
Revascularization versus drug therapy for coronary artery disease in patients aged over 80 years: a real-world study
Introduction
Coronary artery disease (CAD) is one of the most common chronic diseases in the elderly (1). Percutaneous coronary intervention (PCI), coronary artery bypass grafting (CABG), and drug therapy are the mainstay treatment for CAD.
It has been shown that, in comparison with younger patients aged less than 65 years, older CAD patients were more likely to have myocardial infarction, severe arrhythmia, cardiogenic or non-cardiogenic complications, decreased ejection fraction, and high levels of fasting blood glucose, serum creatinine, and low density lipoprotein (LDL) (2). Elderly patients often have multiple coronary lesions, left main stem lesions, and complete occlusion. Revascularization in elderly CAD patients is associated with increased risks of Q-wave myocardial infarction, vascular complications, and mortality in comparison with younger patients (3,4). Therefore, elderly patients with CAD is often managed conservatively due to the existence of comorbidities and concerns of surgical risks (4).
Recent advancements in PCI and CABG have improved safety and provided elderly patients with more options of coronary revascularization (5). These advancements involve the use of new stents, new drugs, safer dosing regimens, and procedure optimization (6). Early results of the TIME (Trial of Invasive versus Medical therapy in Elderly patients with chronic symptomatic coronary artery disease) study found that revascularization treatment in elderly patients with CAD is associated with high risks and lack significant benefit (7). However, the TIME study suggested PCI treatment in these patients (7). Previous studies have shown a lower mortality rate in CAD patients aged over 75 years treated with revascularization in comparison with those treated with drug therapy (8,9). However, it is not clear whether Chinese CAD patients aged over 80 years can benefit from revascularization treatment such as PCI and CABG.
Our study aimed to evaluate the efficacy and safety of revascularization versus drug therapy in the oldest-old Chinese patients with CAD.
Methods
Patients
From January 2011 to January 2016, 501 CAD patients aged ≥80 years were recruited at the Anzhen Hospital (Beijing, China). The diagnosis of CAD was based on stenosis ≥50% of at least one major coronary artery, such as the left main stem, left anterior descending coronary artery, left circumflex branch, right coronary artery or its main large branch.
The inclusion criteria were: (I) age ≥80 years; (II) were diagnosed with CAD; (III) coronary angiography showed stenosis ≥50% of at least one major coronary artery; (IV) with complete medical records. Patients with the following conditions were excluded: (I) younger than 80 years; (II) previous CABG surgery (III) comorbidities that require cardiac surgery; (IV) severe infection; (V) malignant tumors; (VI) platelet count <100×109/L at admission; (VII) hemoglobin <120 g/L for male or <110 g/L for female at admission; (VIII) contraindications for antiplatelet therapy; (IX) failure of switch from PCI to CABG or drug therapy.
This study was approved by the Institutional Review Board of Ethics Committee of Beijing Anzhen Hospital, Capital Medical University, China. All participants gave written informed consent. Our study was conducted in accordance with the Helsinki II declaration.
Treatment
Our patients were managed with three different treatments: PCI (n=283), CABG (n=106), and drug therapy (n=112).
For the PCI procedure, the radial artery or femoral artery pathway was selected based on patient’s condition. The coronary artery lesion was pre-expanded with a balloon. A drug-eluting stent was placed if needed. A TIMI 3 flow after surgery was required. Oral aspirin, statins, and clopidogrel were administered postoperatively for at least 1 year.
Cardioplegia CABG or non-stop CABG was performed with or without cardiopulmonary bypass support. Five days before the surgery, low-molecular-weight heparin was subcutaneously injected instead of aspirin and clopidogrel. Oral aspirin, statins, and clopidogrel were administered postoperatively for at least 1 year.
Oral administration of aspirin and statins was used for the drug therapy.
Follow-up
Patients were followed by telephone call. All-cause death, cardiovascular-related death, and cardiovascular-related readmission (including angina, acute myocardial infarction, and heart failure) were recorded.
Outcome evaluation
The primary outcome was cardiovascular-related mortality during the follow-up period. The secondary outcomes included all-cause mortality, readmission related to cardiovascular events (angina, acute myocardial infarction, heart failure) or hemorrhagic events, and post-discharge Seattle Angina Questionnaire (SAQ) score. The SAQ scale evaluates the functional status and quality of life of patients with CAD (10). Each domain of the scale has a highest score of 100, and a higher score represents a better quality of life.
