Goal attainments and their discrepancies for low density lipoprotein cholesterol (LDL-C) and apolipoprotein B (apo B) in over 2,000 Chinese patients with known coronary artery disease or type 2 diabetes
Introduction
Cardiovascular diseases due to atherosclerosis of the arterial vessel wall and to thrombosis are the foremost cause of premature mortality and of disability-adjusted life years in the developed countries and are also increasingly common ones in developing countries (1). It is acknowledged that patients with diabetes mellitus (DM) are susceptible to coronary artery disease (CAD) and that the coexistence of both diseases is common in clinical practice. According to recently published guidelines, persons with established CAD or CAD risk equivalents, such as DM, are categorized into high risk and need similarly active management of dyslipidemia (2). Thus, it’s reasonable these 2 diseases are put together under investigation. Lipid metabolism can be disturbed in different ways, leading to changes in plasma lipoprotein function and/or levels. This by itself and through interaction with other cardiovascular risk factors may affect the development of atherosclerosis. The lipid evaluation includes total cholesterol (TC), triglycerides (TG), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), apolipoprotein B (apo B), apolipoprotein (apo A1) and lipoprotein (a) [Lp(a)], among which LDL-C is acknowledged as the primary target of therapy on one hand. On the other hand, the apo B, the number of the atherogenic apo B lipoprotein particles, has been emerging as a more accurate biomarker for cardiovascular risk prediction compared with the traditional LDL-C. The superiority of apo B over LDL-C has been confirmed by several large clinical studies (3-5) and Meta analyses (6). Given the importance of LDL-C and apo B, little is known, however, about LDL-C and apo B goal attainments and their discrepancies in Chinese patients with known CAD or DM on stable therapy for at least 3 months. Moreover, as of the present time, there has been no relatively large-scale sample study to compare the both goal attainments in Chinese patients with known CAD or DM.
Methods
Patients
A total of 2,172 hospitalized patients aged >27 years of old were enrolled from Jan. 1st 2009 to Dec. 31st 2012. They had been on stable therapy for CAD or type 2 DM for at least 3 months.
Lipid profile measure and definitions
A venous blood sample was drawn after fasting 8 h and all samples were analyzed in a central laboratory for TC, HDL-C, LDL-C, TG, apo B, apo A1, Lp(a), and blood sugar. The TC, TG, HDL-C and LDL-C concentrations were determined directly by the colorimetry according to the enzymatic principle. The apo B concentrations were determined directly by the immuno-turbidimeters. The related reagents were purchased from Sekisui Medical CO., LTD. CAD diagnosis with coronary artery diameter stenosis of ≥50% was confirmed by coronary angiogram. DM diagnosis was based on fasting glucose ≥7.0 mmol/L recommended by American Diabetes Association (7) or on patients’ histories of hypoglycemic therapy. Primary hypertension was diagnosed based on the blood pressure ≥140/90 mmHg or on patients’ histories of antihypertensive therapy.
Interventions and designs
This is an observational study for hospitalized patients, who were on stable therapy for at least 3 months. These patients were divided into four groups: all patients, including CAD or DM, but not excluding any other diagnoses; CAD alone, excluding DM, but perhaps including any other diagnoses; DM alone, excluding CAD, but perhaps including any other diagnoses; the coexistence of CAD and DM, but not excluding any other diagnoses. Stable therapy meant standard care of aspirin, β-blockers, angiotensin converting enzyme inhibitor, clopidogrel and statins for CAD patients and all kinds of hypoglycemics for DM ones, and also included appropriate drug adjustments for CAD or DM at the discretion of physicians.
Primary endpoint
According to the ESC/EAS guidelines for the management of dyslipidemia (1), documented CAD or DM has been stratified into very high risk, and the treatment target for LDL-C is <1.8 mmol/L and for apo B <0.8 g/L, respectively.
For this study, the primary endpoint was success rate, defined as the proportion of patients achieving apo B treatment goal according to the ESC/EAS guideline (1). The apo B goal attainment are <0.8 g/L for very high risk patients. The apo B goal attainment was evaluated for all patients included, for varying categorizations and for different sexes. The percentages of patients who were not at their LDL-C goals, but at their apo B goals were also determined. The apo B goals were compared across varying categorizations and genders.
Statistical analysis
Continuous variables are expressed as median (25th-75th percentile) as all of these variables are not distributed normally. Categorical variables are expressed as percentages. Independent samples of continuous variables or categorical variables across the groups were compared by Kruskal-Wallis equality-of-populations rank test or by Pearson χ2. A 2-tailed P value <0.05 was considered statistically significant. The statistical analyses were completed using STATA 12.0 software.
