Are dilated ascending aortas of Chinese patients more likely to dissect?
Introduction
The natural evolution of ascending aortic aneurysm without treatment might lead to aortic dissection or rupture, even death (1,2). According to Laplace’s law, as the diameter of the aneurysm increases, the tension of the arterial wall increases. Therefore, it is commonly known that dilated aortas are more likely to dissect (3). Regardless of etiology, surgery should be performed in patients with simple aortic dilation who have a maximal aortic diameter larger than 5.5 cm according to 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases (4). In our usual consciousness, dissection often occurs when the diameter of the aneurysm increases to a certain extent and the diameter of aortic dissection is always larger than the diameter of aortic aneurysm. However, the average diameter of ascending aorta when the aortic dissection occurred is always controversial worldwide (5-7). It makes us begin to examine the correctness of the aortic diameter alone as a surgical indication.
When is the best time to operate? Various surgeons have different opinions. In our study, we compared the ascending aortic diameter and the ascending aortic diameter index between simple ascending aortic dilation group and simple ascending aortic dissection group, and also compared male and female differences between the two groups respectively. The aim of our study was to investigate the accuracy of the timing of operation determined by ascending aortic diameter alone. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/cdt-20-313).
Methods
Patient’s data
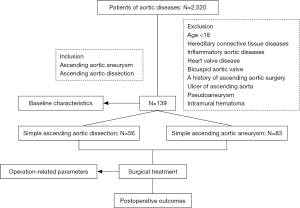
The trial was conducted in accordance with the Declaration of Helsinki. The present study was granted by the Ethics Committee of Beijing Anzhen Hospital (Institutional Review Board File 2014019), and informed consent was taken from all the patients. We collected 2,520 hospitalized patients of aortic dilation and aortic dissection who underwent surgical treatment from January 2010 to June 2017 in Beijing Anzhen Hospital of Capital Medical University. All the disorders only involved the ascending aorta. The diameters of ascending aorta and aortic sinus were determined by transthoracic echocardiography database of the Beijing Anzhen Hospital. In order to exclude some interference factors which are not related to this research, we only identified simple ascending aortic dissection (the simple aortic dissection means the dissection of the ascending aorta alone, and this kind of dissection had been verified through both the preoperative CTA scans and intraoperative detection) and simple ascending aortic dilation (the simple aortic dilation means the dilation of the ascending aorta alone). And the other exclusion criteria included: age <18, hereditary connective tissue diseases such as Marfan syndrome, Loeys-Dietz, and Ehlers-Danlos syndromes; inflammatory aortic diseases; heart valve diseases such as aortic stenosis or insufficiency and bicuspid aortic valve, and a history of ascending aortic surgery. In addition, patients with pseudoaneurysm, ulcer of the ascending aorta and intramural hematoma were also excluded. We finally identified 139 patients in the two groups, 83 in the aortic dissection group and 56 in the aortic dilation group (Figure 1). Since these patients had only ascending aortic disorder, they all had the ascending aortic replacement with the peripheral artery cannulation. The data collection was mainly from medical records of the patients in hospital. The clinical data included diameter of ascending aorta, diameter of aortic sinus, sex, age, height, weight, body surface area, preoperative EF, preoperative LVEDD, preoperative LVESD, left atrial diameter, operation related parameters and postoperative outcomes.
Statistical analysis
The continuous variable of normal distribution is expressed by mean ± standard deviation. The abnormal distribution data is represented by median (interquartile range), and the categorical variable is expressed as a percentage. The t-test and univariable analysis were used to compare the differences between two groups.
Results
Baseline characteristics
A total of 139 patients met the criteria for inclusion. The comparison of basic data is shown in Table 1. At baseline, The age of patients in the aortic dilation group was 57.27±10.96, the age of patients in the aortic dissection group was 56.93±10.74, the age and the proportion of women in the two groups was similar, in addition, there was no significant statistical difference between the two groups, such as height, weight, body surface area, body mass index, preoperative EF, preoperative LVEDD, preoperative LVESD, left atrial diameter etc. before surgery.
