
Diagnostic efficacy of 2-shot compressed sensing cine sequence cardiovascular magnetic resonance imaging for left ventricular function
Introduction
It is vitally important to assess cardiac function in cardiac disease patients, as it is one of the strongest predictors of the prognosis of patients (1,2). It can guide decision making or the implantation of devices during treatment (3). Cardiovascular magnetic resonance (CMR) cine imaging can be used to assess the left ventricular (LV) volume, and it can be considered the noninvasive gold standard (4,5). The retrospective electrocardiogram (ECG)-gated, balanced steady-state free precession (bSSFP) cine sequence during breath-hold is a well-established sequence and is generally considered the standard sequence; in this sequence, segments of the entire k-space are collected for multiple cardiac cycles. However, as each slice requires multiple heartbeats, and only one or two slices can be scanned with one breath-hold. Hence, the whole CMR examination tends to take a long time. If a patient cannot tolerate multiple breath-holds or has arrhythmia, the images will have many artifacts, which lead to difficulties in the evaluation of LV function (6-9). The compressed sensing (CS) technique with sparse sampling can drastically reduce the acquisition time of CMR scans, and an iterative reconstruction algorithm can be used to prevent declines in image resolution (10,11). The CS approach can be integrated into single- or multi-shot sequences with different acceleration rates to record a complete cardiac cycle. Some studies have demonstrated the utility of single-shot (ss) CS cine CMR imaging for the evaluation of LV function (4). However, the image quality is inferior to that of standard cine CMR imaging. Because the ss CS cine sequence reduces the contrast between the myocardium and surrounding tissues due to the lower flip angle on the 3T scanner required to meet the SAR restriction, there are inaccuracies in delineating the epicardium and endocardium, which lead to some deviations (12). Multi-shot CS cine imaging reduces the acceleration rate or increases the spatial and/or temporal resolution compared to single-shot imaging. It can also increase the number of excitations, increase the image contrast and improve the image quality. In this study, we evaluated the use of a 2-shot CS cine technique in quickly acquiring high-quality images and accurately assessing cardiac function in clinical practice.
Methods
Study population
In this study, we continuously included patients from July 2018 to December 2018. Patients were scheduled for a CMR examination and had a variety of cardiac diseases. The exclusion criteria were patients who had a cardiac implantable electronic device, had claustrophobia, or failed to complete a CMR scan. This study was approved by the Ethics Committee of Peking Union Medical College Hospital (Ethical file code JS-1499).
The sample size was estimated based on the primary difference between the EF measurements. We assumed the common SD of the mean EF measure to be 0.15, the probability of type I error to be 0.05 (with both sides), and the probability of type II error to be 0.20. We calculated the necessary sample size for this research to be 36.
Cine magnetic resonance protocol
All the CMR examinations were performed with the clinical 3T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). All patients were subjected to the same scan procedure. After the localized images were taken, the cardiac axis views were planned, including three long axes (4-chamber, 3-chamber, 2-chamber) and a stack of eight to twelve short-axis slices covering the entire LV from the mitral valve to the apex. Then, three kinds of cine sequences were performed sequentially, and all of them included the three long-axis images and all the short-axis images that were mentioned above. The standard retrospectively gated segmented bSSFP cine sequence was first performed. The prototype ECG ss CS cine sequence with adaptive triggering and the prototype retrospectively gated 2-shot CS cine sequence were performed immediately after the standard cine sequence. Both ss CS cine and 2-shot CS cine sequence used the same iterative reconstruction algorithm. All the sequences were performed with breath-holding at end-expiration and covered the complete cardiac cycle. During the scanning, when it reached the SAR restriction, we chose to reduce the flip angle to reduce the SAR value. The details of all the sequence parameters are listed in Table 1.
