Salt reduction in Australia: from advocacy to action
Introduction
In 2013, the Federal Government of Australia signed up to the global targets to reduce population salt (sodium) intake by 30% by 2025. These were part of a broader set of United Nation (UN) nine targets to reduce the burden of non-communicable diseases (NCDs) by 25% by 2025 (1). NCDs, including cardiovascular disease, are the leading cause of death in the world, killing more people each year than all other causes combined (1). Almost 1 in 3 deaths in Australia was due to cardiovascular disease in 2012 (2). Ischemic heart disease was the leading cause of death followed by cerebrovascular diseases (strokes, haemorrhages, infarctions) (3).
There is strong evidence to show that reducing salt intake will reduce blood pressure with subsequent reduction in the number of premature deaths from heart disease and stroke (4). Additionally, population salt reduction has been identified as one of the most cost-effective strategies for reducing the burden of NCDs, both internationally (5) and in Australia (6).
How much salt are we eating?
Whilst there is no nationally representative study of salt intake based on 24-hour urine samples in Australia, most studies suggest that people are eating around 8-9 g each day, almost twice the World Health Organization (WHO) guideline amount (7). As much as 80% of salt in the Australian diet is likely to come from processed foods (8). Recent studies utilising dietary data indicate that around 19% of salt in the diet of both children and adults comes from bread with other main contributors including cereals, meat products, sauces, dairy and egg dishes and combination dishes, for example, pizzas, sandwiches, stir fry dishes (9,10). The average Australian diet derives 35% of daily energy intake from discretionary processed foods which are energy dense, nutrient poor and high in saturated fat, sugar and salt (11). Sources of salt in children’s diets are similar to that of adults (12).
The existing range of salt levels of different brands in similar processed food products found in Australia (13) demonstrates significant potential capacity for reformation of processed food to reduce salt within and between different food categories. One of the advantages of such an approach is that it is possible to reduce the salt content of processed foods to a level that can achieve clinically significant reductions in daily salt intake without adversely impacting customer preference for specific foods (14). But a strong government policy or regulatory approach would be required to achieve this.
The regulatory environment for salt in Australia
Australia has a federal system of government, supplemented by eight state and territory governments, each of which contains multiple local government areas such as cities and shires. All levels of government in Australia have responsibilities for food policy, legislation and regulation. This complexity can be a barrier to nationally coordinated action on food policy, but also provides opportunity for advocacy and action at multiple levels of government. Public health advocates in Australia have commonly used this to encourage evidence-based experimentation in health policy and uptake of best practice across jurisdictions, for example through a high profile National Tobacco Scorecard (15).
The Australian National Healthcare Agreement 2012 (16) sets out the roles of Federal and State and Territory Governments in relation to health and provides a clear remit for State and Territory Governments to act alone or work in partnership with Federal Government on programs related to salt reduction, whether it is through food regulation, health promotion or health research. National food-related public health initiatives are agreed through the Australian Health Ministers’ Advisory Council, through its Australian Population Health Development Principal Committee (APHDPC).
Australia currently has national dietary guidelines for salt and a Food and Health Dialogue (FHD), established in 2010, which has set voluntary salt targets for 11 food categories (17). Analysis of salt reductions against the initial targets has demonstrated positive progress (18). However, additional steps will still be needed to ensure a coherent government response of the magnitude required to ensure that Australia can meet the new global targets. The objective of this paper is to review existing population wide salt reduction activities in Australia with a view to identifying where there is a need for additional action.
Methods
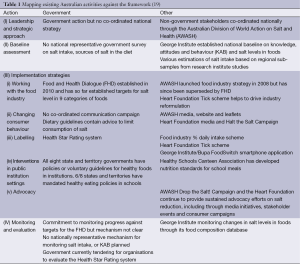
A review of the literature and stakeholder activities was undertaken to provide a comprehensive overview of salt reduction activities in Australia. Peer-reviewed literature and grey literature were retrieved from PubMed, governmental and non-governmental organization websites. Search terms used included salt or sodium and Australia. The literature review and stakeholder information was also supplemented by a questionnaire completed by a representative from the Department of Health. These activities were then assessed against an established framework for salt reduction strategies (19) within the following domains: leadership and strategic approach, baseline assessment, implementation (working with the food industry, changing consumer behaviour, food labelling, interventions in public institution in settings), monitoring and evaluation (Table 1).