Results
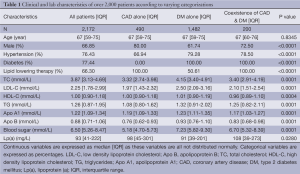
Clinical and lab characteristics of over 2,000 patients
Table 1 shows the clinical and laboratory characteristics of the 2,172 patients included according to varying categorizations. The male patients were dominant across all categorizations. The percentages of hypertension were high across all categorizations, among which the highest percentage (79.28%) was found in DM alone patients, and the lowest percentage was found in CAD alone patients, but also reaching up to 66.94%. Overall, 59.78% of men received lipid lowing therapy as compared with 48.06% of women, with the difference being 10 percentage points in all patients (P<0.0001). The same trends toward to higher proportion of lipid lowing therapy in men than in women have been found across categorizations although only in DM alone was the statistical difference found (P<0.0001).
Full table
LDL-C and apo-B goal attainments by categorization and by sex
Overall, 26.15% and 37.80% of patients attained LDL-C and apo-B goals, respectively. When the success rates of LDL-C and apo B were evaluated by categorization, the success rates were lowest (18.29% and 30.70%, respectively) in DM alone patients as compared with CAD alone patients (44.29% and 55.71%, respectively) or with coexistence of CAD and DM patients (40.00% and 46.50%, respectively) (between-group comparisons, P<0.0001). The trend toward to higher success rates for LDL-C and apo B in men than in women has been found across all categorizations although only in all patients and in DM alone were the statistically significant differences found (P<0.0001). See Table 2.
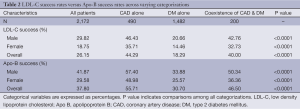
Full table
Interestingly, when the success rates for apo B were compared with the ones for LDL-C, the apo B goal attainment rates were higher than the LDL-C’s across all categorizations, with the statistically significant differences seen in all patients, CAD alone and DM alone (P=0.000), but not in coexistence of CAD and DM (P=0.190). The trend toward to higher success rates for LDL-C and apo B goal attainments in men than in women are marked across all categorizations although only in all patients and in DM alone patients were the statistically significant differences found (P<0.01).
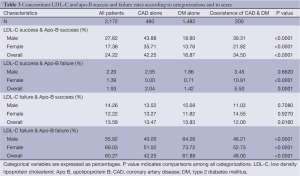
The rates of concomitant LDL-C and apo-B success and failure according to categorizations
Table 3 shows the rates of concomitant LDL-C and apo B success and failure according to categorizations. The highest rates of failure in attaining both goals simultaneously were found in DM alone patients (P<0.0001). On the contrary, the success rates of both goals were highest in CAD alone patients (P<0.0001). Strikingly, 13.58%, 13.47%, 13.83% and 12.00% of patients who failed to attain LDL-C goal attained apo B goal in CAD alone, DM alone, and coexistence of CAD and DM, respectively. Conversely, 1.93%, 2.04%, 1.42% and 5.50% of patients who failed to attain apo B goal attained LDL-C goal in all patients, in CAD alone, DM alone, and coexistence of CAD and DM, respectively.
Full table
Discussion
The most important finding of the current study is the significant differences for apo B and LDL-C goal attainments, with the former being higher than the latter in Chinese patients with known CAD or DM. This finding is particularly striking, we think, in the context that apo B appears to be a more accurate marker of cardiovascular risk prediction than LDL-C. Overall, the success rates for apo B goal attainments are 10 percentage points higher than those for LDL-C’s. This phenomenon can be found across all categorizations. Also, the success rates for apo B goal attainments are 10 percentage points higher for LDL-C’s in men than in women across all categorizations. A study from South Korea has revealed that apo B precedes LDL-C in goal attaining after 6 weeks’ treatment of rosuvastatin or atorvastatin in patients with metabolic syndrome and hypercholesterolemia (8). In that study, the mean value of apo B is 0.71 and 0.78 g/L (all <0.8 g/L) in rosuvastatin group and in atorvastatin group, respectively, while the mean value of LDL-C is 2.19 and 2.55 mmol/L (all >1.8 mmol/L) in rosuvastatin group and in atorvastatin group, respectively (8). Another study from Japan, including 39 patients with abnormal glucose tolerance and CAD, has showed similar findings. The mean value of apo B is 0.73 g/L, which is below the cut-off of 0.8 g/L after the combination therapy of ezetimibe and atorvastatin, while the mean value of LDL-C is 2.14 mmol/L, which is above the cut-off of 1.8 mmol/L after the same combination therapy (9). On the contrary, a large sample study from the Western world has revealed that apo B lags behind LDL-C in goal attainments after 6 weeks’ of simvastatin/ezetimibe or atorvastatin therapy in patients with hypercholesterolemia and metabolic syndrome. The mean value of LDL-C is below the cut-off of 1.8 mmol/L while the mean value of apo B remains above the cut-off of 0.8 g/L (10). Ballantyne et al. studied the effect of ezetimibe/simvastatin vs. atorvastatin or rosuvastatin on modifying lipid profiles in patients with diabetes or metabolic syndrome and found that the both mean values of LDL-C and apo B failed to attain the goal levels of 1.8 mmol/L and 0.8 g/L, respectively (11). A Meta-analysis, including 27 randomized clinical trials, confirmed the lower goal attainment for apo B than for LDL-C in hyperlipideamic patients in Western countries (12). Very few literatures are available to report apo B and LDL-C measurements simultaneously in East Asia and, thus, to provide the limited information about their goal attainments. The above-mentioned 2 studies (8,9) from East Asia are small-sampled and underrepresented. However, the conclusion that apo B precedes LDL-C in goal attainment in East Asian appears to be confirmative if we take into account the current study, which includes over 2,000 Chinese patients. The differences for apo B and LDL-C goal attainments between the East Asia and the Western countries perhaps implicate the established occurrence differences for CADs and for stroke between the East Asia and the Western countries (13,14) given that apo B is superior over LDL-C for CAD prediction but not for stroke (15).
