
Current status on the ability of the elderly in rural China: implications for future nursing and policy
Introduction
It’s been reported that the number of the elderly aged ≥60 years in China has reached 212 million, accounting for 15.5% of the total population (1). It’s been well-acknowledged that with the increase of age, the elderly has more chances of suffering from various chronic diseases (2). Based on previous report, the prevalence of chronic diseases among the elderly aged over 60 in China is as high as 75% (3). Chronic diseases have the characteristics of long course, slow recovery, and many related complications, which can lead to physical dysfunction (4). In the end of 2019, the number of elderly people with disabilities in China has exceeded 46 million, and it is growing at a rate of 3% per year (5). Therefore, understanding the current physical and mental status of the elderly in China is essential to the policy making and nursing care for this population.
Disability refers to the impaired physical and mental function or limited cognitive ability to engage in daily activities and requires the assistance of others. A large group of disabled elderly people needs huge long-term care services (6). With the intensification of the aging population and the continuous improvement of the socio-economic level, the long-term care needs of disabled elders around the world are increasing and showing diverse characteristics (7). At the same time, the government in China has begun to pay attention to the long-term care of disabled elders. The Chinese government clearly proposes to build an old-age service system based on home, community-support, and a combination of medical care and elderly care service system to better meet the needs of the elderly (8).
At present, there are many studies on the care of the elderly with disability in China, but most of them focus on the research on the models of care for the elderly. However, there are very few researches on the evaluation of current status and related factors of the elderly in China. Previous scholar (9) has pointed out that the evaluation of body function and disability in the care of the elderly is a very critical. To elucidate the care needs of the elderly, we must first understand how to assess the functional status of the elderly and how to define and measure disability. And as the American Academy of Medicine (10) pointed out, the goal of health care is to improve human health and body function and the purpose of geriatrics is to pay attention to the maintenance and recovery of elderly functions. Furthermore, most study subjects in previous studies (11,12) have been focused on the urban residents but not rural residents, the current status of the elderly in rural China remains unclear. Therefore, accurate assessment of physical and mental function and disability is not only critical for achieving health care for the elderly, but also important in evaluating the effects of interventions that may delay and prevent the progression of disability in the elder population (13). In this present study, we aimed to conduct a large-scale survey to evaluate the current status on the ability of the population of elderly in the rural of China, to provide insights into future nursing care for the elderly. In this present study, the study PICO design was as following. Participants: the elderly in 20 rural villages; Intervention: questionnaire surveys; Comparison: not applicable; Outcomes: the ability scores of the elderly. We present the following article in accordance with the SURGE-reporting checklist (available at http://dx.doi.org/10.21037/cdt-20-555).
Methods
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This present survey had been certified and approved by the ethical committee of Jinggangshan University (No. 2020032), and written informed consents had been obtained from all the included participants.
Participants
Convenience sampling method was used to identify the potential participants. The elderly in 20 rural villages of Ji’an City, Jiangxi Province were selected as the survey subjects. The inclusion criteria were as following: (I) age ≥60 years old; (II) well informed and voluntary to participate in this survey; (III) were literate self with good listening and speaking skills, or had family members or community staff who were familiar with the current situation of the elderly, and could provide relevant information. The exclusion criteria were: (I) those with illiteracy or who could not cooperate with accomplishment of survey; (II) unwilling to participant in this survey.
Ability assessment
This study used the “Elderly Ability Evaluation Form” issued by the Ministry of Civil Affairs of the People’s Republic of China as the survey tool (14,15). The tool includes two parts: the basic information for the elderly and the elderly ability evaluation. The assessment of the ability of the elderly included following four parts: activities of daily living, mental state, perception and communication, and social participation. The scores varied 0 to 100 points, 0 to 6 points, 0 to 14 points, and 0 to 20 points for each part. Each dimension is divided into intact ability, mild disability, moderate disability and severe disability accordingly.
Survey process
A total of 10 teachers, students and nurses from our school formed a research team. After standardized training, they entered various villages in June 2019 to conduct relevant research. During the survey, every two researchers formed a group to complement and check each other. Each item of the questionnaire in the survey is queried and filled out by the respondents. It took 15 to 20 min to fill out each questionnaire.
Data analysis
After two authors double checked the collected data, all the data were input into SPSS 23.0 statistical software for data analysis. We preformed descriptive analyses on the characteristics and scores of respondents. Analysis of variance and t test were used to analyze the characteristics and score differences of the elderly, Spearman rank correlation and Pearson correlation analysis were performed to evaluate the characteristics of elders and related scores. Logistic regression analyses were conducted to identify the potential risk factors for disability in the elderly (16). P<0.05 was considered statistically significant in this study, all of the tests were two-sided.
