gated images (partial volume effect and wall motion) to rule out attenuation artifacts. No attenuation correction methodology was employed.
Follow-up
All patients/family were interviewed on telephone (median follow-up: 3.1 years; range: 2-5 years) regarding overall death, fatal or non-fatal MI. These events were confirmed by hospital records for those who were managed at our institute and by reviewing the discharge notes for those who were managed at other healthcare facilities. Cardiac death was defined as death caused by MI, significantcardiac arrhythmias, refractory congestive heart failure or unexplained sudden death.
Statistical analysis
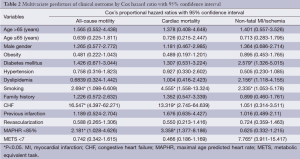
Comparisons between patient groups were performed using Student’s t-test for continuous variables and the χ2 test for categorical variables. Continuous variables were described by mean ± standard deviation (SD). Kaplan-Meier cumulative survival analysis for MACE like fatal and non-fatal MIs was performed, and survival curves were compared by the Logrank test. Univariate and multivariate Cox’s proportional hazard regression models were used to identify independent predictors of end points of interest. The risk of a variable was expressed as a hazard ratio with a corresponding 95% confidence interval. Statistical significance was defined as P<0.05. Commercially available packages Medcalc® and statistical package for social sciences (SPSS 17®) were used.
Results
The mean age of total 428 studied individuals was 56±10 years with a male to female ratio of 69%:31%. The average body mass index (BMI) of studied individuals was 26.660±5.172 Kg/m2 and 177 (41%) were found to be obese (BMI 330 Kg/m2). Prevalence of hypertension, diabetes, dyslipidemia and positive family history was 70%, 37%, 33% and 37% respectively. Smoking (defined as current or left less than 05 years) was found in 80 (19%) individuals. Dynamic exercise was performed by 255 (60%) of individual while dipyridamole stress was used in 173 (40%) who were unable to perform dynamic stress. The mean age predicted heart rate achieved and functional capacity (as metabolic equivalents, METS) were (86±12)% and 8.805±4.944 METS respectively. Mean left ventricular functional parameters like ejection fraction (%), end diastolic volume (EDV in mL) and end systolic volumes (ESV in mL) were (64±11)%, 87±33 and 33±24 mL respectively (Table 1).
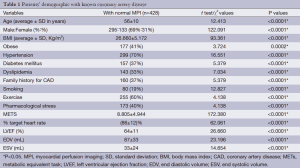
Full table
Follow-up analysis
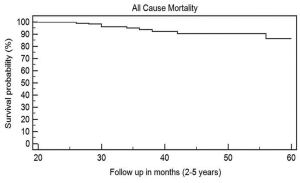
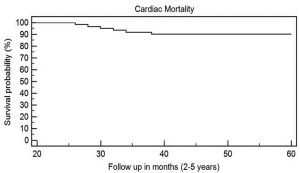
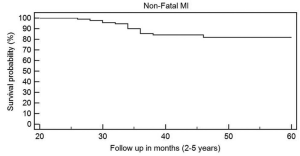
During a median follow-up of 3.1 years (range, 2-5 years), a total number of 60 patients (14%) died (all-cause mortality) with an annualized all-cause mortality rate of 2.8% (Figure 1). Cardiac deaths [fatal MI, congestive heart failure (CHF) or sudden unexplained death] was reported in 41 (10%) patients with annualized cardiac mortality rate was 2.0% (Figure 2). Nonfatal MI was reported in 77 patients (18%) with annualized event rate of 3.6% (Figure 3).
Predictors of long-term outcome
Smoking, CHF and failure to achieve 85% age predicted heart rate were found to be predictors for all-cause and cardiac mortality. Diabetes, dyslipidemia, smoking and limited functional capacity (<7 METS) were found to be predictors for non-fatal MI (Table 2).
Full table
Discussion
Over a long time as SPECT MPI has reached scientific and clinical maturity and we have grown to expect that the results of this test when negative, reliably predicts an excellent patients’ outcome. It is a well-established fact that annual probability of hard cardiac event with a normal exercise gated MPI is <1% (1-6). On the same note there has been an increase prevalence of normal MPI in patients with known CAD and this is primarily caused by remarkable improvement in medical therapy (statins mainly) and revascularization methodologies (8).The reasons for such clinical scenarios could be a patent graft or stent, presence of a haemodynamically non-significant stenosis, or a previous small (subendocardial) MI with a patent infarct-related coronary artery (4). In our study the all-cause mortality during the study period was 2.8% per year which is comparable with other published studies (4,6). However, the annual cardiac mortality and non-fatal MI rates in our study was 2% and 3.6% which are significantly higher than established ≈0.6% of average annual event rate in patients with a normal stress MPI (9). Our findings are in concordance with study by Acampa et al. (10) who studied 362 patients who had post-CABG normal MPIs with 22 month follow-up with a hard event rate (both fatal and non-fatal MIs) of 4%. Annualized cardiac and non-fatal MI rate in our study (2% and 3.6%) when compared with similar studies published by Schinkel (4) (0.5% and 1.4% in first 3 years follow-up) and Ottenhof et al. (7) (0.9% and 1.2% with 12 years follow-up) are significantly higher. Compared with these studies, our patients were younger, predominantly female with higher incidence of diabetes (37% vs. 10%) and hypertension (70% vs. about 50%). However, important to note that in Schinkels’ study (4) the annual cardiac mortality and cardiac mortality/non-fatal MI rate were increased to 1.3% and 3.1% during 4-6 years follow-up (0.5% and 1.4% in first 3-year follow-up) and closer to our findings with a median follow-up of 3.1 years. Another important aspect which draws our attention is the use of dipyridamole as mode of stress in 40% of our patients while previously mentioned studies included normal MPIs with dynamic exercise or with dobutamine stress. Recent reports have shown a higher event rate in patients having a normal GMPI with vasodilators (dipyridamole or adenosine) than dynamic exercise (11,12). Therefore, higher incidence of diabetes and hypertension and use of vasodilator stress in 40% of our patients are the major contributors for higher event rates in our study than other published data (4,6). Diabetes, dyslipidemia and smoking were independent risk factors for non-fatal MI while smoking, CHF and limited effort tolerance were risk factors for fatal MI. Pakistan is among the countries with highest incidence of diabetes with a reported figure of 13.14% (13). However, in our cohort, the incidence was 37% and this is due to referral bias. It is also an established fact that functional capacity of diabetics is lower as compared with non-diabetics (14) and this does explain the use of dipyridamole as stressor in 40% of participants of our study. Similarly the limited functional capacity in studied cohort who had dynamic exercise is a well-known risk factor for dismal outcome despite a normal MPI (15).
