Approach to hypertension among primary care physicians in the West Region of Cameroon: substantial room for improvement
Introduction
Hypertension is the leading cause of cardiovascular disease (CVD) and deaths globally (1). It is associated with at least 7.6 million deaths per year worldwide (13.5% of all deaths). Eighty percent of global CVD mortality occurs in low- and middle-income countries (LMIC) (1-3). The importance of blood pressure (BP) as a modifiable risk factor for CVD is well-recognized and many effective and inexpensive BP—lowering treatments are available. There is considerable evidence that long-term BP lowering to what is considered either normal or optimal levels reduces the likelihood of CVD and results in several other important health benefits (4).
The common rule of halves in hypertension epidemiology suggests that about half of hypertensive populations are diagnosed, half of those diagnosed are treated, and half of those treated are controlled; these estimates may be optimistic in many LMIC. Indeed, poor BP control has been found in these countries (5-7). In Cameroon for instance, a survey conducted in 2011 found a hypertension prevalence of 47.5%, with only 31.7% of all individuals with hypertension who were aware of their status. Moreover, 59.9% of those aware (19% of all those with hypertension) were on treatment, among whom only 24.6% (4.7% of all those with hypertension) achieved expected target BP levels (8). Other studies have confirmed this high prevalence of hypertension and poor BP control in Cameroon as well as in other African countries (9-11), with consequentially complications of hypertension, especially stroke and heart failure, which are becoming rapidly more frequent in the region (10-13).
Physicians’ inability to provide good management of hypertension has been identified as an important contributor to poor BP control in hypertensive patients (14-17). In Cameroon where most of hypertensive patients remain uncontrolled, no previous study has investigated primary care doctors’ state of knowledge and practice patterns on the management of hypertension. This study was carried out to assess the approach of primary care physicians (PCPs) to the detection, evaluation and treatment of hypertension in Cameroon. It is believed that data will contribute to strategies to improve BP control among hypertensive patients in Cameroon.
Methods
Ethics statement
The study was approved by the Regional Office of the Ministry of Public Health (MOH) for the West region, acting as Ethics Committee. All participants interviewed in the study provided a written informed consent.
Study population and setting
We carried out this survey in February 2012 in the West region of Cameroon which had in 2010 a population of 1,785,285 inhabitants (18).The region is divided into 20 health districts, and has a total of 530 health facilities, both public and private, but none is a teaching hospital. There were 111 PCPs (general practitioners) working in the region at the time of the survey. Among these 111 PCPs, we included those who were present at their work place during working hours when the investigator visited, and who consented to participate in the study.
Data collection
Data were collected by a trained investigator using a structured pretested questionnaire administered during interviews of about 10 minutes. The questionnaire was developed based on previous studies (16,19), and assessed: (I) background characteristics such as sex, age, number of years of practice, location of practice, daily patients’ load; (II) detection of hypertension including number of BP readings, threshold levels of BP; (III) evaluation of patients with high BP especially with paraclinical tests to determine co-morbidities, target organ damages and cardiovascular diseases; (IV) treatment of hypertension including patient education, advise on non-pharmacological measures to control BP, choice of antihypertensive drugs and the therapeutic target of BP; (V) source of information on hypertension care and willingness to receive additional training on hypertension.
Participants’ approach to hypertension was evaluated in accordance with the recommendations of the Seventh report of the Joint National Committee (JNC 7) on prevention, detection, evaluation, and treatment of high BP (20).
Data analysis
Data were coded, entered and analyzed using the Statistical Package for Social Science (SPSS) version 20.0 for Windows (SPSS, Chicago, Illinois, USA). We described continuous variables using means with standard deviations (SD), and categorical variables using their frequencies and percentages. We divided our study population in recent graduates (≤10 years since graduation) and older graduates (>10 years since graduation) and made comparison between them. The Chi-square test or its equivalents were used to compare qualitative variables and a P value less than 0.05 was considered statistically significant.