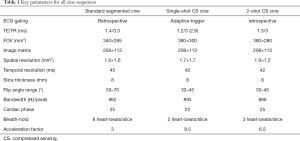
Full table
Qualitative image quality analysis
Two radiologists with 6 and 5 years of experience in CMR assessed all three types of cine sequences independently, focusing on the border of the myocardium and artifacts. The image quality was evaluated visually using a five-point scale: 0 = nondiagnostic quality, extensive artifacts affecting volumetric analysis, 1 = poor quality, moderate artifacts affecting volumetric analysis; 2 = adequate quality, mild artifacts affecting volumetric analysis; 3 = good quality, minimal or no artifacts affecting volumetric analysis; and 4 = excellent quality, no artifacts. The edge sharpness was evaluated by measured the maximum gradient of pixel intensities across the septal part in the middle segment of interventricular at the end of diastolic phase in 4 chamber view. The higher the gradient of the pixel intensities, the sharper of the edges were. The measure performed by one of the radiologists using ImageJ (National Institutes of Health, USA). Before the measurement, a scale bar was set to convert the pixel to the actual distance.
Quantitative analysis of the LV volume
For the quantitative measurement, all stacks of the short-axis slices of all cine CMR images were assessed using Medis Suite 3.1 (Medis Medical Imaging System, Leiden, The Netherlands). The epicardial and endocardial contours were traced manually and separately by the two radiologists. The endocardial trabeculations and papillary muscles of the left ventricle were included in the cavity volume of the LV. The most basal slice with at least 75% of the muscular ring at the end of systolic phase was considered the base, and the most apical slice that showed the LV cavity at the end of the diastolic phase was regarded as the apex. The LV volume and LV mass were calculated using the Simpson method in the software. The end of the systolic phase and end of the diastolic phase were detected manually based on the smallest and largest LV volumes over the entire cardiac cycle.
Statistical analysis
If the data showed a normal distribution, the data were expressed as the mean ± standard deviation (SD). If the data showed an abnormal distribution, the data were expressed as the median (first quartile, third quartile). The image quality was determined using the Wilcoxon matched-pairs signed-rank test. The edge sharpness was determined using paired t-test. The results of the LVEDV, left-ventricle end-systolic volume (LVESV), left-ventricle stroke volume (LVSV), LV mass, and left ventricular ejection fraction (LVEF) for each cine sequence were compared by the Wilcoxon matched-pairs signed-rank test. Linear regression and Bland–Altman analysis were used to evaluate the correlation and agreement between these LV measurements. The interobserver and intraobserver reliability were assessed using the intraclass coefficient correlation (ICC). A P value of less than 0.05 was considered statistically significant. All statistical analyses were performed by the commercially available software MedCalc Statistical Software, version 18.2.1 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2018).
Results
Thirty-eight patients successfully completed imaging scans with the three types of cine sequences. The detailed characteristics of the study population are summarized in Table 2. The mean heart rate was 74±14 bpm (range, 55–106 bpm) during the CMR scans. Among all patients, there were 2 patients encountered arrythmia and all of them were atrial fibrillation, while none of patients in this study encountered poor breath hold capacity.
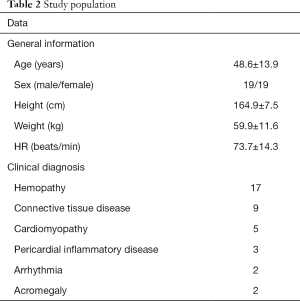
Full table
Examination time
The total examination time was 101±20 s (range, 67–146 s) for the standard cine sequence, 20±4 s (range, 14-29 s) for the ss CS cine sequence, and 30±6 s (range, 21–44 s) for the 2-shot CS cine sequence. The ss CS cine and 2-shot CS cine sequences had significantly shorter durations than did the standard cine sequence.