Results
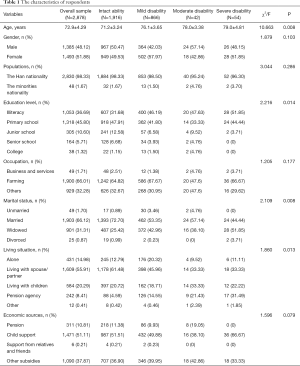
The characteristics of respondents
We initially identified 3,000 potential elders for this survey and received 2,878 qualified answers, with an overall response rate of 95.93%. As Table 1 presented, among the included 2,878 elders, there were 1,916 elders with intact ability, 866 elders with mild disability, 42 elders with moderate disability, 54 elders with severe disability. The incidence of disability among the respondents was 33.43%. There were significantly statistical differences on the age, education level, marital status and living situations among respondents (all P<0.05). And no significantly statistical differences were found on the gender, populations, occupation and economics sources (all P>0.05).
Full table
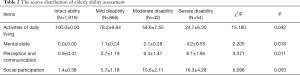
The score distribution
As Table 2 presented, there were significantly statistical differences on the dimensions of activities of daily living, mental state, perception and communication, and social participation among elders with intact ability, mild, moderate and severe disability (all P<0.05).
Full table
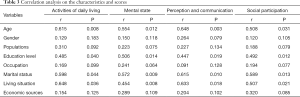
Correlation analysis on the characteristics of elders and scores
As Table 3 showed, the age, education level, marital status and living situations were all corrected with the scores on the activities of daily living, mental state, perception and communication, and social participation among elders (all P<0.05). And the gender, populations, occupation and economics sources were not correlated with the scores on the activities of daily living, mental state, perception and communication, and social participation among elders (all P>0.05).
Full table
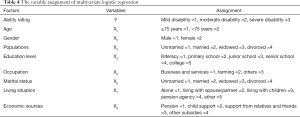
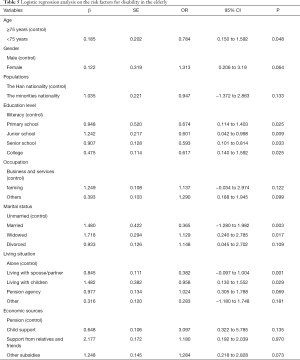
The risk factors for disability in the elderly
We use the disability level of the elderly as the dependent variable, and the potential influencing factors as the independent variable to conduct the logistic regression analysis. The variable assignments of multivariate logistic regression were indicated in Table 4. As Table 5 presented, the age, education level, marital status and living situations were the independent influencing factors for the disability in the elderly (all P<0.05), indicating that the elderly with age ≥75 years, illiteracy, unmarried and live alone had higher risk for disability.
Full table
Full table
Discussion
At present, the aging of the population has become an obstacle to the development of countries around the world and it has attracted worldwide attentions. Compared with developed countries, China’s aging problem is even more prominent. Compared with the aging process of the international community for tens or even hundreds of years, China has entered the era of aging in less than 30 years (17). Moreover, China’s aging population is also characterized by aging, empty nesting, high disability rate, and high incidence of chronic diseases, which makes the challenge of aging in China more severe (18). In the next 20 years, China will enter a period of rapid growth of the elderly population, and the size and number of disabled elders will inevitably continue to increase accordingly, and the problems related to the elderly will also surge (19). However, a fact that cannot be ignored is that, on the one hand, the total amount of demand for health care by the disabled elderly is increasing (20). On the other hand, the traditional care function undertaken by the family for elders is decreasing with industrialization, urbanization, and smaller family size (21). If this contradiction between demand and supply is not improved, it will surely become a major social problem affecting the life quality of elders and the future sustainable development of society (22). In our survey, the incidence of disability among the rural elders was 33.43%, which is higher than that of previous reports which focused on the urban residents, indicating that problems of old-age service are more severe in the rural area in China. Furthermore, we have found that the age, education level, marital status and living situations are corrected with the activities of daily living, mental state, perception and communication, and social participation among rural elders, future policy and nursing care on the services for rural elders should be targeted on those factors.
