Improved non-calcified plaque delineation on coronary CT angiography by sonogram-affirmed iterative reconstruction with different filter strength and relationship with BMI
Introduction
Recently introduced iterative reconstruction (IR) technique has shown to improve image quality and reduce radiation dose at coronary computed tomography angiography (CCTA) compared with the standard filtered back projection (FBP) (1-4). However, concerns were raised that image quality improvement encountered texture changes due to noise reduction which may affect diagnostic confidence (5). The new generation IR method, which not only worked with basic image correction, but also re-projected in the raw data space, yields higher contrast-to-noise ratio (CNR) and better image quality than FBP in CCTA (6-8). But these studies did not identify the optimal reconstruction kernel among different IR filter strength. Vendors provide different strength scales (e.g., IR-2, 3, and 4). Further, the diagnostic and clinical benefit has not been fully established. The detection of non-calcified plaque with CCTA is still a challenge using FBP, mainly due to difficulties in delineation of the outer plaque boundary, which is influenced by computed tomography (CT) image noise (9,10). Non-calcifying plaque detection is of importance in clinical practice for coronary risk estimation and patient management. Non-calcifying fibroathermoma may indicate culprit lesions for acute coronary syndromes (11), and total plaque burden predicts outcome (12).
The diagnostic benefits of IR for patients and clinical applications in CCTA have not been defined yet. Obese patients with high body mass index (BMI) might benefit more from IR than normal patients.
Therefore, the aim of this study was to prospectively compare non-calcified plaque delineation and image quality of CCTA obtained with sinogram-affirmed IR with different filter strengths and FBP, and to correlate with BMI.
Materials and methods
Study population
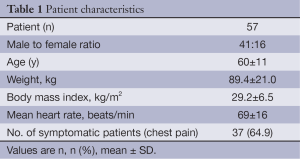
This prospective study included 57 consecutive patients who were referred for the assessment of known or suspected coronary artery disease (CAD) by CCTA according to clinical indications. Exclusion criteria were contraindications to contrast agent, pregnancy, clinical instability and renal insufficiency.
CCTA image acquisition protocol
All CCTA examinations were performed on a second generation 128-slice dual source computed tomography (DSCT) system (SOMATOM Definition FLASH, Siemens Healthcare, Forcheim, Germany). Beta blockers were given in all patients, in whom no contraindications were present, and in whom heart rate (HR) was >60 bpm. The CCTA protocol was determined on patients’ HR and rhythm, BMI, and needed for cardiac functional analysis and meanwhile to minimize the radiation exposure as follows [1= high pitch (3.4 pitch) if HR <58; prospective ECG-triggering if HR regular and <65 bpm; and 2= retrospective ECG-gating if HR >65 bpm and/or irregular]. CCTA images were acquired in cranio-caudal direction from above the ostium of the coronary arteries to below the dome of diaphragm. Acquisition parameters were 2×128×0.6 mm detector collimation, 280 ms gantry rotation time. Tube potential (range, 80-140 kV) and tube current (300-450 mA) were chosen based upon individual patient BMI by experienced technicians. In patients with high BMI, mAs were adjusted upwards. A range of 80-140 mL of iodinated contrast agent (Ultravist 370 mgI/mL, Bayer, Berlin, Germany) with injection velocity of 4.5-6 mL/s was injected through antecubital artery adjusted individually to body size and scan length. FBP reconstruction with kernel of B26f, sonogram-affirmed IR (SAFIRE, Siemens, Germany) with different kernel (IR-2, IR-3 and IR-4) was performed with a section thickness of 0.75 mm in 0.4-mm increments respectively.
Image analysis
All the four reconstructions were transferred to a dedicated 3-D image processing workstation. To assess the overall examination image quality and non-calcified plaque image quality, both subjective and objective parameters were evaluated. Window and level settings were permitted to adjust individually for each study.