Image quality
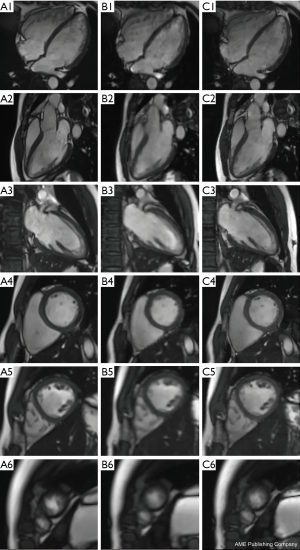
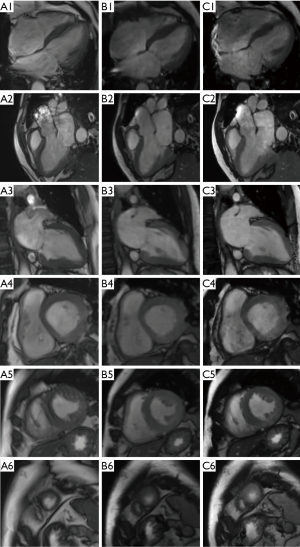
The standard cine sequence image score was 3.68±0.64, the ss CS cine sequence image score was 3.13±0.35, and the 2-shot cine sequence image score was 3.54±0.51. There was a significant difference in the image quality between the standard cine sequence and the ss CS cine sequence (Z=−2.858, P=0.004), while there was no significant difference between the standard cine sequence and the 2-shot CS cine sequence (Z=−0.832, P=0.405). There was good interobserver agreement in image quality for all types of cine sequence images. The kappa score was 0.871 for the standard cine sequence, 0.939 for the ss CS cine sequence, and 0.897 for the 2-shot CS cine sequence. The standard cine sequence edge sharpness was (2.47±0.18) mm, the ss CS cine sequence edge sharpness was (4.69±0.02) mm, and the 2-shot cine sequence edge sharpness was (2.51±0.13) mm. There was a significant difference in the edge sharpness between the standard cine sequence and the ss CS cine sequence (P<0.001), and between the standard cine sequence and the 2-shot CS cine sequence (P=0.037). Figures 1,2 show typical images for all the different types of the three cine sequences of a dilated cardiomyopathy patient with regular rhythm at diastole phase (Figure 1), and an atrial fibrillation patient at systolic phase (Figure 2).
LV function
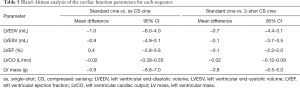
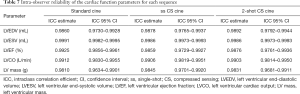
All 38 patients underwent quantitative analysis of the LV volume measurements. The standard cine images were used as the standard reference for the LV function measurement. Table 3 shows the cardiac function parameters for all three types of cardiac cine sequences. Table 4 show that according to the linear regression, there was good agreement between the standard cine and single-shot CS cine sequences and between the standard cine and 2-shot CS cine sequences, while for each LV volume measurement, the coefficient of determination (R2) between the standard cine and 2-shot CS cine sequences was better than the R2 between the standard cine and single-shot CS cine sequences. Table 5 and Figure 3 show the mean difference with the 95% confidence interval (CI) between the standard cine and the single-shot CS cine sequences and between the standard cine and 2-shot CS cine sequences according to the Bland-Altman analysis results. All the mean differences between the standard cine and 2-shot CS cine sequences are closer to zero than the mean differences between the standard cine and single-shot CS cine sequences. The interobserver and intraobserver reliability show very good agreement, as shown in Tables 6,7.
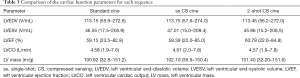
Full table

Full table
Full table


Full table
Full table
Discussion
Cardiac function is an important part of CMR examinations. The occurrence, development, treatment and prognosis of many diseases are closely related to cardiac function. CMR imaging can be used to quantify cardiac function noninvasively. Unlike other methods for which a mathematical model of the cardiac cavity is assumed, such as echocardiography, CMR imaging can accurately assess the entire cardiac cavity by direct calculations, so the results are more accurate, and CMR imaging can be considered the non-invasive gold standard.