Covariates
Gender, age, body mass index, glycosylated hemoglobin level, low density lipoprotein-cholesterol (LDL-C) level, high density lipoprotein-cholesterol (HDL-C) level, smoking, hypertension (11), diabetes (12), old cerebral infarction, old myocardial infarction, and previous PCI at administration were included as the covariates. Ejection fraction during hospitalization, left ventricular end diastolic diameter, and coronary angiography were also collected.
Statistical analysis
Normally distributed continuous variables were compared using the one-way analysis of variance. Non-normally distributed continuous variables were compared using the Kruskal-Wallis test. The Student-Newman-Keuls (SNK) method was used to perform post hoc multiple comparisons when there was significant difference. Categorical variables were compared using the Chi-square test or the Fisher exact test. To compare the 1-, 2-, and 3-year mortality, the unconditional logistic regression model was used with adjustment of gender, age, lesion count, stem lesion, CAD type, and previous cerebral infarction. All statistical analyses were performed using the SAS version 9.3 (SAS Institute, Cary, NC). A two-tailed P value <0.05 was considered statistically significant.
Results
General information
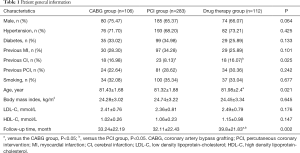
A total of 501 patients (age range, 80–92 years) were included in our study. Ten patients died in hospital, and 90 patients were lost to follow-up after discharge. The follow-up rate was 82.0%. The median follow-up time was 25 months (interquartile range, 17.0–55.5 months). Patients who were lost to follow-up consisted of 50 patients (17.7%) in the PCI group, 21 patients (19.8%) in the CABG group, and 19 patients (17.0%) in the drug therapy group, which showed no significant difference (P=0.872). The three groups also showed no significant difference in age, gender, smoking, body mass index, LDL-C, HDL-C, hypertension, diabetes, previous myocardial infarction, previous cerebral infarction, and previous PCI (Table 1).
Full table
CAD pathology
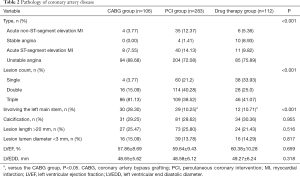
The types of CAD differed significantly between the three groups (Table 2). There was 88.68% of unstable angina in the CABG group, which was significantly higher than that in the PCI group (72.08%) and the drug therapy group (75.89%). Acute ST-segment elevation myocardial infarction and acute non-ST-segment elevation myocardial infarction accounted for 14.13% and 12.37% in the PCI group, respectively, which were significantly higher than the CABG group (7.55%, 3.77%) and the drug therapy group (9.82%, 5.36%). The drug therapy group had a significantly higher proportion of stable angina (8.93%). than the PCI group (1.4%).
Full table
Angiography showed a significantly higher proportion of the left main stem lesion in the CABG group (28.30%) in comparison with the PCI group (10.25%) and the drug therapy group (10.71%). There was no significant difference in lesion calcification, long lesion (>20 mm), small vessel disease (lumen <3 mm), left ventricular ejection fraction, and left ventricular end diastolic diameter between the three groups (Table 2).
Outcomes
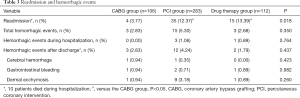
There was no significant difference in bleeding and mortality between the three groups during hospitalization (Table 3). The readmission rate for cardiovascular events in the CABG group was significantly lower than the PCI and drug therapy groups (P=0.018) (Table 3).
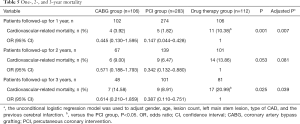
Full table
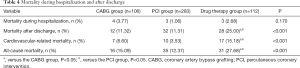
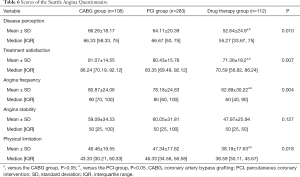
All-cause mortality and cardiovascular-related mortality in the drug therapy group were significantly higher than the PCI and CABG groups (P<0.05, Table 4). With respect to cardiovascular-related 1-year mortality, the odds ratio (OR) was 0.147 (0.044–0.428) for the PCI group, 0.445 (0.130–1.595) for the CABG group with the drug therapy group as the reference (Table 5). Similar results were observed for cardiovascular-related 2- and 3-year mortality. Scores of physical limitation, angina frequency, treatment satisfaction, and disease perception of the SAQ scale in the PCI and CABG groups were significantly higher than the drug therapy group (all P<0.05, Table 6). The scores of angina stability did not differ significantly between the three groups (P=0.127).