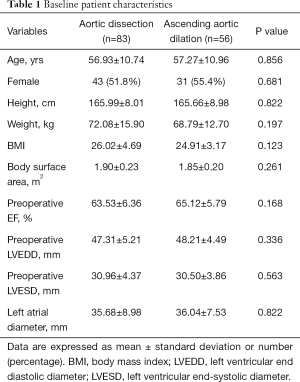
Full table
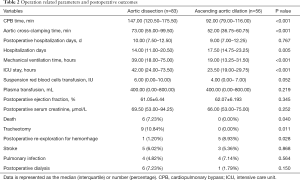
Operation related parameters and postoperative outcomes
Among patients in the dissection group, more CPB time, more aortic cross-clamping time, less hospitalization days, more mechanical ventilation time and longer ICU stay were present which was shown in Table 2. There was no significant statistical difference between the two groups, such as postoperative hospital days, suspension red blood cells transfusion, plasma transfusion, postoperative ejection fraction and postoperative serum creatinine. For postoperative outcomes, the dissection group had higher mortality, incidence of tracheotomy and postoperative re-exploration for hemorrhage. The incidence of stroke, pulmonary infection and postoperative dialysis between the two groups were similar.
Full table
Ascending aortic diameters
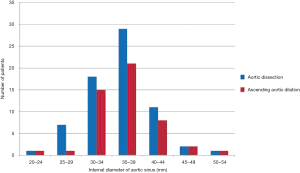
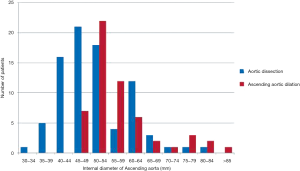
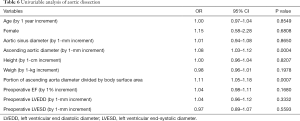
We can find out in Table 3, among the 139 patients, that the mean ascending aortic diameter of the dissection group was 50.72±9.53 mm and the mean ascending aortic diameter of the dilation group was 57.30±9.41 mm. The dilation group had greater ascending aortic diameter compared with the dissection group. For the aortic sinus diameter, there was no significant statistical significance between the two groups (Figure 2). Nearly 73% of the patients of the dissection group had aortic diameters <5.5 cm, and 52% of the patients had aortic diameters <5 cm (Figure 3). If we considered the influence of body surface area, we used the index of ascending aortic diameter, which was equal to the diameter of ascending aorta/body surface area. We could conclude from Table 3 that the dilation group had greater index of ascending aortic diameter compared with the group of dissection. This was consistent with the result of ascending aortic diameter. After that, we divided the two groups into male group and female group which were compared respectively. We found that male group and female group had different results which were shown in Tables 4 and 5. For male patients, the ascending aortic diameter and the index of ascending aortic diameter of the dilation group was greater compared with the dissection group. However, the aortic sinus diameter was similar between the two groups. But for female patients, there was no significant statistical significance between the two groups including the aortic sinus diameter, the ascending aortic diameter and the index of ascending aortic diameter. In order to eliminate interference from other confounding factors, we used univariable binary logistic regression analysis, which was shown in Table 6.

Full table

Full table

Full table
Full table
Discussion
The surgical indication for simple aortic dilation was set in 5.5 cm, which comes from the guideline of American College of Cardiology (ACC), American Heart Association (AHA), Society of Thoracic Surgery (STS) and the American Association for Thoracic Surgery (AATS) in the year of 2010 (8). Coady et al. (9) also put forward a lot of clinical evidence in 1997 to support this surgical indication. The guideline was mainly based on the experience accumulated by clinicians and surgeons, and lacked sufficient evidence support and theoretical basis (10-13). At the same time, the guideline implied that these indications were not absolute, and the influence of many other factors should be considered. The surgical indication for patients with Marfan syndrome was 5 cm, and for patients with additional risk factors, consisting of family history of dissection and severe aortic regurgitation, the indication could be reduced to 4.5 cm (8). As seen from the guidelines, genetic factors, valve disorders and so on had a great influence on surgical indications. So in our study, we excluded the interference caused by genetic factors, inflammation, valve disorders, etc., and chose simple ascending aortic dilation and simple ascending aortic dissection as the subjects for our study. This allowed us to focus on the effect of aortic diameter on indications for ascending aortic dilation and the two groups of patients were more comparable.