The traditional bSSFP sequence is currently used to achieve sufficient image resolution in the evaluation of cardiac function; only one slice is scanned at one time. CS cine imaging can acquire images much faster and can even acquire one slice in a single heartbeat. Some previous studies have shown that CS cine and traditional imaging have similar image quality and LV measurements. Some research studies have shown that EDV, SV and LVEF were underestimated with CS cine imaging because prospective ECG triggering may miss the very first and the last phase of the cardiac cycle (13). We used adaptive ECG triggering and retrospective gating and therefore always acquired the full cardiac cycle to overcome this limitation. Other substantial image quality problems may occur because the spatial and temporal resolution is lower with CS imaging than with standard CMR imaging (14). In our study, the 2-shot CS cine prototype was designed to have better spatial resolution (1.6 mm × 1.6 mm) and temporal resolution (42 mm) than the standard CMR cine sequence. Although the single-shot CS cine sequence we used in this study has a similar spatial and temporal resolution as the standard cine sequence, the 2-shot CS cine prototype has good image quality and high agreement in the LV measurements with the standard cine sequence. It is reasonable that the edge sharpness of standard cine was superior to single-shot CS cine and 2-shot cine CS cine, but as for clinical use, the 2-shot CS cine images were able to get accurate measurements. These results indicate that the 2-shot CS cine prototype has better image quality and can obtain more accurate LV measurements than the single-shot CS cine sequence. Moreover, as it can shorten the total CMR examination time, the 2-shot CS cine prototype is more cost effective than the standard cine sequence during multiple breath-holds.
As we show in Table 1, for single-shot CS cine sequence, it scans one slice needs two heart-beats, and 2-shot CS cine needs three heart-beats. Single-shot CS acquired all k-space lines required for reconstructing an image in one readout train in a single heart-beat, while 2-shot CS were assembling k-space lines acquire from two heart-beats then reconstructing one image. The reason we got an extra one heart-beat is because for all CS sequence, we used the first heart-beat for steady state preparation, and the follow one or two heart-beats to acquire the data. That is why the name of the sequence is single-shot or 2-shot. For one slice, the 2-shot CS cine sequence increases the acquisition time by one heart-beat time compare with single-shot CS cine.
Moreover, the quality of retrospective standard cine images is often poor for patients with arrhythmia or a poor breath-hold capacity. Previous studies have shown that single-shot cine imaging can be inherently insensitive to arrhythmia or respiratory motions because of the single-shot acquisition technique (15). In this study, we found that the 2-shot CS cine prototype has a similar image score to the single-shot CS cine sequence, and those of both sequences were better than that of the standard cine sequence. Some of the CS cine sequences can be acquired during free breathing (16); in the future, a free-breathing CS cine sequence with better image quality should be investigated for patients with arrhythmia and a poor breath-hold capacity.
Limitations
There are some limitations to this study. Firstly, as for ss CS cine sequence, one of the major benefits is that it is insensitive to arrhythmia, theoretically 2-shot CS cine sequence may lose this benefit. In our study, we met 2 arrhythmia case, which were all atrial fibrillation. To our surprise, we did not meet very heavy artifacts, and did not affect the evaluation for cardiac parameters. But we think if the patient has some malignant arrhythmia, for 2-shot CS cine sequence will encounter heavy artifacts as the standard cine sequence, which need further study. Secondly, the sample size was relatively small, and all the participants included in the study were patients. However, because the sequence is mainly used in patients who cannot undergo the traditional examination process, the study results with patients are convincing. And lastly, he right-heart function was not evaluated, and we can compare this measure in future studies.
Conclusions
The 2-shot compressed sensing cine sequence can acquire images that are closer to the quality of the standard cine sequence, has a higher scanning speed, and has an acceptable level of accuracy in the functional parameter assessment compared with the single-shot cine sequence.