Objective overall examination image quality analysis
To obtain objective parameters of image quality, the CT attenuation in Hounsfield Units (HU) and noise (standard deviation, SD) of CT value was measured by manually prescribing circular region of interest (ROI) at consistent slice of image within the aortic root, left main (LM) coronary artery and proximal segment of right coronary artery (RCA) in FBP, IR-2, IR-3 and IR-4 reconstructed images respectively. Calcification or plaque within artery wall was carefully avoided during ROI placement. For each patient, the CNR was calculated with the following formula: CNR = contrast enchantment/image noise.
Subjective overall examination image quality analysis
The overall image quality of FBP, IR-2, IR-3 and IR-4 reconstructions were evaluated by using a 5-point scale according to the severity of image noise, quality of contour delineation, and general image impression: 1= poor; 2= fair; 3= moderate; 4= good; 5= excellent.
Non-calcified plaque image analysis
First, co-registration of the detected non-calcified plaques of all four reconstruction images were performed on multiplanar reformations perpendicular and parallel to the vessel centerline in one-millimeter intervals. The coronary ostia and fiducial markers (side branches, bifurcations and vessel wall morphological features) were used to co-register the plaques. Coronary arteries were divided into 17 segments according to the modified American Heart Association classification in order to record the location of plaque (13).
To obtain subjective evaluation of the non-calcified plaque, a dedicated plaque outer border delineation score was used and graded on a 5-point scale: 1= poor (almost no delineation, very poor diagnostic confidence); 2= fair (possible detection, difficult visualization due to artifacts or weak display); 3= moderate (moderate diagnostic confidence); 4= good (good confidence, minor image quality limitations); 5= excellent (perfect visualization, high diagnostic confidence) Then, to obtain the objective parameters of plaque, circular ROI (as large as possible without including parts of the coronary vessel wall) were drawn on all of these plaques in the four reconstruction images. Areas of prominent artifacts, if any, were carefully avoided. The mean CT attenuation (HU = Hounsfield Units) and image noise (SD = standard deviation of HU) were measured on these plaques, the CNR were calculated using the same formula as above. One experienced reader with 5 years of cardiac CT experience performed the analysis. A second reader with a higher level of experience (10 years) performed the same evaluations.
Statistical analysis
Results were expressed as means ± SD for continuous variables and frequencies with percentages for categorical variables. One on one comparison of CNR and noise between the four reconstructions were conducted using one-way analysis of variance (ANOVA) and multiple comparisons by least significant difference (LSD). A Kruskal-Wallis test was used for non-normally distributed data. The overall examination image quality and non-calcified plaque delineation score were also grouped and compared in different BMI stratification. Statistical analysis was made using IBM SPSS Statistics 20 software. P<0.05 was considered statistically significant. Interobserver variability was calculated using kappa-statistics.
Results
A total of 57 CCTA studies were included. Four of these patients had history of coronary artery bypass grafts. Demographic data of patients are shown in Table 1. The average BMI in our patient was 29.2 kg/m2 (range, 20.0-59.0 kg/m2).
Full table
Assessment of overall examination image quality
A total of 71.9% (41/57) patients were reconstructed with FBP, 96.5% (55/57) with I2f, 96.5% (55/57) with I3f and 98.2% (56/57) applying I4f who had overall CCTA image quality score ≥3.
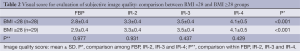
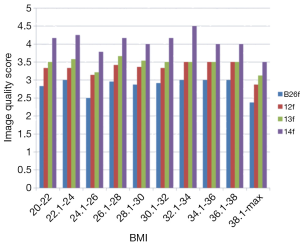
There were statistical differences in CCTA exam image quality score among the 4 image reconstructions (FBP: 2.9±0.4, IR-2: 3.3±0.4, IR-3: 3.5±0.4, IR-4: 4.1±0.4, P<0.001). When splitting the patients into BMI <28 and BMI ≥28 groups, there were no significant differences between the two groups compared within the same IR- reconstruction, but significant differences between the two groups compared among different IR-filter strength and reconstruction methods (FBP vs. IR) (Table 2), IR-4 reveals the highest score in both BMI <28 and BMI ≥28 groups. In the BMI <28 group, compared with FBP, the average image quality score increased by 17.9% for IR-2, by 25% for IR-3, and 46.4% for IR-4. In BMI ≥28 groups, as compared with FBP, the average image quality score increased by 13.8% for IR-2, by 20.7% for IR-3, and 41.4% for IR-4. When patients were stratified into different BMI subgroups, the changes of image quality score among the four reconstructions are shown in Figure 1.