Results
Among the 111 PCPs working in the region at the time of the study, 77 were met during the study period and asked to participate in the study, and all of them consented. Participants were mostly males (71.4%), with a mean age of 38.5 (SD 8.8) years and a mean duration of practice of 10.1 (SD 7.6) years. They received an average of 10.5 (SD 5.8) patients daily, and specifically 2.1 (SD 1.6) hypertensive patients.
Detection
Most of the PCPs (80.5%, n=62) measured BP for all adult patients in consultation, however, only 63.6% (n=49) of them used correct BP level for labeling a patient with hypertension, and 16.9% (n=13) used correct criteria for the diagnosis of hypertensive emergencies. About half of the PCPs used the correct number of required BP readings before assigning the hypertensive status (three readings), with an average of 2.7 (SD 0.6) measurements (Table 1).

Full table
Evaluation
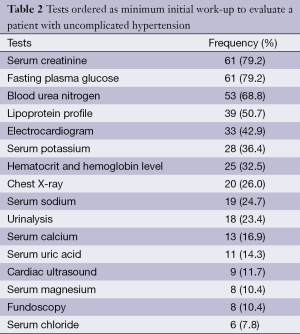
Sixty-seven PCPs (87.0%) ordered a minimal work-up for each newly diagnosed hypertensive patient, but only the work-up offered by eight participants was adequate (10.4%). The frequency of prescription of the minimal tests recommended by JNC 7 for the initial evaluation of uncomplicated hypertension was 32.5% for hematocrit and hemoglobin level, 79.2% and 68.8% for serum creatinine and blood urea nitrogen, 79.2% for fasting plasma glucose, 36.4% and 16.9% for serum potassium and calcium, 50.7% for lipoprotein profile (including high-density lipoprotein cholesterol, low-density lipoprotein cholesterol and triglycerides), 23.4% for urinalysis and 43.9% for electrocardiogram (Table 2).
Full table
Treatment
Recommendation of lifestyle modifications to patients was reported highly done (77.9%) in our study. While assessing prescribing practices, we found that five PCPs (6.5%) reported prescription of sedative drugs as their first-line antihypertensive treatment. The most commonly prescribed medications as monotherapy were loop diuretics (exclusively furosemide, 49.3%), thiazide diuretics (27.3%) and calcium channel blockers (23.4%). Bitherapy mostly included the combination of a diuretic and an angiotensin converting enzyme inhibitor (33.8%) or a diuretic and a calcium channel blocker (24.7%). Adequate treatment of hypertensive emergencies with injectable nicardipine was reported by 51.9% of PCPs (Table 3). Eight PCPs (10.4%) prescribed only antihypertensive originator brands, 15 (19.5%) only generics and 52 (67.5%) either generics or originator brands.

Full table
The correct target BP for patients without relevant cardiovascular comorbidities was aimed for by 44.2% of PCPs (n=34). The correct levels of target BP for patients with CVD, diabetes, and renal disease were aimed for by only 18.2% (n=14), 28.6% (n=22), and 23.4% (n=18) of PCPs, respectively. The general tendency was to use higher target levels. Some of these targets differed significantly among recent versus older medical school graduates (Table 1). Once BP control was achieved, 50 (64.9%) PCPs usually continued with the treatment, 25 (24.7%) reduced the dose and 2 (2.6%) stopped the treatment.
Sources of information
PCPs received updates on hypertension management mostly through drug companies representatives (53.2%, n=41), medical journals or internet (32.5%, n=25) and conferences (32.5%, n=25). Almost all PCPs (97.4%, n=75) were willing to receive continuing medical training on hypertension (Table 1).
Discussion
Hypertension control is a major challenge in LMIC where high BP has reached epidemic proportions becoming one of the leading cause of CVD and deaths (1). Physicians’ inability to provide good management of hypertension has been identified as an important contributor to poor BP control in hypertensive patients. In Cameroon, no previous study has investigated primary care doctors’ state of knowledge and practice patterns on the management of hypertension. This study was carried out to assess the knowledge and approach of PCPs in Cameroon towards the management of hypertension in accordance to the JNC 7 guidelines.