Our clinical data from Anzhen Hospital showed that in 83 aortic dissection patients, nearly 73% of the patients were less than 5.5 cm in diameter, and nearly 52% were less than 5 cm. Pape et al. (14) showed similar data in his article in 2007. This article enrolled 591 type A dissection patients (mean age, 60.8 years) from International Registry of Acute Aortic Dissection (IRAD) between 1996 and 2005. It was found that 59% of the patients were less than 5.5 cm in diameter and 40% were less than 5 cm, which was similar to our article. According to our data, most patients in dissection group had diameters <5.5 cm. If current indications were applied, these patients would face the risk of death. For some patients, the diameter of ascending aorta when aortic dissection occurrence was even normal. In clinical practice, we do find that some patients had suffered aortic dissection, although they have a “small aorta” or even less than 3.5 cm. On the contrary, in some patients of aortic dilation, the diameter of ascending aorta sometimes even reaches 8–9 cm and it was still “safe”, so, for these “small aorta” patients, it seems to be necessary to use more radical surgical indications to avoid disastrous aortic diseases, but for some “big aorta” patients, 5.5 cm appears too radical. This fact indicates that it is not enough to rely solely on diameter of the aorta to decide whether or not to operate. It is necessary to find more accurate evaluation indexes for the surgery.
Traditionally, we believed that the diameter of ascending aortic dilation was less than the diameter of ascending aortic dissection. With the increase of the diameter of the aorta, the risk of dissection increases, which means that the diameter of the aorta is “large enough”, causing the occurrence of aortic dissection under this diameter. However, our research was different from this. Many doctors believed that aortic diameter was still interfered by many factors, gender and body surface area are two important factors. Davies et al. (15) reviewed 805 patients of aortic aneurysm and found that the incidence of dissection in female was higher and the 5-year survival rate was lower. Cheung et al. (16,17) found that aortic diameter increased faster in women patients of aortic aneurysm. In order to exclude the interference of sex factors, we divided the patients into two groups, male and female, and it had different results. The diameter of the ascending aorta in female patients appeared to be thicker than that in male patients. We also recognized the effect of body surface area on the diameter of the aorta. Kälsch et al. (18) found out that BSA is an independent factor associated with increased aortic diameter. In order to exclude the interference of this factor, we compared the parameter of the ascending aortic diameter/body surface area between two groups, which was called the aortic diameter index, and found it was consistent with the results of aortic diameter. Davies et al. (15) believed that surgical treatment should be performed in patients of aortic aneurysm when the aortic diameter index reaches 2.75 cm/m.
In another study, some scholars believed that the diameter of the aorta presented the so-called “normal distribution” in the population, and the number of the middle aorta was largest, which meant that the population of the “smaller diameter” aorta had a relatively larger population, so the number of aortic dissection was also larger than that of “larger diameter” aorta (19,20). They confirmed that although aortic dissections did occur at small sizes, patients with large aortas were at a 6,000-fold higher risk of experiencing aortic dissection. If we want to measure the risk of occurrence of aortic dissection, the number of patients with aortic dissection/the total population of that diameter should be measured. The result was that the risk of aortic dissection in the larger diameter was significantly larger than the smaller diameter, which explained why 5.5 cm was used as a surgical indication for ascending aortic dilation. However, in the actual situation, the data of the aorta diameter of the total population is difficult to collect. Therefore, whether diameter of the aorta in the general population is normally distributed still needs further evidence. Besides, although the risk of aortic dissection occurrence in small aortas is less than large aortas, the population of people with small aortas is quite large, so the absolute number of patients of aortic dissection in small aortas is very large too, which can’t be ignored in clinical practice. In our study, the dissection group had higher mortality, incidence of tracheotomy and postoperative re-exploration for hemorrhage. It suggested that once aortic dilation developed into aortic dissection, the perioperative mortality and morbidity would be significantly increased, and the risk of surgical intervention for the patients with aortic dilation would be much lower before aortic dissection occurrence.