Full table
For the objective image quality parameters, there were significant differences in image noise among the 4 reconstructions at different position (Table 3). When comparing among groups, there were significant differences between FBP, IR-2, IR-3 and IR-4 (P=0.000-0.03) except between IR-2 and IR-3 (P=0.062), between IR-3 and IR-4 (P=0.061) in LM segment, and between IR-3 and IR-4 (P=0.079) in RCA proximal segment. IR-4 always showed the lowest image noise.
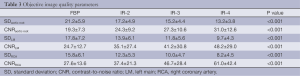
Full table
There were significant differences in CNR among the 4 image reconstruction groups at different position (Table 3). There were significant differences between different reconstructions (P=0.000-0.035) except between IR-2 and IR-3 (P=0.122), between IR-3 and IR-4 (P=0.05) in aortic root level, between IR-2 and IR-3 (P=0.213), between IR-3 and IR-4 (P=0.156) in LM segment, and between FBP and IR-2 (P=0.069), between IR-2 and IR-3 (P=0.089) in RCA proximal segment. IR-4 always showed the highest CNR.
When splitting patients into BMI <28 and BMI ≥28 groups, there were no significant differences in image noise within the same reconstruction (P=0.083-0.737), but significant differences in CNR between the two BMI groups compared within the same reconstruction (P=0.000-0.048) were found (except for IR-2, IR-3 and IR-4 at LM level). CNR in BMI <28 group was higher than BMI >28 group.
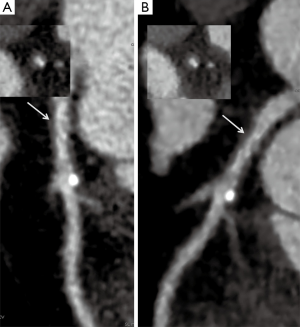
Delineation and image quality of non-calcified plaque
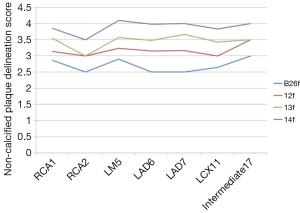
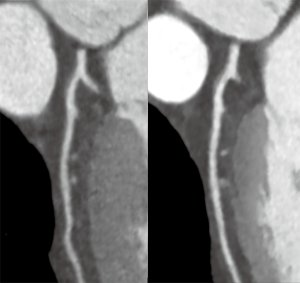
There were 61 non-calcified plaques in 57 patients (RCA1=11, RCA2=1, LM5=15, LAD6=23, LAD7=3, LCX11=7, Intermediate17=1). All of the 61 plaques (100%) were detected by IR reconstructions, out of those 11 (18.0%) plaques were missed by FBP in the first evaluation due to worse image noise or small lesion size (BMI >28: 9 patients, small size lesion: 1 patient, low BMI with low voltage setting: 1 patient). There were statistical differences in non-calcified plaque delineation score among the 4 image reconstructions, with increasing scores with increasing IR- filter strength (FBP: 2.7±0.4, IR-2: 3.2±0.3, IR-3: 3.5±0.3, IR-4: 4.0±0.4, P<0.001) (Figure 2).
When patients were split into BMI <28 and BMI ≥28 groups, there were no significant differences of non-calcified plaque delineation score between the two groups compared within the same reconstruction, but significant differences between the two groups compared among differences reconstruction methods (Table 4). I4f revealed the highest score in both BMI <28 and BMI ≥28 groups. Notably, for IR-4, the average delineation score in BMI ≥28 group was 4.0±0.4, even higher than BMI <28 group (3.9±0.3). In the BMI <28 group, compared with FBP, the average plaque delineation score increased by 14.3% for IR-2, by 25.0% for IR-3, and by 39.3% for IR-4 group. In BMI ≥28 groups, as compared with FBP, the average plaque delineation score increased by 19.2% when applying IR-2, by 34.6% for IR-3, and by 53.8% for IR-4 filter. The average plaque delineation scores in different segments are presented in Figure 3.