Findings of our study fuel the debate of safety profile of a normal MPI in patients with known CAD than in patients with suspected CAD where it is very high (cardiac event rate <1%). Higher event rates in this study puts a question mark over concept of warranty period in patients with known CAD and normal stress MPI (both exercise and vasodilator) as these patients had higher incidence of risk factors than patients cohorts reported in other studies (1,6). Based on multivariate analysis in this study, we suggest that patients with known CAD despite having a normal MPI need a close surveillance in the presence of risk factors like diabetes, dyslipidemia, history of smoking, limited effort tolerance and use of vasodilator as stressor. We strongly feel that in current era of effective medical and interventional strategies resulting in growing number of normal MPIs in patients with known CAD, more prospective studies are required to establish the safety profile of normal MPI in patients’ subset with known CAD and to design a cost effective but comprehensive surveillance strategy.
Our study has some limitations. (I) As coronary angiography was not routinely performed, odds of inclusion of false negative cases can be ruled out; (II) lack of data about how effectively diabetes and other risk factors were controlled as inadequate control of risk factors could be the reason for higher incidence during study period despite a normal MPI as noted in second half of follow-up in Schinkle’s study (4); (III) higher incidence of diabetes in studied population due to referral bias.
We conclude that patients with known CAD had higher cardiac event rates despite a normal stress SPECT MPI. Diabetes, dyslipidemia, smoking and limited functional capacity were the predictors for fatal and non-fatal cardiac events. A cost effective but comprehensive surveillance strategy is warranted.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Metz LD, Beattie M, Hom R, et al. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: a meta-analysis. J Am Coll Cardiol 2007;49:227-37. [PubMed]
- Shaw LJ, Hendel R, Borges-Neto S, et al. Prognostic value of normal exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: results from the multicenter registry of 4,728 patients. J Nucl Med 2003;44:134-9. [PubMed]
- Uz Zaman M, Fatima N, Samad A, et al. Overall and gender-based negative predictive value of a normal gated myocardial perfusion SPECT study: a single center experience. Ann Nucl Med 2011;25:207-11. [PubMed]
- Schinkel AF, Elhendy A, Bax JJ, et al. Prognostic implications of a normal stress technetium-99m-tetrofosmin myocardial perfusion study in patients with a healed myocardial infarct and/or previous coronary revascularization. Am J Cardiol 2006;97:1-6. [PubMed]
- Shaw LJ, Heller GV, Travin MI, et al. Cost analysis of diagnostic testing for coronary artery disease in women with stable chest pain. Economics of Noninvasive Diagnosis (END) Study Group. J Nucl Cardiol 1999;6:559-69. [PubMed]
- Hachamovitch R, Hayes S, Friedman JD, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40. [PubMed]
- Ottenhof MJ, Wai MC, Boiten HJ, et al. 12-Year outcome after normal myocardial perfusion SPECT in patients with known coronary artery disease. J Nucl Cardiol 2013;20:748-54. [PubMed]
- Lefkowitz RJ, Willerson JT. Prospects for cardiovascular research. JAMA 2001;285:581-7. [PubMed]
- Klocke FJ, Baird MG, Lorell BH, et al. American College of Cardiology; American Heart AssociationTask Force on Practice Guidelines; American Society forNuclear Cardiology. ACC/AHA/ASNC guidelines for the clinical useof cardiac radionuclide imaging—executive summary: a report of theAmerican College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2003;108:1404-18. [PubMed]
- Acampa W, Petretta M, Evangelista L, et al. Stress cardiac single-photon emission computed tomographic imaging late after coronary artery bypass surgery for risk stratification and estimation of time to cardiac events. J Thorac Cardiovasc Surg 2008;136:46-51. [PubMed]
- Fatima N, Uz Zaman M, Ishaq M, et al. Higher events rate in patients with a normal gated myocardial perfusion imaging with dipyridamole than exercise: “Run for reliability Indian J Nucl Med 2012;27:172-5. [PubMed]
- Navare SM, Mather JF, Shaw LJ, et al. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol 2004;11:551-61. [PubMed]
- Zafar J, Bhatti F, Akhtar N, et al. Prevalence and risk factors for diabetes mellitus in a selected urban population of a city in Punjab. J Pak Med Assoc 2011;61:40-7. [PubMed]
- Fang ZY, Sharman J, Prins JB, et al. Determinants of exercise capacity in patients with type 2 diabetes. Diabetes Care 2005;28:1643-8. [PubMed]
- Hachamovitch R, Hayes S, Friedman JD, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40. [PubMed]