Previous studies have confirmed the comparative decrease in the cardiovascular events for women and for men with the statin therapy (16,17).The sex-related differences, however, were noteworthy in apo B and LDL-C attainments and in lipid lowing therapy across all categorizations. Male patients dominated over female ones in incident CAD and DM. The reasonable explanation for the sex-related differences in apo B and LDL-C attainments seems to be the higher rates of lipid lowing therapy in men than in women in the current study. The higher rates for apo B and LDL-C goal attainments and for lipid lowing therapy in men than in women indicated the presence of care gaps reported in the literatures (18,19) and an opportunity to improve clinical cardiovascular outcomes for women.
In conclusions, this is the first large sample study to compare the apo B and LDL-C goal attainments in Chinese patients with known CAD or DM. The current study has revealed the discrepancies of apo B and LDL-C in goal attainments on stable statin therapy for at least 3 months. Whether the discrepancies are associated with the occurrence differences for CAD and for stroke between the East Asia and the Western countries warrants further study.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Catapano AL, Reiner Z, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis 2011;217:3-46. [PubMed]
- Cheng AY, Leiter LA. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Curr Opin Cardiol 2006;21:400-4. [PubMed]
- Holewijn S, den Heijer M, Swinkels DW, et al. Apolipoprotein B, non-HDL cholesterol and LDL cholesterol for identifying individuals at increased cardiovascular risk. J Intern Med 2010;268:567-77. [PubMed]
- McQueen MJ, Hawken S, Wang X, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet 2008;372:224-33. [PubMed]
- Chien KL, Hsu HC, Su TC, et al. Apolipoprotein B and non-high density lipoprotein cholesterol and the risk of coronary heart disease in Chinese. J Lipid Res 2007;48:2499-505. [PubMed]
- Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 2011;4:337-45. [PubMed]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2013;36:S67-74. [PubMed]
- Park JS, Kim YJ, Choi JY, et al. Comparative study of low doses of rosuvastatin and atorvastatin on lipid and glycemic control in patients with metabolic syndrome and hypercholesterolemia. Korean J Intern Med 2010;25:27-35. [PubMed]
- Uemura Y, Watarai M, Ishii H, et al. Atorvastatin 10 mg plus ezetimibe 10mg compared with atorvastatin 20 mg: impact on the lipid profile in Japanese patients with abnormal glucose tolerance and coronary artery disease. J Cardiol 2012;59:50-6. [PubMed]
- Robinson JG, Ballantyne CM, Grundy SM, et al. Lipid-altering efficacy and safety of ezetimibe/simvastatin versus atorvastatin in patients with hypercholesterolemia and the metabolic syndrome (from the VYMET study). Am J Cardiol 2009;103:1694-702. [PubMed]
- Ballantyne CM, Blazing MA, King TR, et al. Efficacy and safety of ezetimibe co-administered with simvastatin compared with atorvastatin in adults with hypercholesterolemia. Am J Cardiol 2004;93:1487-94. [PubMed]
- Abramson BL, Benlian P, Hanson ME, et al. Response by sex to statin plus ezetimibe or statin monotherapy: a pooled analysis of 22,231 hyperlipidemic patients. Lipids Health Dis 2011;10:146. [PubMed]
- Zhao D, Liu J, Wang W, et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing Project. Stroke 2008;39:1668-74. [PubMed]
- Moran A, Gu D, Zhao D, et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes 2010;3:243-52. [PubMed]
- Robinson JG, Wang S, Jacobson TA. Meta-analysis of comparison of effectiveness of lowering apolipoprotein B versus low-density lipoprotein cholesterol and nonhigh-density lipoprotein cholesterol for cardiovascular risk reduction in randomized trials. Am J Cardiol 2012;110:1468-76. [PubMed]
- Waters DD, LaRosa JC, Barter P, et al. Effects of high-dose atorvastatin on cerebrovascular events in patients with stable coronary disease in the TNT (treating to new targets) study. J Am Coll Cardiol 2006;48:1793-9. [PubMed]
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002;360:7-22. [PubMed]
- Wenger NK. Lipid abnormalities in women: data for risk, data for management. Cardiol Rev 2006;14:276-80. [PubMed]
- Kim C, Hofer TP, Kerr EA. Review of evidence and explanations for suboptimal screening and treatment of dyslipidemia in women. A conceptual model. J Gen Intern Med 2003;18:854-63. [PubMed]