The older the age, the more severe of the disabled in the elders, thereby the longer they need long-term care (23). Scholars (24,25) have found that the long-term care needs of the elderly in poor rural areas that the proportion of those who require long-term care has increased by nearly 38.1% compared with the older age group (≥80 years old) and the lower age group (60–69 years old). It may be because the elderly with older age have a higher prevalence of chronic diseases and the risk of disability and dementia (26). At the same time, previous surveys (27,28) have found that the age-gradient of hypertension occurrence is obvious, the prevalence of low, middle and high age groups is 60%, 72% and 77% respectively. However, the control rate of hypertension in rural China is rather low, only 5% patients diagnosed with hypertension may take the regimes (29). Lin et al. (30) showed that age is one of the important factors that affect the rise of long-term care for demented elderly. With the increase of age, the physical and mental condition often deteriorates and repeats. It requires continuous long-term care to meet the balance of physical and mental state of the elders. It is foreseeable that with the further intensification of aging in the future, the proportion of the elderly who need long-term care in rural China will also increase.
This survey has found that total scores of married and living with others are better than that of unmarried and live alone. Most unmarried elders live alone or with non-immediate relatives, and widowed or divorced elders mostly live with their children or live alone (31). In addition, according to previous research (32), the relationship network in Chinese society presents a “differentiated pattern”. Immediate relatives have the closest relationship with the elderly, while non-immediate relatives are naturally not as careful and thoughtful as spouses and children (33). Therefore, not only for the elderly living alone, but also for the elderly who do not live with their immediate family members, more attentions and care services are needed to improve their life quality.
Affected by traditional culture, the elderly is reluctant to leave their familiar environment or community to go to the institutions of nursing care, which is particularly evident in rural China (34). Previous studies (35,36) have shown that 73.2% of disabled elders are more willing to choose home and community care. However, the role of the community in health care for the aged is still quite limited. Most elderly people do not take advantage of the services provided by the community, and a large proportion of the elderly do not know what services the community provides (37). Therefore, it’s necessary to vigorously promote the development of rural community health care services for the disabled. Rely on village health service centers and other professional institutions, the social groups, community volunteers, non-governmental organizations and other social forces should be combined to establish professional service, to provide on-site services or multi-level care services for the disabled elderly, including physical function rehabilitation and mental comfort.
Interestingly, this study did not find a correlation between economic income and the ability of rural elderly. This may be related to the fact that the economic level of the elderly in rural areas is generally low (38). Economic income is an important factor affecting the choice of care mode. It’s been reported that about half of the disabled elderly said that they did not choose a professional institution for care because they could not afford it (39). Furthermore, previous studies (40,41) have reported the disabled elderly with higher monthly income are more willing to choose professional institutions to provide care services. However, the current long-term care services for the disabled elderly are not covered by the basic medical insurance in China (42). The disabled elderly may be reimbursed for some medical expenses through inpatient treatment of other diseases (43). Although at this stage the disabled elderly still mainly rely on the help of spouses and children to provide care, but in the future, with the further increase of disabled elderly, and the family size continues to decrease, the nursing care provided by children and families is becoming more and more inadequate, and the demand for nursing care services provided by professional institutions or other social organizations will be greater (25,44). Thus, the cost of care for disabled elderly will increase in the future, future policies targeted on this issue are highlighted (45).
Conclusions