Studies have shown that hypertension is largely underdiagnosed and poorly controlled in most developing countries (5-11). Systematic screening for hypertension by BP measurement for all adults consulting in a health facility could contribute to improve the poor rates of diagnosis and treatment. Most PCPs (80.5%) in our study reported measuring BP for all adult patients in consultation, hence, an opportunity to diagnose unknown hypertensive patients. However, only 63.6% of them used correct BP thresholds for labeling a patient with hypertension, with a general tendency of using higher thresholds. Moreover, only 16.9% of PCPs used correct criteria for the diagnosis of hypertensive emergencies. Updating PCPs on the correct diagnosis criteria of hypertension would therefore contribute to increased rates of diagnosis and treatment in our setting.
A minimum work-up is recommended for the evaluation of hypertensive patients, along with clinical evaluation, to identify other cardiovascular risk factors or concomitant disorders that may affect prognosis and guide treatment, to reveal identifiable causes of hypertension, and to assess the presence or absence of target organ damage and CVD (20). Although 87% of PCPs in our study reported ordering investigations to evaluate patients with uncomplicated hypertension, only 10.4% asked an adequate minimum work-up as recommended by JNC 7. This finding is alarming since failure to identify other cardiovascular risk factors, target organ damage and CVD may lead to inadequate treatment and thus poor outcomes (20).
Hypertension treatment includes both lifestyle modifications and pharmacologic treatment. Lifestyle modifications reduce BP, prevent or delay the incidence of hypertension, enhance antihypertensive drug efficacy, and decrease cardiovascular risk (20). JNC 7 recommended lifestyle modifications for patients with prehypertension and no compelling indications, and its combination to drug therapy for those with established hypertension. These lifestyle modifications include weight reduction, adoption of the Dietary Approaches to Stop Hypertension (DASH), dietary sodium reduction, physical activity and moderation of alcohol consumption (20). Recommendation of lifestyle modifications to patients was reported highly done (77.9%) by the PCPs in our study. This finding contrasts with that of a study conducted in South Africa where only 50% of doctors indicated that they even mentioned lifestyle modifications to some of their patients (21). Such high awareness of the importance and advice of lifestyle treatments as found in our setting are very important, especially in primary care where preventive interventions are paramount and in low income settings where compliance to drug therapy is usually not optimal due to financial limitations. Indeed, effective lifestyle interventions may reduce the amount and cost of prescribed medications (20).
Although recommendation of lifestyle changes to patients were reported highly done in our study, we did not evaluate the knowledge of these lifestyle changes among our participants. Hence counseling on lifestyle modifications among our participants might be inadequate. Moreover, if the relative light patient load seen in this study might allow time for the physicians to provide counseling on lifestyle treatments to their patients, this could be very difficult in settings where physicians are facing overwhelming heavy patient load (15,21).
A large number of drugs are currently available for reducing BP. Besides thiazide diuretics are the least expensive hypertensive agents (20), there are compelling evidences that they confer the same or even better benefit in preventing the cardiovascular complications of hypertension compared to calcium channel blockers and angiotensin converting enzyme (ACE) inhibitors (20,22). Thiazide diuretics are therefore recommended as preferred initial agent alone or in combination (20). Unfortunately, thiazide diuretics were underprescribed in our setting, especially in monotherapy. Similarly, a study in the US has shown that despite the various benefits of thiazide diuretics, they remain underutilized (23). For a low income country like Cameroon where access to adequate health care is poor, effective and affordable hypertensive drugs such as thiazide diuretics should be highly utilized.
Whatever are the hypertensive drugs used, lowering BP to appropriate targets is the most important. Knowledge of adequate BP targets for hypertensive patients, especially for those with diabetes, chronic kidney disease or CVD was poor in this study, with a general tendency of using higher target levels. The use of inappropriate BP targets contribute significantly to poor rates of hypertension control and thus to persistent related-morbidity and mortality.