Results
Leadership and strategic approach
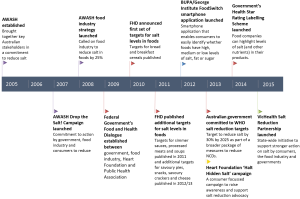
Whilst a range of salt reduction activities currently exist in Australia, there is no co-ordinated national government strategy on salt. In fact, there is a paucity of national policy in relation to public health nutrition in general. A National Food Plan (20) was produced in 2013, and was primarily orientated towards food industry, as opposed to public health, concerns. Similarly, a scoping study for a National Nutrition Policy (21) is in development, but without a publicly-available timeline for delivery. There is currently no obesity strategy in Australia, although a National Diabetes Strategy (22) is in development. Given this lack of national leadership on food policy by government, much of the salt reduction work to date has been led by non-governmental organisations (NGOs), such as the Heart Foundation, and advocacy networks. Since 2005 this has been co-ordinated through the Australian Division of World Action on Salt and Health (AWASH) (Figure 1).
National leadership
Australian Division of World Action on Salt and Health (AWASH)
AWASH was established in 2005, modelled on UK CASH and affiliated with World Action on Salt and Health (WASH). WASH was established in 2005 and is a global group with the mission to improve the health of populations throughout the world by achieving a gradual reduction in salt intake (23). In 2007, AWASH launched its Drop the Salt! Campaign to persuade the government to develop a national salt reduction strategy (8). Hosted by The George Institute for Global Health, the campaign brought together key stakeholders to persuade government to set a population salt reduction target, engage the food industry to reduce salt in foods, support a comprehensive social marketing campaign to change consumer behaviour, introduce clearer labelling of the salt content of foods and commit to regular monitoring of population salt intake. The main strategies of AWASH were government engagement, food industry engagement and media and communications, underpinned by a robust research and monitoring program.
National Heart Foundation of Australia
The National Heart Foundation’s Tick Program has been challenging Australian food companies to reformulate to produce healthier products in specified food categories and highlight them to consumers using the Tick logo since 1989 (24,25). The Heart Foundation continues to be a key player in salt reduction. Its existing 5-year Strategic Plan (26) prioritises salt reduction by pushing for stronger government action on food reformulation and launching a consumer awareness/advocacy campaign (27). The Heart Foundation was instrumental in the establishment of the FHD in 2009 and has continued to play a critical role in its implementation. This has included providing reformulation expertise and nutritional analysis, and profiling of various food categories to support the nutrient target setting process. The Heart Foundation has argued strongly in recent years for a “super-charging” of the FHD (28).
Australian government
Whilst there is no overarching government policy or strategy on salt, the federal government has acknowledged the importance of reducing salt in the diet for several decades (29,30), and currently leads a number of initiatives related to salt reduction. These include the FHD with a remit to drive food reformulation as well as to implement a social marketing strategy to improve healthy eating (31); the Australian Health Survey (AHS), which recently reported on salt intake levels for Australia (32), and recently endorsed a Healthy Star rating labelling scheme to highlight the healthiness of foods on labels on the front of food products (33).
State and territory leadership
VicHealth salt reduction partnership
VicHealth is a statutory health promotion foundation in the State of Victoria which is home to about 6 million people, one quarter of the population of Australia. In recognition of the public health benefits that can be achieved, VicHealth has prioritised the establishment of a State-level partnership to reduce population salt intake. Principal partners include the World Health Organization Collaborating Centre on Population Salt at The George Institute, Deakin University and the National Heart Foundation (Victoria). The strategy and action plan, to be launched in 2015, outlines the intentions to work with governments, the food industry, non-government organisations and the Victorian public, to build a shared commitment to action on salt. This includes initiatives to get more Victorians talking about the current high levels of salt in foods; support for stronger government policy and leadership; work with food industry partners to find innovative solutions to lowering salt in foods and meals, and a program to monitor and evaluate progress made to reduce salt in Victoria.
Baseline assessment
The 2011-2012 AHS is the only nationally representative survey of salt intake in Australia and recently reported that mean population salt intake was about 6 g/day (32). However, this was based on dietary surveys (repeat 24-hour recall) which are known to under-estimate salt intakes and did not include discretionary salt (34). Most studies using 24-hour urine, indicate that salt intake in Australia is 8-9 g/day per person. There are marked regional differences, for example from 7.9 g/day in the city of Adelaide, South Australia (9) to 9 g/day in the market town of Lithgow, New South Wales (35). Most studies also demonstrate significant differences in salt intake between men and women. For example, the most recent Victorian study estimated a daily intake of 9.5 g for men and 6.9 g for women (36). Children are also eating more than the recommendations for adults. The recent AHS showed that almost all children were exceeding recommended upper levels, with intakes ranging from just under 4 g for 2-3 year olds to almost 7 g for 14-18 year olds (32). This is consistent with the salt intake assessed by 24-hour urinary sodium excretion in Victorian school children aged 5 to 13 years (37).