In conclusions, the overall ability of the elderly in rural China is poor, the age, education level, marital status and living situations are associated with the activities of daily living, mental state, perception and communication, and social participation of rural elders. Furthermore, the elderly with age ≥75 y, illiteracy, unmarried and live alone had higher risk for disability. The government and health care providers should provide long-term, continuous and effective long-term care services for the elders in rural China, from the aspects of establishing long-term care evaluation standards and strengthening the interaction targeted on those influencing factors. However, limited by the local region and small sample size, our results should be understood with cautions, future studies on the ability assessment of elderly with larger sample are needed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors present the study in accordance with the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/cdt-20-555
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/cdt-20-555). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This present survey had been certified and approved by the ethical committee of Jinggangshan University (No. 2020032), and written informed consents had been obtained from all the included participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li L, Zhang R, Chen Y, et al. Achievements and challenges in health management for aged individuals in primary health care sectors: a survey in Southwest China. BMC Public Health 2020;20:338-46. [Crossref] [PubMed]
- Li T, Fang Y, Zeng D, et al. Developing an Indicator System for a Healthy City: Taking an Urban Area as a Pilot. Risk Manag Healthc Policy 2020;13:83-92. [Crossref] [PubMed]
- Fang EF, Scheibye-Knudsen M, Jahn HJ, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev 2015;24:197-205. [Crossref] [PubMed]
- Leng SX, Liu B, Kennedy BK. Aging mechanisms and interventions that impact senior health: Introduction to a special issue on Geroscience. Aging Med (Milton) 2019;2:126-9. [Crossref] [PubMed]
- Yang F, Qian D, Hu D. Life-course and Cohort Trajectories of Chronic Non-communicable Diseases Risk Factors in China. Iran J Public Health 2017;46:591-601. [Crossref] [PubMed]
- Zhu W, Chi A, Sun Y. Physical activity among older Chinese adults living in urban and rural areas: A review. J Sport Health Sci 2016;5:281-6. [Crossref] [PubMed]
- Ma S, Shi J, Li L. Dilemmas in caring for older adults in Zhejiang Province, China: a qualitative study. BMC Public Health 2019;19:311. [Crossref] [PubMed]
- Zeng Y, Hu X, Li Y, et al. The Quality of Caregivers for the Elderly in Long-Term Care Institutions in Zhejiang Province, China. Int J Environ Res Public Health 2019;16:2164. [Crossref] [PubMed]
- Feng Z, Cramm JM, Nieboer AP. A healthy diet and physical activity are important to promote healthy ageing among older Chinese people. J Int Med Res 2019;47:6061-81. [Crossref] [PubMed]
- Elder NC, Imhoff R, Chubinski J, et al. Congruence of Patient Self-Rating of Health with Family Physician Ratings. J Am Board Fam Med 2017;30:196-204. [Crossref] [PubMed]
- Zhang L, Ding Z, Qiu L, et al. Falls and risk factors of falls for urban and rural community-dwelling older adults in China. BMC Geriatr 2019;19:379. [Crossref] [PubMed]
- Xie L. Age-Friendly Communities and Life Satisfaction Among the Elderly in Urban China. Res Aging 2018;40:883-905. [Crossref] [PubMed]
- Zhou Z, Zhou Z, Gao J, et al. Urban-rural difference in the associations between living arrangements and the health-related quality of life (HRQOL) of the elderly in China-Evidence from Shaanxi province. PLoS One 2018;13:e0204118. [Crossref] [PubMed]
- Chen S, Cui Y, Li X. Survey on Comprehensive Ability and Analysis of Influencing Factors of Elderly People Applying for Financial Assistance in the Outskirts of Nanjing. Nursing Research 2017;49:4642.
- Yang L, Kuang X, Su A. Research progress on disability of the elderly and its assessment tools. Nursing Research 2019;33:1722-6.
- Hickey GL, Dunning J, Seifert B, et al. Statistical and data reporting guidelines for the European Journal of Cardio-Thoracic Surgery and the Interactive CardioVascular and Thoracic Surgery. Eur J Cardiothorac Surg 2015;48:180-93. [Crossref] [PubMed]
- Qin N, Yan E. Common Crime and Domestic Violence Victimization of Older Chinese in Urban China: The Prevalence and Its Impact on Mental Health and Constrained Behavior. J Interpers Violence 2018;33:889-914. [Crossref] [PubMed]
- Wu C, Smit E, Xue QL, et al. Prevalence and Correlates of Frailty Among Community-Dwelling Chinese Older Adults: The China Health and Retirement Longitudinal Study. J Gerontol A Biol Sci Med Sci 2017;73:102-8. [Crossref] [PubMed]
- Chen R, Xu P, Li F, et al. Internal migration and regional differences of population aging: An empirical study of 287 cities in China. Biosci Trends 2018;12:132-41. [Crossref] [PubMed]
- Yang M, Lu J, Hao Q, et al. Does residing in urban or rural areas affect the incidence of polypharmacy among older adults in western China? Arch Gerontol Geriatr 2015;60:328-33. [Crossref] [PubMed]