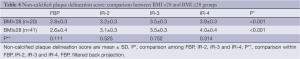
Full table
For the objective plaque delineation parameters, there were significant differences in image noise and CNR among the 4 reconstructions (Table 5). When patients were split into BMI <28 and BMI ≥28 groups, there no significant differences of image noise and CNR of non-calcified plaques between the two groups compared within the same reconstruction (image noise: P=0.401-0.788; CNR: P=0.252-0.975), but significant differences in image noise (BMI <28: P<0.001, BMI ≥28: P<0.001) and CNR (BMI <28: P=0.001, BMI ≥28: P<0.001) between the two groups among the 4 reconstructions were observed. IR-4 revealed the lowest image noise and highest CNR both in low and high BMI groups. The 140 kV tube setting for extremely obese patients was required in 9/57 patients (15.7%).
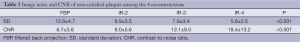
Full table
Interobserver variability was kappa 0.89 for non-calcifying plaque detection.
Discussion
To the best of our knowledge, this is the first report investigating non-calcified plaque delineation and image quality of CCTA obtained with sonogram-affirmed IR with different filter strengths, in relation to BMI. We included patients with high (>28 BMI) as well as excessively high BMI (>35). The major finding of our study is that IR offers improved non-calcifying plaque delineation and image quality as compared with FBP, especially if BMI is increasing. Importantly, 18% of non-calcifying plaques were missed with FBP initially but detected by IR. IR-4 shows the best objective and subjective image related parameters of overall examination and plaque delineation among the different IR filter strength. IR in combination with low—radiation dose techniques such as prospective ECG-triggered or high—pitch CT, helps to provide high quality CCTA images in obese patients with low radiation (14).
In line with other studies (6-8,15), our results revealed that compared with images obtained by standard FBP, IR led to significant improvement of CCTA examination image quality through reduction in the image noise.
Furthermore, we demonstrated that the IR-4 is the best filter strength in order to optimize image quality, due to its highest “smoothing” capability (= noise reduction). Compared with the low BMI group, image quality did not deteriorate and the image noise did not increase in the high BMI group when applying IR. Therefore, IR can be used in the obese patients in order to maintain image quality and to keep the diagnostic confidence high. Studies (1,5) which used prior generation IR suggested that IR alters image appearance, resulting in artificial over-smoothing of the images compared to FBP reconstructions. Studies (6-8,16) that used the new generation IR, which worked both on image-based and raw-data-based domain, suggested that the noise reduction did not come at the cost of spatial resolution impairments affecting image texture. Our results are in line with these findings.
Studies between CCTA and intravascular ultrasound (IVUS) have shown that partially calcified and calcified plaques can be accurately detected by CCTA, whereas non-calcified plaque volume is often underestimated (17,18). A potential explanation is that high image noise “masks” partly the non-calcifying plaque volume. Image noise is reduced when using IR, which critical in multi-slice CT because image noise is directly related to the ability to depict low-contrast lesions, and thus highly relevant clinical CT imaging (19). Vulnerable plaque characteristics are associated with the occurrence of acute coronary syndrome, especially in the presence of positive remodeling and low density plaques (20-22). Therefore, improving the non-calcified plaque detection is crucial for an individual’s risk stratification for further coronary events, such as the DUKE-score or the segment involvement score (SIS). In our study, compared with IR, there were 11 (18.0%) plaques was missed by FBP, which suggested that IR is helpful for improving non-calcified plaque detection in CCTA by decreasing image noise. Our results showed that compared with FBP, the performance of IR is better both in objective and subjective plaque delineation parameters, and IR-4 always reveals the best performances among them (Figure 4). Furthermore, the non-calcifying plaque delineation score, image noise and CNR in the high BMI group are consistent with low BMI group within the same reconstruction, and even average plaque delineation score of high BMI group is higher than that of low BMI group in IR-4. The improvement in plaque delineation was more obviously in obese patients. In addition, no significant effect of the lesion size on the plaque visualization when using IR was found (23). Plaques in proximal segments were prone to have higher delineation score in our study, this is partially in line with the study that demonstrating that the ability of plaque detection is related to their size (22).