A national baseline for sodium levels in foods and consumer knowledge, attitudes and behaviour (KAB) towards salt was undertaken by The George Institute in 2008 (38,39). Subsequent regional assessments have been conducted (40). There is no agreed national mechanism for monitoring changes in salt intake or KAB. Objective monitoring of the food industry progress on reducing salt in foods is being undertaken via the establishment of a database of sodium levels in foods (13).
Implementation
Working with the food industry
The government’s FHD is now the main vehicle for engaging the food industry to reduce salt levels in processed foods and meals. AWASH previously launched its food industry strategy in 2008 building on the efforts of the successful Heart Foundation Tick program which had been running since 1989 (41). The objective of the AWASH food industry strategy was to engage all sectors of the food industry in a voluntary collaborative effort to reduce salt in all food categories that contributed to salt in the diet. The four main goals were to achieve high level commitment from the food industries, to obtain individual company agreements and action plans; to develop product-specific targets for salt levels in major food categories; and to promote good practice and innovation by food companies.
The food industry engaged willingly in the strategy and over the first three years, commitments to salt reduction were received from 19 companies (including retailers, manufacturers, quick-food service and contract caterers) and detailed action plans from 10. A range of targets for salt reductions, most between 5-40%, were established to be delivered over the following few years. For example a major supermarket and snack food company committed to reducing the salt content of their products by 25% over five years, directly in line with the AWASH strategy. Media work to promote the good practice of food companies in relation to salt was a key element of the AWASH food industry strategy.
Food and Health Dialogue (FHD) targets
AWASH and the Heart Foundation both contributed to raising the profile of salt reduction on the government’s agenda, including the establishment of the FHD in 2009 and the setting of salt reduction targets (42). The FHD brought the Federal Department of Health together with food companies and public health organisations, including the Heart Foundation and the Public Health Association, to agree action plans to improve the health of diets. Over the next four years salt level targets were set for 9 different categories of processed foods (bread, ready to eat breakfast cereals, simmer sauces, processed meats, soups, savoury pies, potato/corn/extruded snacks, savoury crackers and cheese) (43). Timescales for reporting were between 2010 and 2013. However, there has been some speculation as to the future of the FHD since the new government was elected in 2013 and many of the scheduled monitoring reports were very late or still missing in 2014 (43). The Australian Government’s Assistant Health Minister, said in June 2014 that she was “currently considering the best and most appropriate way forward for the Food and Health Dialogue” (44) but no announcement have yet been made.
Changing consumer behaviour
The Australian Dietary Guidelines recommend limiting foods containing added salt but there has been no coordinated public awareness campaign to try and change consumer behaviour. The AWASH Drop the Salt! Campaign has a website, disseminates leaflets and undertakes regular media activity to try and raise awareness about the importance of reducing salt. In 2013, the Heart Foundation launched the “Halt Hidden Salt” consumer and advocacy initiative to raise the community’s awareness of the issue and garner support for salt reduction advocacy activities. The Heart Foundation Campaign also provides direct advice to consumers to change behaviour, for example “Adding Something Else”, “Sticking To Fresh”, “Reading Labels” and “Knowing Your Foods” (45). However, whilst important, both of these initiatives have limited reach and are unlikely to result in mass behaviour change at this stage.
Front of pack labelling
Front of pack labelling on packaged food is another tool that can be used both to drive food industry reformulation, and to change consumer behaviour in relation to salt. The Heart Foundation’s Tick scheme has helped consumers to make healthier choices within specific food categories for 25 years (46). In 2006, the food and beverage industry introduced the % daily intake (%DI) scheme and encouraged companies to include this information on front of pack (47). However, both schemes are voluntary and public health organisations have been calling on government to introduce a mandatory front of pack scheme. More recently, all nine Australian governments, and the government of New Zealand, endorsed the voluntary Health Star Rating interpretive front-of-pack-labelling system, developed jointly by health groups, industry and government, which applies to all packaged, manufactured or processed foods ready for sale, with the exception of agreed exemptions. As part of the Health Star Rating symbol, nutrient information on saturated fat, sugars, sodium and one optional positive nutrient relevant to the food can be displayed (48) along with the optional use of the word ‘high’ or ‘low’ where relevant criteria are met. A government funded education campaign is being planned to support the roll out of the Health Star Rating system.
FoodSwitch smartphone application
In response to the previous lack of government initiative in assisting consumers make healthier food choices, The George Institute partnered with Bupa Australia and in 2012 launched the FoodSwitch smartphone application (49,50). The app is supported by a comprehensive nutrition composition database which is updated annually and relies heavily on crowdsourcing. As an important tool for advocacy as well as behaviour change, the app allows consumers to scan the barcodes of food products and be immediately presented with the nutrition information interpreted in the form of colour–coded traffic light labels and provides a list of similar products that are healthier. Over 500,000 users have downloaded and regularly update the app which now includes a SaltSwitch option for people who are particularly interested in controlling their salt intake (49).