In China, there is no database platform like IRAD yet. It is difficult to summarize the experience of diagnosis and treatment of ascending aortic dilation and hard to get evidence-based medical researches. At present, cardiac surgeons in China rely more on European and American guidelines to guide clinical work. Our existing indications for ascending aortic dilation are also based on these European and American guidelines. As everyone knows, there is a big difference between Chinese and European or American race, so it is necessary to establish an indication of surgery for ascending aortic dilation that belongs to the Chinese. This article is to investigate the diameter of the aorta and the risk of aortic dissection occurrence in Chinese, but there is still a lot of work to do before we have our own guidelines.
There were also some limitations in our article. We excluded the hereditary and inflammatory aortic diseases in the selection of cases, which may be a key to unlock the “silent killer” secrets of the aortic dilation. Besides, it should be noted that our research mostly included only ascending aortic diameters post-dissection, which was known to be roughly 13 mm larger compared to pre-dissection (21). And more than 60% of patients have non-dilated aortas prior to the dissection (22). But the pre-dissection diameter was the real diameter at risk. So, the actual diameter of aorta when aortic dissection occurred was smaller than expected. Did it mean that the current surgical indication was wrong? For ascending aortic dilation, should we adopt a more aggressive surgical strategy? Apart from these, Wu et al. referred that ascending aortic length could serve as a novel predictive factor to evaluate risk of aortic adverse events, which include aortic rupture, aortic dissection and death and raised that aortic elongation of 11 cm should be a new indication for aortic intervention. It is a completely new criterion for aortic surgery and needs to be further verified. We did not assess the quality of this factor in our research because we paid more attention to the existed criterion of surgery. But it certainly should be one of our next research interests to check its effectiveness (23).
In the future, we will further explore the pathogenesis of the aortic dilation. At the same time, the factors that affect the diameter of the aorta in this article only include gender and body surface area, and there are still some other factors that are not involved. This is the problem we need to further study in the future.
Conclusions
The majority of patients with aortic dissection present with aortic diameters <5.5 cm and this is not consistent with the current indications of aortic dilation. The group of aortic dilation has greater ascending aortic diameter and the index of ascending aortic diameter compared with the group of aortic dissection. And for male and female patients, it has different results. It is far from enough to predict the occurrence of aortic dissection with aortic diameter alone. We need better risk predictors to identify patients at risk and individualized surgical indications should be applied to different patients.
Acknowledgments
Thanks to the collection of clinical data used in this paper by Haiyang Li, Ming Gong, Xiaolong Wang and others.
Funding: This study was supported by National Key R&D Program of China (No. 2017YFC1308000); National Natural Science Foundation of China (No. 81800404); Capital Health Development Research Project (No. 2018-4-2068); Beijing Municipal Administration of Hospitals’ Youth Program (No. QML20180601); Foundation of Beijing Outstanding Young Talent Training Program (No. 2017000021469G254); Beijing Lab for Cardiovascular Precision Medicine (No. PXM2017_014226_000037).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/cdt-20-313
Data Sharing Statement: Available at http://dx.doi.org/10.21037/cdt-20-313
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/cdt-20-313). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of Beijing Anzhen Hospital (Institutional Review Board File 2014019), and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Olsson C, Thelin S, Stahle E. Thoracic aortic dilation and dissection: Increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14,000 cases from 1987 to 2002. J Vasc Surg 2007;46:609. [Crossref]