In our study, interobserver variability for non-calcifying plaques was good, which is attributed to the high level of cardiac CT experience of both readers, which may not apply for less experienced readers. Further, our plaques were homogenous non-calcifying, while a variation in observer agreement among different among plaque types (with K =0.48, K =0.42, and K =1.00 for non-versus mixed versus calcifying plaques, resp.), has been shown (24). A low variability however has been demonstrated previously in another study (25).
Study limitations
Our study was designed to assess improvements in image quality and delineation of non-calcified plaque garnered by the use of IR over FBP in patients with non-calcified plaques, especially in obese patients. We did not calculate radiation dose, because multiple previous studies have already shown a high potential of IR for radiation dose reduction while a decrease in image noise was observed (1,2,4,5). Further, we did not lower mAs as low as possible to obtain a ultra-low radiation dose because the aim of our study was to compare the different IR-reconstruction modules while keeping mAs and aiming optimal image quality with a reasonable radiation dose for the patients in our institution, which has been reported as 4.7 mSv ±5 (1.07 mSv ±0.2 for high-pitch; 4.2 mSv ±2.4 for sequential and 11.1 mSv ±5 for spiral technique).
We further acknowledge that no correlation with IVUS was performed, which is the gold standard. Next, there may be a slight selection bias towards obese patients with high BMI, in whom 140 kV tube voltage (26) was applied in order to ensure image quality. However, only a few patients (15.7%) received 140 kV.
Finally, we did not calculate plaque volume but we included all plaques (independent from size) in our study order to simulate a real-world scenario, while we acknowledge that the ability to detect plaque is related to their size, and more difficult for smaller lesions.
In summary, our study suggests that IR offers improved image quality and non-calcifying delineation compared with FBP, especially in high BMI patients. IR-4 shows the best objective and subjective image parameter among the different IR strength. Importantly, non-calcifying plaque can be missed on FBF, while IR improves detection rate and image quality. Most recent data from a large international multicenter registry (CONFIRM) indicate that coronary plaque burden is an important predictor of outcome. Non-calcifying plaques are important risk factors for adverse cardiac event (12). Beyond, non-calcifying atheroma is known to be related to culprit lesions causing acute coronary syndrome and predict outcome (11).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Leipsic J, Labounty TM, Heilbron B, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol 2010;195:655-60. [PubMed]
- Gosling O, Loader R, Venables P, et al. A comparison of radiation doses between state-of-the-art multislice CT coronary angiography with iterative reconstruction, multislice CT coronary angiography with standard filtered back-projection and invasive diagnostic coronary angiography. Heart 2010;96:922-6. [PubMed]
- Renker M, Nance JW Jr, Schoepf UJ, et al. Evaluation of heavily calcified vessels with coronary CT angiography: comparison of iterative and filtered back projection image reconstruction. Radiology 2011;260:390-9. [PubMed]
- Ebersberger U, Tricarico F, Schoepf UJ, et al. CT evaluation of coronary artery stents with iterative image reconstruction: improvements in image quality and potential for radiation dose reduction. Eur Radiol 2013;23:125-32. [PubMed]
- Marin D, Nelson RC, Schindera ST, et al. Low-tube-voltage, high-tube-current multidetector abdominal CT: improved image quality and decreased radiation dose with adaptive statistical iterative reconstruction algorithm--initial clinical experience. Radiology 2010;254:145-53. [PubMed]
- Utsunomiya D, Weigold WG, Weissman G, et al. Effect of hybrid iterative reconstruction technique on quantitative and qualitative image analysis at 256-slice prospective gating cardiac CT. Eur Radiol 2012;22:1287-94. [PubMed]