State-based work in public institutional settings
In addition to federal government action, many state and territory governments have developed settings based policies and guidelines that could influence the amount of salt in schools, health facilities, including public hospitals, and the workplace (51-55). However, salt is usually only one component of a wider nutrition policy and implementation is often minimally funded, if at all. For example, the Tasmanian State Government adopted the Tasmanian Food and Nutrition Policy in 2004 which specifies their commitment to promoting healthy eating including reducing salt intakes (56-59). The Victorian state government has developed a number of healthy food and drink policies and guidelines for settings such as schools, public hospitals, workplaces and residential aged care facilities which include sodium limits in the nutrient criteria (60) and has a Healthy Eating Advisory Service to support organisations in the aforementioned settings to meet the food and drink guidelines, including salt reduction (61).
Monitoring and evaluation
As the recent nationally representative AHS survey was based on repeat dietary recall, and other previous and recent surveys have used 24-hour urine and been non-representative, it has not been possible to demonstrate a reduction in population salt intake since 2005. In relation to the key implementation activities, there have been some research institute efforts to assess the impact of programs of work with the food industry and a further study on consumer behaviour. However, there have not yet been any attempts to assess the impact on salt arising from labelling initiatives or work in settings.
A recent study examining changes in the sodium content of the first three FHD targets—bread, breakfast cereals and processed meats—showed that there had been significant reductions (9%, 25% and 8% respectively) in each of the product categories, both by companies that had signed up to the targets and others (18). The targets were set in 2010 to be achieved by 2013. Previous analysis of changes in the sodium levels of pasta sauces, ready meals and bread showed that there had been limited change (62-64). Likewise, there were only very small changes in the sodium content of fast foods over the three years between 2009 and 2012 (65). The authors state that the new changes show that companies are able to make changes in response to the targets and provide a strong case for strengthening and extending the work of the FHD (18).
Whilst not nationally representative, a recent regional survey of KAB on salt also demonstrated that levels remained the same as in previous surveys (66).
Discussion
This review has assessed the existing programs of work on salt reduction in Australia between 2005 and 2015 against the criteria outlined in a framework for national salt reduction strategies (Table 1). A number of different initiatives exist and some evidence of progress has been documented. However, most of the activity to date has been led by NGOs. Whilst the impact of these organisations is impressive, there is a need for stronger government leadership to ensure that Australia will be able to meet its commitment to the global targets to reduce salt intake by 30% over the next decade.
The UK is well on its way to demonstrating that such a target is achievable. It launched its salt reduction strategy in 2003 and by 2013 had reported a 1.4 g (15%) reduction (67) in population salt intake, with parallel reductions in blood pressure estimated to be saving around 9,000 lives a year (68). It did this through a well-funded multi-faceted strategy combining the establishment of clear salt levels targets for the food industry to achieve, a sustained and wide-reaching consumer social marketing campaign and traffic light labelling (69). The main response of the Australian government to date is the FHD which brings together government, the food industry and NGOs. However, progress has been extremely slow: the FHD took more than four years to set targets for just 11 food categories, compared to three years for 80 voluntary targets in the UK, and 2 years for legislation on 14 targets in South Africa (70). A previous review of the FHD concluded it was inefficient and increased resources and more focus was needed (43). Whilst The FHD is making an impact as highlighted through this review, the existing government needs to make a stronger commitment to this program including through the provision of adequate funds.
The recently established Health Star Rating scheme could be a further opportunity to drive reformulation as well as informing consumers about the relative healthiness of different food products. However, it is too early to know what the update of this might be or whether it will have an impact. The fact that both the FHD and the Health Star Rating scheme are voluntary initiatives means that there is no way of holding different companies to account if they don’t comply and many would argue that legislation to mandate industry action would be a more effective approach (43,69,70).
Overall, analysis of existing activity in Australia against the framework for salt reduction strategies (19) shows that there are at least three major gaps: lack of sustained, high-level commitment, including salt reduction specific investment, across all levels of government to salt reduction; no existing national mechanisms for monitoring salt intake, and; no co-ordinated campaign to influence consumer attitudes and behaviour. The continued role of NGOs and research organisations and the new state levels activity in Victoria will provide important influences in this respect. However, the time required to build meaningful cross-sector (NGO, industry, government) recognition and alignment on the issue, particularly in view of government reticence to regulate, means that that further immediate action is required.
The VicHealth partnership provides a useful opportunity to both have a direct impact at State level and to influence federal government action. The State of Victoria is home to leading food industry organisations, many of whom are already engaged in reducing the salt content of their products. This means Victoria is well positioned to foster innovation and creative approaches to promoting salt reduction. It is also likely that action in Victoria will stimulate further action in other Australian states, thus further increasing the pressure on federal government and multiplying the impact at a national level.