Full table
Full table
Full table
Discussion
Our study for the first time evaluated the efficacy of revascularization treatments versus drug therapy in Chinese oldest-old patients with CAD. We found that patients treated with PCI or CABG had significantly lower all-cause mortality and cardiovascular-related mortality and significantly higher scores in four domains of the SAQ scale in comparison with those treated with drug therapy. Readmission rate for cardiovascular events in the CABG group was significantly lower than that the PCI and drug therapy groups.
Our study found that patients treated with revascularization had significantly lower mortality than those treated with drug therapy group. However, there was no significant difference in mortality between the PCI and CABG groups. Our finding is consistent with a previous study based on a Canadian cohort (13). Oldest-old patients are more likely to have severe coronary artery lesions, leading to increased complexity of surgery and more vascular complications (14). Patients with ischemic cardiomyopathy and impaired heart function may benefit from revascularization, which can effectively improve heart function, quality of life, and survival time. The insignificant difference in all-cause mortality and cardiovascular-related mortality between the PCI and CABG groups should be interpreted considering the relatively higher proportions of left main stem lesion and multiple coronary artery lesions in the CABG group. This is consistent with guidelines that recommend CABG for the treatment of multiple lesions or left main stem lesions. Despite the relatively high complication risks of CABG, this procedure is more effective than PCI in treating more serious coronary artery lesions.
It has been shown that dual antiplatelet therapy after revascularization is safe and effective in the oldest-old patients (15). Consistently, our study found that dual antiplatelet therapy in the PCI and CABG groups was not associated with increased risks of cerebral hemorrhage, gastrointestinal bleeding, and skin ecchymosis in comparison with the drug therapy group. A study based on registry database suggested that the risks of PCI in the oldest-old patients with CAD have decreased with the emergence of radial artery intervention, drugs such as bivalirudin, and second-generation drug-eluting stents (16). Safety and efficacy of statins in the oldest-older patients have been confirmed (17), but their impact on prognosis is still not convincing (18). Currently, drug therapy is the mainstay for the treatment of oldest-old patients with CAD in China (19). With advancement in the safety and efficacy of revascularization in the oldest-old patients, prognosis of patients with CAD is expected to be further improved.
Our study demonstrated that patients in the PCI and CABG groups had significantly higher scores in physical limitation, angina frequency, treatment satisfaction, and disease perception of the SAQ scale than those in the drug therapy group. Our findings indicate that patients treated with revascularization may have better quality of life in comparison with those treated with drug therapy alone. The SAQ scale is a valid assessment for prognosis in patients with CAD (10). However, our study found no significant difference in angina stability between the three groups. Based on the evidence from clinical trials, a strategy of routine revascularization (with PCI or CABG surgery as appropriate) plus guideline-directed medical therapy reduces rates of death or myocardial infarction, and improves quality of life compared to an initial approach of guideline-directed medical therapy alone in patients (20,21). In contrast, in our study, drug therapy did not provide better clinical outcomes, which may be related to the fact that our study subjects were over 80 years old patients whose susceptibility to medication may have been reduced by long-term medication.
Our study has some limitations. First, the pathological types of CAD and coronary artery lesions differed significantly between the three groups, which may cause heterogeneity and confounding factors. Second, we were unable to conduct a detailed quantitative analysis on coronary artery lesions in all patients due to incomplete information. Third, the drug regimen was limited to aspirin and statins. These limitations may lead to errors in research results.
Conclusions
Revasculation treatments such as PCI and CABG are associated with improved survival time and quality of life in the oldest-old patients with CAD in comparison with drug therapy. Revascularization treatment shows generally good safety and efficacy in the oldest-old patients. We recommend CABG as the option of revascularization for the treatment of left main stem lesions in oldest-old patients.