- Mészáros I, Morocz J, Szlavi J, et al. Epidemiology and clinicopathology of aortic dissection. Chest 2000;117:1271-8. [Crossref] [PubMed]
- Szilagyi DE, Smith RF, Derusso FJ, et al. Contribution of abdominal aortic dilationectomy to prolongation of life. Ann Surg 1966;164:678-99. [Crossref] [PubMed]
- Erbel R, Aboyans V, Boileau C, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35:2873-926. [Crossref] [PubMed]
- Dapunt OE, Galla JD, Sadeghi AM, et al. The natural history of thoracic aortic dilations. J Thorac Cardiovasc Surg 1994;107:1332-3. [Crossref]
- McNamara JJ, Pressler VM. Natural History of Arteriosclerotic Thoracic Aortic Dilations. Ann Thorac Surg 1978;26:468-73. [Crossref] [PubMed]
- Crawford ES, Hess KR, Cohen ES, et al. Ruptured dilation of the descending thoracic and thoracoabdominal aorta. Analysis according to size and treatment. Ann Surg 1991;213:417-25. [Crossref] [PubMed]
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology,American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. J Am Coll Cardiol 2010;55:e27-129. [Crossref] [PubMed]
- Coady MA, Rizzo JA, Hammond GL, et al. What is the appropriate size criterion for resection of thoracic aortic dilations? J Thorac Cardiovasc Surg 1997;113:476-91; discussion 489-91. [Crossref] [PubMed]
- Coady MA, Rizzo JA, Elefteriades JA. Developing surgical intervention criteria for thoracic aortic dilations. Cardiol Clin 1999;17:827-39. [Crossref] [PubMed]
- Ergin MA, Spielvogel D, Apaydin A, et al. Surgical treatment of the dilated ascending aorta: when and how? Ann Thorac Surg 1999;67:1834-9. [Crossref] [PubMed]
- Gott VL, Greene PS, Alejo DE, et al. Replacement of the aortic root in patients with Marfan’s syndrome. N Engl J Med 1999;340:1307-13. [Crossref] [PubMed]
- Borger MA, Mark P, Joan I, et al. Should the ascending aorta be replaced more frequently in patients with bicuspid aortic valve disease? J Thorac Cardiovasc Surg 2004;128:677-83. [Crossref] [PubMed]
- Pape LA, Tsai TT, Isselbacher EM, et al. Aortic Diameter ≥5.5 cm Is Not a Good Predictor of Type A Aortic Dissection Observations From the International Registry of Acute Aortic Dissection (IRAD). Circulation 2007;116:1120-7. [Crossref] [PubMed]
- Davies RR, Amy G, Coady MA, et al. Novel measurement of relative aortic size predicts rupture of thoracic aortic dilations. Ann Thorac Surg 2006;81:169-77. [Crossref] [PubMed]
- Jue J, Boodhwani M, Beauchesne L, et al. Sex Differences in the Associations of Arterial Stiffness and Pulsatile Hemodynamics with Thoracic Aortic Dilation Size. Canadian J Cardiol 2018;34:e6. [Crossref]
- Cheung K, Boodhwani M, Chan KL, et al. Thoracic Aortic Dilation Growth: Role of Sex and Dilation Etiology. J Am Heart Assoc 2017;6:e003792. [Crossref] [PubMed]
- Kälsch H, Lehmann N, Mohlenkamp S, et al. Body-surface adjusted aortic reference diameters for improved identification of patients with thoracic aortic dilations: results from the population-based Heinz Nixdorf Recall study. Int J Cardiol 2013;163:72-8. [Crossref] [PubMed]
- Paruchuri V, Salhab KF, Kuzmik G, et al. Aortic Size Distribution in the General Population: Explaining the Size Paradox in Aortic Dissection. Cardiology 2015;131:265. [Crossref] [PubMed]
- Elefteriades JA, Ziganshin BA. Gratitude to the International Registry of Acute Aortic Dissection From the Aortic Community. J Am Coll Cardiol 2015;66:359-62. [Crossref] [PubMed]
- Rylski B, Blanke P, Beyersdorf F, et al. How does the ascending aorta geometry change when it dissects? J Am Coll Cardiol 2014;63:1311-9. [Crossref] [PubMed]
- Rylski B, Branchetti E, Bavaria JE, et al. Modeling of predissection aortic size in acute type A dissection: More than 90% fail to meet the guidelines for elective ascending replacement. J Thorac Cardiovasc Surg 2014;148:944-8.e1. [Crossref] [PubMed]
- Wu J, Zafar MA, Li Y, et al. Ascending Aortic Length and Risk of Aortic Adverse Events: The Neglected Dimension. J Am Coll Cardiol 2019;74:1883-94. [Crossref] [PubMed]