A key element of the VicHealth partnership will be public awareness activities to generate public debate and influence consumer behaviour, which have not before been implemented in Australia. Evaluation of this work will be significant as most assessments of salt-reduction activities to date have studied the outcomes of a multi-faceted intervention as a whole and do not enable any assessment of the impact of the different strands of the intervention (19).
This review demonstrated the limited activity in relation to monitoring different salt reduction activities, with existing salt intake estimates based on dietary surveys or non-representative survey samples. There is also no clear understanding of socio-economic differences. One report examining salt intake in relation to socio-economic status in children in Victoria showed that there was a marked difference, with children of low SES consuming 0.5 g per day more than those of high SES due to the fact that they are eating more sodium from convenience style foods including pies, sausage rolls, savoury sauces, potato chips (crisps) and processed meats (71). It is important that comprehensive nationally representative mechanisms for monitoring changes in salt intakes using 24-hour urine samples are established. This should include the population in general but also for specific population groups including Aboriginal and Torres Strait Islanders (72) and children, and across SES status.
As salt is the main vehicle for iodine fortification to reduce iodine deficiency, it is important that respective programs are effectively co-ordinated (73,74). In 2009, the Australian government mandated iodine fortification of salt in bread to help solve the problem of re-emerging iodine deficiency (75). This may correct iodine deficiency in children and adults (76) but will not adequately address the needs of pregnant women who will still need to take supplements. The fortification of all food-grade salt with iodine (Universal Salt Iodisation) would be a better approach to ensuring that all at risk groups benefited from fortification as well as being in harmony with salt reduction initiatives. In addition, future studies of this type should include co-ordination with iodine deficiency elimination programs as criteria for salt reduction strategies.
Conclusions
A salt reduction strategy would be highly cost-effective and has the potential to prevent thousands of deaths by reducing the burden of chronic disease in Australia. An effective strategy should be co-ordinated by government and include food reformulation, public education, food labelling and work in public institutional settings backed by a robust monitoring an evaluation strategy (42). Whilst, a number of initiatives have been established and some progress in relation to reducing salt levels in foods has been made, key elements of a co-ordinated strategy to reduce population salt intake in Australia are still missing. Both state and federal government have a responsibility to take further action on salt reduction to ensure that Australia is on track to achieve the global targets of a 30% reduction by 2025.
Acknowledgements
J Webster is supported by a joint National Health and Medical Research Council and National Heart Foundation Career Development Fellowship on International Strategies to Reduce Salt. She also receives additional funding from the NHMRC, Vichealth and the World Health Organization for work on salt reduction. E Dunford is supported by an NHMRC postdoctoral fellowship.
The views expressed in this publication are those of the authors and responsibility rests solely with the authors. Any views or opinions expressed in the publication do not necessarily represent the views and opinions of VicHealth, The George Institute for Global Health or the National Heart Foundation and these organisations assume no liability for any content or opinion expressed in the publication.
Disclosure: J Webster is the Director of the World Health Organization Collaborating Centre on Population Salt Reduction at the George Institute for Global Health and previously co-ordinated the Australian Division of World Action on Salt and Health.
References
- World Health Organization. 2008-2013 action plan for the global strategy for the prevention and control of noncommunicable diseases. Geneva, Switzerland, 2008.
- Nichols M, Peterson K, Alston L, et al. Australian heart disease statistics, 2014 (Accessed on 4th March, 2015). Available online: http://www.heartfoundation.org.au/SiteCollectionDocuments/HeartStats_2014_web.pdf
- Australian Bureau of Statistics. 3303.0 - Causes of Death, Australia, 2012 (Accessed on 4th March, 2015). Avalaible online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/3303.0main+features100012012
- He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens 2009;23:363-84. [PubMed]
- World Health Organization and World Economic Forum. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries, 2011 (Accessed on 4th March, 2015). Available online: http://apps.who.int/medicinedocs/documents/s18804en/s18804en.pdf
- Cobiac LJ, Magnus A, Barendregt JJ, et al. Improving the cost-effectiveness of cardiovascular disease prevention in Australia: a modelling study. BMC Public Health 2012;12:398. [PubMed]
- National Health and Medical Research Council. Nutrient Reference Values for Australia and New Zealand, 2006 (Accessed on 4th March, 2015). Available online: https://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/n35.pdf
- Webster J, Dunford E, Huxley R, et al. The development of a national salt reduction strategy for Australia. Asia Pac J Clin Nutr 2009;18:303-9. [PubMed]
- Keogh JB, Lange K, Hogarth R, et al. Foods contributing to sodium intake and urinary sodium excretion in a group of Australian women. Public Health Nutr 2013;16:1837-42. [PubMed]
- Charlton K, Yeatman H, Houweling F, et al. Urinary sodium excretion, dietary sources of sodium intake and knowledge and practices around salt use in a group of healthy Australian women. Aust N Z J Public Health 2010;34:356-63. [PubMed]
- National Health and Medical Research Council. Dietary Guidelines for all Australians. Canberra, Australia, 2003.