Acknowledgments
Funding: This study was supported by the Beijing Lab for Cardiovascular Precision Medicine, Beijing, China (No. PXM2017_014226_000037).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/cdt-20-185). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of Ethics Committee of Beijing Anzhen Hospital, Capital Medical University, China. All participants gave written informed consent. Our study was conducted in accordance with the Helsinki II declaration.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See:
References
- Natarajan A, Samadian S, Clark S. Coronary artery bypass surgery in elderly people. Postgrad Med J 2007;83:154-8. [Crossref] [PubMed]
- Pfisterer M, Buser P, Osswald S, et al. Outcome of elderly patients with chronic symptomatic coronary artery disease with an invasive vs optimized medical treatment strategy: one-year results of the randomized TIME trial. JAMA 2003;289:1117-23. [Crossref] [PubMed]
- Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation 2007;115:2570-89. [Crossref] [PubMed]
- TIME Investigators. Trial of invasive versus medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomised trial. Lancet 2001;358:951-7. [Crossref] [PubMed]
- García-Palmieri MR. Evidence based secondary prevention of coronary artery disease in the elderly--2006. P R Health Sci J 2006;25:229-39. [PubMed]
- Wong CK, Newby LK, Bhapker MV, et al. Use of evidence-based medicine for acute coronary syndromes in the elderly and very elderly: insights from the Sibrafiban vs aspirin to Yield Maximum Protection from ischemic Heart events postacute cOroNary sYndromes trials. Am Heart J 2007;154:313-21. [Crossref] [PubMed]
- Wang TY, Gutierrez A, Peterson ED. Percutaneous coronary intervention in the elderly. Nat Rev Cardiol 2011;8:79-90. [Crossref] [PubMed]
- Batchelor WB, Anstrom KJ, Muhlbaier LH, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7,472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol 2000;36:723-30. [Crossref] [PubMed]
- Miranda Malpica E, Peña Duque MA, Castellanos J, et al. Predictors of mortality and adverse outcome in elderly high-risk patients undergoing percutaneous coronary intervention. Arch Cardiol Mex 2007;77:194-9. [PubMed]
- Patel KK, Arnold SV, Chan PS, et al. Validation of the Seattle angina questionnaire in women with ischemic heart disease. Am Heart J 2018;201:117-23. [Crossref] [PubMed]
- Alexander KP, Anstrom KJ, Muhlbaier LH, et al. Outcomes of cardiac surgery in patients > or = 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol 2000;35:731-8. [Crossref] [PubMed]
- Likosky DS, Dacey LJ, Baribeau YR, et al. Long-term survival of the very elderly undergoing coronary artery bypass grafting. Ann Thorac Surg 2008;85:1233-7. [Crossref] [PubMed]
- Graham MM, Ghali WA, Faris PD, et al. Survival after coronary revascularization in the elderly. Circulation 2002;105:2378-84. [Crossref] [PubMed]
- Legrand VM, Serruys PW, Unger F, et al. Three-year outcome after coronary stenting versus bypass surgery for the treatment of multivessel disease. Circulation 2004;109:1114-20. [Crossref] [PubMed]
- Hoffman SN, TenBrook JA, Wolf MP, et al. A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: one- to eight-year outcomes. J Am Coll Cardiol 2003;41:1293-304. [Crossref] [PubMed]
- Bromage DI, Jones DA, Rathod KS, et al. Outcome of 1051 Octogenarian Patients With ST-Segment Elevation Myocardial Infarction Treated With Primary Percutaneous Coronary Intervention: Observational Cohort From the London Heart Attack Group. J Am Heart Assoc 2016;5:e003027. [Crossref] [PubMed]
- Sang CW, Xie J, Sun YY. Study on efficacy and safety of atorvastatin in treatment of elder patients with hypertension and hyperlipidemia. Journal of Clinical and Experimental Medicine 2012;11:264-5.
- Rothschild DP, Novak E, Rich MW. Effect of Statin Therapy on Mortality in Older Adults Hospitalized with Coronary Artery Disease: A Propensity-Adjusted Analysis. J Am Geriatr Soc 2016;64:1475-9. [Crossref] [PubMed]
- Liu HW, Fan J, Wang L, et al. Current situation on therapeutic methods of coronary heart disease in the elderly Chin J Health Care Med 2014;16:83-6. (in Chinese).
- Phillips LM, Hachamovitch R, Berman DS, et al. Lessons learned from MPI and physiologic testing in randomized trials of stable ischemic heart disease: COURAGE, BARI 2D, FAME, and ISCHEMIA. J Nucl Cardiol 2013;20:969-75. [Crossref] [PubMed]
- Stone GW, Hochman JS, Williams DO, et al. Medical Therapy With Versus Without Revascularization in Stable Patients With Moderate and Severe Ischemia: The Case for Community Equipoise. J Am Coll Cardiol 2016;67:81-99. [Crossref] [PubMed]