Acknowledgement
Funding: The work is supported by the National Natural Science Foundation of China (2018, Grant NO.81873891), the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (2018RC320004).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/cdt-20-135). The authors have no conflicts of interest to declare.
Ethical Statement: the authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of Peking Union Medical College Hospital (Ethical file code JS-1499). Written informed consent was obtained from the patient for publication of this study and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- White HD, Norris RM, Brown MA, et al. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation 1987;76:44-51. [Crossref] [PubMed]
- Curtis JP, Sokol SI, Yongfei W, et al. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J Am Coll Cardiol 2003;42:736-42. [Crossref] [PubMed]
- Knauth AL, Gauvreau K, Powell AJ, et al. Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of Fallot repair. Heart 2008;94:211-6. [Crossref] [PubMed]
- Rathi VK, Biederman RW. Imaging of ventricular function by cardiovascular magnetic resonance. Curr Cardiol Rep 2004;6:55-61. [Crossref] [PubMed]
- Moon JC, Lorenz CH, Francis JM, et al. Breath-hold FLASH and FISP cardiovascular MR imaging: left ventricular volume differences and reproducibility. Radiology 2002;223:789-97. [Crossref] [PubMed]
- Kozerke S, Plein S. Accelerated CMR using zonal, parallel and prior knowledge driven imaging methods. J Cardiovasc Magn Reson 2008;10:29. [Crossref] [PubMed]
- Jahnke C, Nagel E, Gebker R, et al. Four-dimensional single breathhold magnetic resonance imaging using kt-BLAST enables reliable assessment of left- and right-ventricular volumes and mass. J Magn Reson Imaging 2007;25:737-42. [Crossref] [PubMed]
- Eberle HC, Kai N, Jensen CJ, et al. Rapid MR assessment of left ventricular systolic function after acute myocardial infarction using single breath-hold cine imaging with the temporal parallel acquisition technique (TPAT) and 4D guide-point modelling analysis of left ventricular function. Eur Radiol 2010;20:73-80. [Crossref] [PubMed]
- Schwitter J, Oelhafen M, Wyss BM, et al. 2D-spatially-selective real-time magnetic resonance imaging for the assessment of microvascular function and its relation to the cardiovascular risk profile. J Cardiovasc Magn Reson 2006;8:759-69. [Crossref] [PubMed]
- Candes EJ, Wakin MB. An Introduction To Compressive Sampling. IEEE Signal Process Mag 2008;25:21-30. [Crossref]
- Lustig M, Donoho D, Pauly JM. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn Reson Med 2007;58:1182-95. [Crossref] [PubMed]
- Kido T, Kido T, Nakamura M, et al. Compressed sensing real-time cine cardiovascular magnetic resonance: accurate assessment of left ventricular function in a single-breath-hold. J Cardiovasc Magn Reson 2016;18:50. [Crossref] [PubMed]
- Vincenti G, Monney P, Chaptinel J, et al. Compressed sensing single–breath-hold CMR for fast quantification of LV function, volumes, and mass. JACC Cardiovasc Imaging 2014;7:882-92. [Crossref] [PubMed]
- Muthurangu V, Lurz P, Taylor A, et al. 1118 Real-time assessment of right and left ventricular volumes and function in patients with congenital heart disease using high spatio-temporal resolution radial k-t SENSE. Radiology 2008;248:782-91. [Crossref] [PubMed]
- Aandal G, Nadig V, Yeh V, et al. Evaluation of left ventricular ejection fraction using through-time radial GRAPPA. J Cardiovasc Magn Reson 2014;16:79. [Crossref] [PubMed]
- Goebel J, Nensa F, Bomas B, et al. Real-time SPARSE-SENSE cardiac cine MR imaging: optimization of image reconstruction and sequence validation. Eur Radiol 2016;26:4482-9. [Crossref] [PubMed]