- Grimes CA, Campbell KJ, Riddell LJ, et al. Sources of sodium in Australian children's diets and the effect of the application of sodium targets to food products to reduce sodium intake. Br J Nutr 2011;105:468-77. [PubMed]
- Webster JL, Dunford EK, Neal BC. A systematic survey of the sodium contents of processed foods. Am J Clin Nutr 2010;91:413-20. [PubMed]
- Girgis S, Neal B, Prescott J, et al. A one-quarter reduction in the salt content of bread can be made without detection. Eur J Clin Nutr 2003;57:616-20. [PubMed]
- Chapman S. "Keep a low profile": pesticide residue, additives, and freon use in Australian tobacco manufacturing. Tob Control 2003;12 Suppl 3:iii45-53. [PubMed]
- Council of Australian Governments. National Healthcare Agreement 2012. Available online: http://www.federalfinancialrelations.gov.au/content/npa/healthcare/national-agreement.pdf
- Australian Government Department of Health. Summary of Food Categories Engaged under the Food and Health Dialogue to date, 2013 (Accessed on 4th March, 2015). Available online: http://www.foodhealthdialogue.gov.au/internet/foodandhealth/publishing.nsf/Content/summary_food_categories
- Trevena H, Neal B, Dunford E, et al. An evaluation of the effects of the Australian food and health dialogue targets on the sodium content of bread, breakfast cereals and processed meats. Nutrients 2014;6:3802-17. [PubMed]
- Webster JL, Dunford EK, Hawkes C, et al. Salt reduction initiatives around the world. J Hypertens 2011;29:1043-50. [PubMed]
- Australian Government Department of Agriculture. National Food Plan-Our food future, 2013 (Accessed on 13th March, 2013). Available online: http://www.agriculture.gov.au/style%20library/images/daff/__data/assets/pdffile/0011/2293328/national-food-plan-white-paper.pdf
- Australian Government Department of Health. National Nutrition Policy, 2013 (Accessed on 13th March, 2015). Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/phd-nutrition-health
- Australian Government Department of Health. National Diabetes Strategy Advisory Group (Accessed on 13th March, 2015). Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/ndsag
- WASH. World Action on Salt and Health, 2014 (Accessed on 4th March, 2015). Available online: http://www.worldactiononsalt.com/
- Heart Foundation Conference 2009: Hearts in focus celebration, collaboration and challenges. Available online: http://www.heartfoundation.org.au/SiteCollectionDocuments/Heart-Foundation-Conference.pdf
- National Heart Foundation of Australia. Tick Program, 2007 (Accessed on 22nd November 2013). Available online: http://www.heartfoundation.org.au/Information-for-professionals/pages/information-professionals.aspx
- Australian National Heart Foundation. For all Hearts: making a difference to Australia's Heart Health, 2013 (Accessed on 22nd November, 2013).Available online: http://www.heartfoundation.org.au/SiteCollectionDocuments/Heart-Foundation-Strategic-Plan-2013-2017.pdf
- National Heart Foundation of Australia. Halt Hidden salt for a healthier Australia, 2013 (Accessed on 22nd November, 2013). Available online: http://www.heartfoundation.org.au/driving-change/Halt-Hidden-Salt/Pages/default.aspx
- National Heart Foundation of Australia and the National Stroke Foundation. Saving lives reducing avoidable hospital admissions Towards a National Action Plan for Heart Attack and Stroke, 2013 (Accessed on 11th March 2015). Available online: http://www.heartfoundation.org.au/SiteCollectionDocuments/Budget%20Sub%202013-14%20%20FINAL.pdf
- National Health and Medical Research Council (Australia). Report of the Working Party on Sodium in the Australian Diet. Canberra, Australia, 1984.