We also found that appropriate treatment of hypertensive emergencies were reported by only half of our PCPs. Up to 28.6% of them reported using sublingual nifedipine for this indication. The use of sublingual nifedipine should be avoided because of the risk of complications from unpredictable aggressive BP reduction (24,25).
As found in other developing countries (16,26), the practices of recent graduates from medical school were not better than those of older graduates. This means that even recent graduates from medical schools who are supposed to have updated knowledge are practicing inappropriate medicine. This finding highlight the need for the revision of the teaching curricula in medical schools with regard to the management of hypertension.
Another striking findings of this study is that PCPs relied mostly on pharmaceutical representatives for updates on the management of hypertension. Interestingly, some studies have suggested that limiting the influence of pharmaceutical industry on clinical practice would improve the treatment outcomes of patients with chronic diseases in primary care (27-30). Indeed, interactions between physicians and pharmaceutical representatives increase the chances that the physician will act contrary to duties owed to the patient. Ideally, a physician might both interact with pharmaceutical representatives and also do the research necessary to counteract the commercial bias in their message (27). Unfortunately, significantly less PCPs in our study searched for updates on hypertension management through medical journals or internet. In this situation, the publication of national guidelines could provide accepted consensus on best practice and help physicians to conform to standards.
In Cameroon, there are no guidelines for the management of hypertension provided by the National Diabetes-Hypertension Control Program. Although physicians can rely on the international guidelines published by either the JNC or the European Society of Hypertension (ESH)/European Society of Cardiology (ESC), it has been suggested that guidelines developed at local level with the consensus of clinicians would be most effective (31). Furthermore, as demonstrated by a Canadian randomized controlled trial, a simplified hypertension treatment algorithm could be significantly more effective than guideline-based practice (32). Such a hypertension treatment algorithm developed for local implementation in Cameroon should encourage the use of highly affordable and available antihypertensive drugs like thiazide diuretics.
Almost all our participants were willing to participate in training sessions on updated management of hypertension. Structured continuing medical training on hypertension alongside with the provision of a simplified hypertension treatment algorithm to PCPs would improve hypertension control in our setting as it has been demonstrated elsewhere (32-34).
Conclusions
PCPs’ knowledge and management of hypertension is poor in this region of Cameroon. There is a need for continually updating the teaching curricula of medical schools with regard to the management of hypertension. All physicians involved in the management of hypertensive patients should receive continuing medical education, and a simplified hypertension treatment algorithm should be conceived by local experts in order to develop minimum standards for coherence and uniformity in the management of hypertension. The use of low-price generic thiazide diuretics should be scaled up.
Acknowledgements
Authors’ contributions: Study conception and design: AMJ, JJNN; Data collection: AMJ, AEO; Statistical analysis: JJNN, AMJ; Drafting: JJNN, AMJ; Critical discussion and manuscript revision: JJNN, AMJ, SVW, AEO, EWY, SK. All the authors approved the final version of the manuscript.
Disclosure: The authors declare no conflict of interest.
References
- World Health Organization. Global Status Report on Non-communicable Diseases 2010. World Health Organization. Geneva, 2010.