- Dong X, Simon MA. Urban and rural variations in the characteristics associated with elder mistreatment in a community-dwelling Chinese population. J Elder Abuse Negl 2013;25:97-125. [Crossref] [PubMed]
- Norstrand JA, Xu Q. Social capital and health outcomes among older adults in China: the urban-rural dimension. Gerontologist 2012;52:325-34. [Crossref] [PubMed]
- Zhao A, Wang MC, Szeto IM, et al. Gastrointestinal discomforts and dietary intake in Chinese urban elders: a cross-sectional study in eight cities of China. World J Gastroenterol 2019;25:6681-92. [Crossref] [PubMed]
- Dai B. The old age health security in rural China: where to go? Int J Equity Health 2015;14:119. [Crossref] [PubMed]
- Long Y, Li LW. "How Would We Deserve Better?" Rural-Urban Dichotomy in Health Seeking for the Chronically Ill Elderly in China. Qual Health Res 2016;26:1689-704. [Crossref] [PubMed]
- Hu S, Tan H, Peng A, et al. Disparity of anemia prevalence and associated factors among rural to urban migrant and the local children under two years old: a population based cross-sectional study in Pinghu, China. BMC Public Health 2014;14:601. [Crossref] [PubMed]
- Wang D, Li S, Hu M. Negative academic emotion and psychological well-being in chinese rural-to-urban migrant adolescents: examining the moderating role of cognitive reappraisal. Front Psychol 2017;8:1312. [Crossref] [PubMed]
- Dong X, Simon MA, Gorbien M. Elder abuse and neglect in an urban chinese population. J Elder Abuse Negl 2007;19:79-96. [Crossref] [PubMed]
- Xie F, Xie L, Li X, et al. Prevalence and risk factors of hypertension combined with diabetes in middle and elder population in Nan'an district of Chongqing. Zhonghua Liu Xing Bing Xue Za Zhi 2019;40:666-9. [PubMed]
- Lin JN, Wang JJ. Psychometric evaluation of the Chinese version of the Cornell Scale for Depression in Dementia. J Nurs Res 2008;16:202-10. [Crossref] [PubMed]
- Wang F, Meng LR, Zhang Q, et al. Elder abuse and its impact on quality of life in nursing homes in China. Arch Gerontol Geriatr 2018;78:155-9. [Crossref] [PubMed]
- Zhou J, Hearst N. Health-related quality of life of among elders in rural China: the effect of widowhood. Qual Life Res 2016;25:3087-95. [Crossref] [PubMed]
- Liu H, Han X, Xiao Q, et al. Family structure and quality of life of elders in rural China: the role of the new rural social pension. J Aging Soc Policy 2015;27:123-38. [Crossref] [PubMed]
- Shao R, Hu T, Zhong YS, et al. Socio-demographic factors, dental status and health-related behaviors associated with geriatric oral health-related quality of life in Southwestern China. Health Qual Life Outcomes 2018;16:98. [Crossref] [PubMed]
- Wang M, He B, Wang Y, et al. Depression among Low-Income Female Muslim Uyghur and Kazakh Informal Caregivers of Disabled Elders in Far Western China: Influence on the Caregivers' Burden and the Disabled Elders' Quality of Life. PLoS One 2016;11:e0156382. [Crossref] [PubMed]
- Liu X, Lu B, Feng Z. Intergenerational transfers and informal care for disabled elderly persons in China: evidence from CHARLS. Health Soc Care Community 2017;25:1364-74. [Crossref] [PubMed]
- Li LW, Liu J, Zhang Z, et al. Late-life depression in Rural China: do village infrastructure and availability of community resources matter? Int J Geriatr Psychiatry 2015;30:729-36. [Crossref] [PubMed]
- Cao MJ, Guo XL, Yu H, et al. Chinese community-dwelling elders' needs: promoting ageing in place. Int Nurs Rev 2014;61:327-35. [Crossref] [PubMed]
- Lu S, Wu Y, Mao Z, et al. Association of formal and informal social support with health-related quality of life among Chinese rural elders. Int J Environ Res Public Health 2020;17:1351. [Crossref] [PubMed]
- Lin CC, Li CI, Chang CK, et al. Reduced health-related quality of life in elders with frailty: a cross-sectional study of community-dwelling elders in Taiwan. PLoS One 2011;6:e21841. [Crossref] [PubMed]
- Wan KY, McMillan AS, Wong MC. Orofacial pain symptoms and associated disability and psychosocial impact in community-dwelling and institutionalized elderly in Hong Kong. Community Dent Health 2012;29:110-6. [PubMed]
- Zeng Y, Li J, Yuan Z, et al. The effect of China's new cooperative medical scheme on health expenditures among the rural elderly. Int J Equity Health 2019;18:27. [Crossref] [PubMed]
- Li W, Wang D, Gan Y, et al. Factors influencing government insurance scheme beneficiary acceptance of the gatekeeper policy: a cross-sectional study in Wuhan, China. BMC Health Serv Res 2018;18:241. [Crossref] [PubMed]
- Dai BZ, Zhou LL, Mei YJ. Old age security in rural China: there is a long way to go. Chin Med J 2013;126:4348-53. [PubMed]
- Qin S, Ding Y. Why not see a doctor when ill? Evidence from the Chinese elderly. BMC Health Serv Res 2019;19:365. [Crossref] [PubMed]