- National Health and Medical Research Council. Dietary Guidelines for Australian Adults, 2003 (Accessed on 2nd December, 2012). Available online: https://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/n33.pdf
- Australian Government Department of Health and Ageing. Food Category Action Plans, 2012 (Accessed 2nd December, 2012). Available online: http://www.foodhealthdialogue.gov.au/internet/foodandhealth/publishing.nsf/Content/food-category-action-plans
- Australian Bureau of Statistics. 4364.0.55.008 - Australian Health Survey: Usual Nutrient Intakes, 2011-12, 2015 (Accessed 13th March, 2015). Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.008
- Commonwealth of Australia. Health Star Rating System. Canberra: Commonwealth of Australia, 2015 (Accessed on 13th March, 2015). Available online: http://healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/content/home
- McLean RM. Measuring population sodium intake: a review of methods. Nutrients 2014;6:4651-62. [PubMed]
- Land MA, Webster J, Chalmers J, et al. Correlation of salt intake with knowledge, attitudes and behaviours in Australian adults. Available online: http://journals.lww.com/jhypertension/Abstract/2012/09001/1119_CORRELATION_OF_SALT_INTAKE_WITH_KNOWLEDGE,.1038.aspx
- Jeffery P, Nowson C, Riddle L, et al. Quantifying salt and potassium intake in Victorian adults. Available online: http://journals.lww.com/jhypertension/Abstract/2012/09001/1118_QUANTIFYING_SALT_AND_POTASSIUM_INTAKE_IN.1037.aspx
- Grimes CA, Riddell LJ, Campbell KJ, et al. Dietary salt intake assessed by 24 h urinary sodium excretion in Australian schoolchildren aged 5-13 years. Public Health Nutr 2013;16:1789-95. [PubMed]
- Webster JL, Dunford EK, Neal BC. A systematic survey of the sodium contents of processed foods. Am J Clin Nutr 2010;91:413-20. [PubMed]
- Webster JL, Li N, Dunford EK, et al. Consumer awareness and self-reported behaviours related to salt consumption in Australia. Asia Pac J Clin Nutr 2010;19:550-4. [PubMed]
- Grimes CA, Riddell LJ, Nowson CA. Consumer knowledge and attitudes to salt intake and labelled salt information. Appetite 2009;53:189-94. [PubMed]
- Williams P, McMahon A, Boustead R. A case study of sodium reduction in breakfast cereals and the impact of the Pick the Tick food information program in Australia. Health Promot Int 2003;18:51-6. [PubMed]
- Webster J, Dunford E, Kennington S, et al. Drop the Salt! Assessing the impact of a public health advocacy strategy on Australian government policy on salt. Public Health Nutr 2014;17:212-8. [PubMed]
- Elliott T, Trevena H, Sacks G, et al. A systematic interim assessment of the Australian Government's Food and Health Dialogue. Med J Aust 2014;200:92-5. [PubMed]
- Commonwealth of Australia. Senate Community Affairs Legislation Committee. Canberra, Australia, 2014 (Accessed on 3rd June, 2014). Available online: http://parlinfo.aph.gov.au/parlInfo/download/committees/estimate/62633228-9eba-4c9e-88f7-46b152ef610a/toc_pdf/Community%20Affairs%20Legislation%20Committee_2014_06_03_2547_Official.pdf;fileType=application%2Fpdf#search=%222010s%202014%2006%20food%20and%20health%20dialogue%22
- National Heart Foundation. Halt Hidden Salt For A Healthier Australia. National Heart Foundation of Australia, 2014 (Accessed on 13th March, 2015). Available online: http://www.heartfoundation.org.au/driving-change/Halt-Hidden-Salt/Pages/What-You-Can-Do.aspx
- Heart Foundation. 25 years of Heart Foundation Tick National Heart Foundation, 2014 (Accessed on 4th March, 2015). Available online: http://www.heartfoundation.org.au/healthy-eating/heart-foundation-tick/Pages/default.aspx
- Australian Food and Grocery Council. Daily Intake Guide- Healthy Eating Made Easy. Australian Food and Grocery Council, 2011 (Accessed on 4th March, 2015). Available online: http://www.mydailyintake.net/
- Australian Government Department of Health. Front-of-pack labelling updates. Commonwealth of Australia, 2014 (Accessed on 26th March, 2014). Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/foodsecretariat-front-of-pack-labelling-1
- Bupa website. The Healthy Food Initiative. (Accessed on 21st February, 2012). Available online: http://www.bupa.com.au/health-and-wellness/tools-and-apps/mobile-apps/foodswitch-app-faq#About
- Dunford E, Trevena H, Goodsell C, et al. FoodSwitch: A Mobile Phone App to Enable Consumers to Make Healthier Food Choices and Crowdsourcing of National Food Composition Data. JMIR Mhealth Uhealth 2014;2:e37. [PubMed]
- Queensland Government. Smart Choices - Healthy Food and Drink Supply Strategy for Queensland Schools. Department of Eduction, Training and Employment, 2011 (Accessed on 21st November, 2013). Available online: http://education.qld.gov.au/schools/healthy/food-drink-strategy.html