- Lawes CM, Vander Hoorn S, Rodgers A, et al. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513-8. [PubMed]
- He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009;374:1765-72. [PubMed]
- Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362:1527-35. [PubMed]
- Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959-68. [PubMed]
- Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension 2013;62:18-26. [PubMed]
- Lloyd-Sherlock P, Beard J, Minicuci N, et al. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol 2014;43:116-28. [PubMed]
- Dzudie A, Kengne AP, Muna WF, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open 2012;2. [PubMed]
- Tantchou Tchoumi JC, Butera G. Profile of cardiac disease in Cameroon and impact on health care services. Cardiovasc Diagn Ther 2013;3:236-43. [PubMed]
- Ogah OS, Rayner BL. Recent advances in hypertension in sub-Saharan Africa. Heart 2013;99:1390-7. [PubMed]
- van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa--consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J 2013;16:38. [PubMed]
- Jingi AM, Noubiap JJ, Kamdem P, et al. The spectrum of cardiac disease in the West Region of Cameroon: a hospital-based cross-sectional study. Int Arch Med 2013;6:44. [PubMed]
- Jingi AM, Noubiap JJ, Yonta EW, et al. A Centre for the Diagnosis and Treatment of Tuberculosis (CDT) in a resource-limited setting: a dragnet for patients with heart disease? Arch Public Health 2014;72:26. [PubMed]
- Degli Esposti E, Di Martino M, Sturani A, et al. Risk factors for uncontrolled hypertension in Italy. J Hum Hypertens 2004;18:207-13. [PubMed]
- Düsing R. Overcoming barriers to effective blood pressure control in patients with hypertension. Curr Med Res Opin 2006;22:1545-53. [PubMed]
- Jafar TH, Jessani S, Jafary FH, et al. General practitioners’ approach to hypertension in urban Pakistan: disturbing trends in practice. Circulation 2005;111:1278-83. [PubMed]
- Hyman DJ, Pavlik VN, Vallbona C. Physician Role in Lack of Awareness and Control of Hypertension. J Clin Hypertens (Greenwich) 2000;2:324-330. [PubMed]
- 3eme recensement general de la population humaine. La population du Cameroun en 2010;2010. Available online: http://www.statistics-cameroon.org/downloads/La_population_du_Cameroun_2010.pdf
- Hyman DJ, Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med 2000;160:2281-6. [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560-72. [PubMed]
- Parker A, Nagar B, Thomas G, et al. Health practitioners’ state of knowledge and challenges to effective management of hypertension at primary level. Cardiovasc J Afr 2011;22:186-90. [PubMed]
- ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981-97. [PubMed]
- Psaty BM, Manolio TA, Smith NL, et al. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med 2002;162:2325-32. [PubMed]
- O’Mailia JJ, Sander GE, Giles TD. Nifedipine-associated myocardial ischemia or infarction in the treatment of hypertensive urgencies. Ann Intern Med 1987;107:185-6. [PubMed]
- Grossman E, Messerli FH, Grodzicki T, et al. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA 1996;276:1328-31. [PubMed]
- Al-Azzam SI, Najjar RB, Khader YS. Awareness of physicians in Jordan about the treatment of high blood pressure according to the seventh report of the Joint National Committee (JNC VII). Eur J Cardiovasc Nurs 2007;6:223-32. [PubMed]
- Brody H. The company we keep: why physicians should refuse to see pharmaceutical representatives. Ann Fam Med 2005;3:82-5. [PubMed]
- Hunt LM, Kreiner M, Brody H. The changing face of chronic illness management in primary care: a qualitative study of underlying influences and unintended outcomes. Ann Fam Med 2012;10:452-60. [PubMed]
- Westfall JM. Physicians, pharmaceutical representatives, and patients: who really benefits? J Fam Pract 2000;49:817-9. [PubMed]
- Figueiras A, Caamaño F, Gestal-Otero JJ. Influence of physician’s education, drug information and medical-care settings on the quality of drugs prescribed. Eur J Clin Pharmacol 2000;56:747-53. [PubMed]
- Mashru M, Lant A. Interpractice audit of diagnosis and management of hypertension in primary care: educational intervention and review of medical records. BMJ 1997;314:942-6. [PubMed]
- Feldman RD, Zou GY, Vandervoort MK, et al. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension 2009;53:646-53. [PubMed]
- Goldstein MK, Hoffman BB, Coleman RW, et al. Implementing clinical practice guidelines while taking account of changing evidence: ATHENA DSS, an easily modifiable decision-support system for managing hypertension in primary care. Proc AMIA Symp 2000;300-4. [PubMed]
- O’Connor PJ, Quiter ES, Rush WA, et al. Impact of hypertension guideline implementation on blood pressure control and drug use in primary care clinics. Jt Comm J Qual Improv 1999;25:68-77. [PubMed]