- Chen MY, Steigner ML, Leung SW, et al. Simulated 50% radiation dose reduction in coronary CT angiography using adaptive iterative dose reduction in three-dimensions (AIDR3D). Int J Cardiovasc Imaging 2013;29:1167-75. [PubMed]
- Takx RA, Schoepf UJ, Moscariello A, et al. Coronary CT angiography: comparison of a novel iterative reconstruction with filtered back projection for reconstruction of low-dose CT-Initial experience. Eur J Radiol 2013;82:275-80. [PubMed]
- Leber AW, Knez A, Becker A, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol 2004;43:1241-7. [PubMed]
- Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 2005;46:147-54. [PubMed]
- Dohi T, Mintz GS, McPherson JA, et al. Non-fibroatheroma lesion phenotype and long-term clinical outcomes: a substudy analysis from the PROSPECT study. JACC Cardiovasc Imaging 2013;6:908-16. [PubMed]
- Otaki Y, Arsanjani R, Gransar H, et al. What have we learned from CONFIRM? Prognostic implications from a prospective multicenter international observational cohort study of consecutive patients undergoing coronary computed tomographic angiography. J Nucl Cardiol 2012;19:787-95. [PubMed]
- Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975;51:5-40. [PubMed]
- Wang R, Schoepf UJ, Wu R, et al. Image quality and radiation dose of low dose coronary CT angiography in obese patients: sinogram affirmed iterative reconstruction versus filtered back projection. Eur J Radiol 2012;81:3141-5. [PubMed]
- Eisentopf J, Achenbach S, Ulzheimer S, et al. Low-dose dual-source CT angiography with iterative reconstruction for coronary artery stent evaluation. JACC Cardiovasc Imaging 2013;6:458-65. [PubMed]
- Gramer BM, Muenzel D, Leber V, et al. Impact of iterative reconstruction on CNR and SNR in dynamic myocardial perfusion imaging in an animal model. Eur Radiol 2012;22:2654-61. [PubMed]
- Sun J, Zhang Z, Lu B, et al. Identification and quantification of coronary atherosclerotic plaques: a comparison of 64-MDCT and intravascular ultrasound. AJR Am J Roentgenol 2008;190:748-54. [PubMed]
- Leber AW, Becker A, Knez A, et al. Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am Coll Cardiol 2006;47:672-7. [PubMed]
- von Falck C, Galanski M, Shin HO. Informatics in radiology: sliding-thin-slab averaging for improved depiction of low-contrast lesions with radiation dose savings at thin-section CT. Radiographics 2010;30:317-26. [PubMed]
- Hammer-Hansen S, Kofoed KF, Kelbaek H, et al. Volumetric evaluation of coronary plaque in patients presenting with acute myocardial infarction or stable angina pectoris-a multislice computerized tomography study. Am Heart J 2009;157:481-7. [PubMed]
- Sato A, Ohigashi H, Nozato T, et al. Coronary artery spatial distribution, morphology, and composition of nonculprit coronary plaques by 64-slice computed tomographic angiography in patients with acute myocardial infarction. Am J Cardiol 2010;105:930-5. [PubMed]
- Kitagawa T, Yamamoto H, Horiguchi J, et al. Characterization of noncalcified coronary plaques and identification of culprit lesions in patients with acute coronary syndrome by 64-slice computed tomography. JACC Cardiovasc Imaging 2009;2:153-60. [PubMed]
- von Falck C, Bratanova V, Rodt T, et al. Influence of sinogram affirmed iterative reconstruction of CT data on image noise characteristics and low-contrast detectability: an objective approach. PLoS One 2013;8:e56875. [PubMed]
- van der Giessen AG, Toepker MH, Donelly PM, et al. Reproducibility, accuracy, and predictors of accuracy for the detection of coronary atherosclerotic plaque composition by computed tomography: an ex vivo comparison to intravascular ultrasound. Invest Radiol 2010;45:693-701. [PubMed]
- Stolzmann P, Schlett CL, Maurovich-Horvat P, et al. Variability and accuracy of coronary CT angiography including use of iterative reconstruction algorithms for plaque burden assessment as compared with intravascular ultrasound-an ex vivo study. Eur Radiol 2012;22:2067-75. [PubMed]
- Leschka S, Stinn B, Schmid F, et al. Dual source CT coronary angiography in severely obese patients: trading off temporal resolution and image noise. Invest Radiol 2009;44:720-7. [PubMed]