- Queensland Government. Healthy Choice Catering. In: Department of Justice and Attorney-General. Available online: https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0007/82951/healthy-choice-info-sheet.pdf
- Queensland Government. Growing Strong: Feeding You and Your Baby. Queensland Government, 2012 (Accessed on 21st November, 2013). Available online: http://www.health.qld.gov.au/ph/documents/hpu/growing_strong.asp
- Tasmanian School Canteen Association. School Canteen Accreditation Program. Tasmanian School Canteen Association, 2010 (Accessed on 21st November, 2013). Available online: http://www.tascanteenassn.org.au/accreditation/
- Eat Well Tasmania Incorporated. Eat Well Tasmania, 2009 (Accessed on 21st November, 2013). Available online: http://www.eatwelltas.org.au/
- Tasmanian Government. Tasmanian Food and Nutrition Policy, 2004 (Accessed on 21st November, 2013). Available online: http://www.dhhs.tas.gov.au/__data/assets/pdf_file/0009/81747/Tasmanian_food_and_nutrition_policy_2004.pdf
- NSW Health. Healthy Living. NSW Government, 2013 (Accessed on 10th December, 2013). Available online: http://www.health.nsw.gov.au/healthyliving/Pages/default.aspx
- Healthy Kids Association. Fresh Tastes @ School NSW Healthy School Canteen Strategy. Healthy Kids Association, 2013 (Accessed on 10th December, 2013). Available online: http://healthy-kids.com.au/school-canteens/the-menu/fresh-tastes-school/
- Department of Education. Canteen nutrition and healthy eating. Northern Territory Government of Australia, 2013 (Accessed on 10th December, 2013). Available online: http://www.education.nt.gov.au/about-us/policies/documents/schools/canteen-policy
- Department of Health and Human Services, State Government of Victoria, Healthy Together Victoria. State Government of Victoria, Australia, 2013 (Accessed on 20th November, 2013). Available online: http://www.health.vic.gov.au/prevention/healthytogether.htm
- Department of Health Victoria Australia. Healthy Eating Advisory Service. Department of Health, Victoria, Australia, 2013 (Accessed on 20th November, 2013). Available online: http://docs.health.vic.gov.au/docs/doc/The-Victorian-Healthy-Eating-Advisory-Service
- Trevena H, Dunford E, Neal B, et al. The Australian Food and Health Dialogue - the implications of the sodium recommendation for pasta sauces. Public Health Nutr 2014;17:1647-53. [PubMed]
- Christoforou AK, Dunford EK, Neal BC. Changes in the sodium content of Australian ready meals between 2008 and 2011. Asia Pac J Clin Nutr 2013;22:138-43. [PubMed]
- Dunford EK, Eyles H, Mhurchu CN, et al. Changes in the sodium content of bread in Australia and New Zealand between 2007 and 2010: implications for policy. Med J Aust 2011;195:346-9. [PubMed]
- Garcia J, Dunford EK, Sundstrom J, et al. Changes in the sodium content of leading Australian fast-food products between 2009 and 2012. Med J Aust 2014;200:340-4. [PubMed]
- Land MA, Webster J, Christoforou A, et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int J Behav Nutr Phys Act 2014;11:47. [PubMed]
- Shankar B, Brambila-Macias J, Traill B, et al. An evaluation of the UK Food Standards Agency's salt campaign. Health Econ 2013;22:243-50. [PubMed]
- He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open 2014;4:e004549. [PubMed]
- Charlton K, Webster J, Kowal P. To legislate or not to legislate? A comparison of the UK and South African approaches to the development and implementation of salt reduction programs. Nutrients 2014;6:3672-95. [PubMed]
- Webster J, Trieu K, Dunford E, et al. Target salt 2025: a global overview of national programs to encourage the food industry to reduce salt in foods. Nutrients 2014;6:3274-87. [PubMed]
- Grimes CA, Campbell KJ, Riddell LJ, et al. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross-sectional study. BMJ Open 2013;3. [PubMed]
- Lawrence CG. The urgency of monitoring salt consumption and its effects in Aboriginal and Torres Strait Islander Australians. Med J Aust 2013;198:365-6. [PubMed]
- World Health Organization. Salt reduction and iodine fortification strategies in public health-report of a joint technical meeting. World Health Organization, 2014 (Accessed on 15th March, 2015). Available online: http://apps.who.int/iris/bitstream/10665/101509/1/9789241506694_eng.pdf
- Webster J, Land MA, Christoforou A, et al. Reducing dietary salt intake and preventing iodine deficiency: towards a common public health agenda. Med J Aust 2014;201:507-8. [PubMed]
- Food Standards Australia and New Zealand. Proposal P230 - Iodine Fortification. Available online: http://www.foodstandards.gov.au/code/proposals/pages/proposalp230iodinefo2802.aspx
- Australian Bureau of Statistics. Australian Health Survey: Biomedical results for nutrients, 2011-2012. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.006Chapter1102011-12