Assessment of the effect of off-pump coronary artery bypass (OPCAB) surgery on right ventricle function using strain and strain rate imaging
Introduction
Reduced right ventricular function is a common finding in coronary artery bypass graft surgery (CABG) which can cause heart failure and increase mortality after surgery (1-4). Although the underlying mechanism is not clear, such a condition is attributed to different causes such as intraoperative ischemia, intraoperative myocardial damage, and the use of cardiopulmonary pump (CPB) (5,6). Several studies have shown that intraoperative right ventricle dysfunction can last up to 6 months after the surgery (7-9). Some other studies have reported that the echocardiographic right ventricular dysfunction can last up to even 1 year after CABG (2,10); nevertheless, due to improved levels of exercise stress test, some studies have considered a minor clinical value for such disorders (2).
On the other hand, nowadays, off-pump coronary artery bypass surgery (OPCAB) or beating heart is accepted as a procedure that allows the surgeon to perform CABG on a beating heart without aortic cannulation and clamp (11,12) and it has been proved as a safe and effective way whose long-term patients survival rate do not differ with that of on-pump CABG (13). Although CPB, which is one of the possible causes of reduced right ventricular function, is not used in this type of surgery, several studies have reported declined right ventricular function after this type of surgery; the rate of decline immediately after surgery was similar to that of on-pump technique (3).
Echocardiographic assessment of left ventricular function is simple, however due to the complex anatomy of the right ventricle; it is difficult to evaluate its performance by echocardiography. Therefore, different methods have been used to assess right ventricular function of which it can be named tricuspid annular motion or TAM measurement, which is actually an estimate of ejection fraction, tricuspid annular velocity or TAV, and tissue Doppler imaging or TDI (10). However, the procedure of strain and strain rate imaging (SRI), which is an exact method for assessment of right ventricular function, has been used rarely (14). Accordingly, this study aimed to evaluate the right ventricular function in patients undergoing OPCAB surgery using strain and SRI.
Materials and methods
This study was conducted on 30 patients, candidate for elective OPCAB surgery, in Modarres Hospital, between 2011 and 2012. The main criterion for the inclusion was the electiveness of the surgery. Exclusion criteria were: the absence of sinus rhythm, emergency cardiac surgery or repeated CABG, the presence of tricuspid regurgitation or the need to repair it, myocardial infarction in right ventricle, and severe mitral or tricuspid valve disease. The study received ethical approval from the ethics committee of Shahid Beheshti University of Medical Sciences.
After explaining the aims of the study to patients and obtaining their written informed consent, the researchers performed standard echocardiography including different views of parasternal, long axis parasternal, apical, and apical 4 chambers, short axis apical 2 and 3 chambers. Right ventricular function of patients was examined by strain and SRI echocardiography and the following items were determined through echocardiography: tricuspid annular plane systolic excursion (TAPSE), strain and SRI of right ventricle and tissue Doppler imaging or TDI at lateral annulus of tricuspid valve. Then patients underwent OPCAB. Echocardiography was performed again 6 days and 3 months after surgery and the results obtained from the three stages were compared with each other. All of the echocardiographic measurements in our study were done by an experienced echocardiographer. To assess intraobserver variability, one experienced echocardiographer measured the strain data, with the second set of measurements performed 2 weeks later.
SPSS 18 software was used for data analysis. In order to describe the variables we used mean and standard deviation, and to compare the values obtained before surgery, 6 days and 3 months after the surgery we used repeated measures ANOVA test and its non-parametric equivalent i.e., Friedman test. To compare pairs of means we used paired t-test and its non-parametric equivalent i.e., Wilcoxon signed-rank test. P value <0.05 was considered as the significant level.
Results
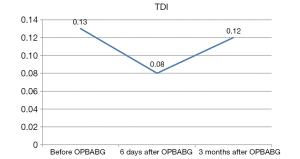
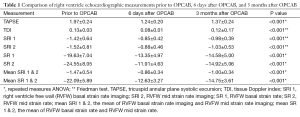
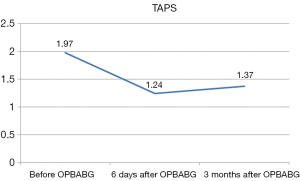
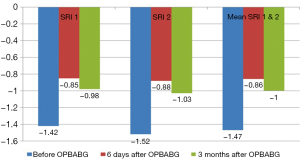
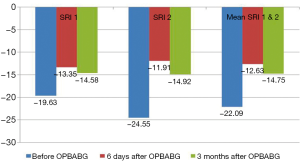
Participants included 30 patients (23 males and 7 females) with a mean age of 66±11 years (ranged from 49 to 83 years). Table 1 and Figures 1-4 show the comparison between echocardiography items before surgery, 6 days after surgery and 3 months after surgery. As it can be observed, in all cases there is a difference between measurements (P<0.001), so that the measured values of 6 days and 3 months after surgery are significantly lower than preoperative values; the values obtained 3 months after surgery are also significantly higher than those obtained 6 days after the surgery. In other words, right ventricular function had deteriorated 6 days after surgery, but the amount of the loss was compensated 3 months after surgery. According to this point that all measurements were performed by one experienced echocardiographer, the intraobserver variability was 0.90 (range, 0.79–0.97).
Full table
Discussion
The findings of this study are consistent with other studies in this field, and showed that after coronary artery surgery a decline occurs in right ventricular function. However, more detailed quantitative strain and SRI parameters which were measured in our study showed that at the early days after the OPCAB surgery there was a decline in the right ventricle function which was relatively reversible at longer intervals (3 months after surgery).
CABG, as the common method of coronary artery bypass, is performed using CPB on the stopped heart. The main advantage of this method is convenient and easy access to coronary artery which facilitates accurate anastomosis in an environment with good vision and without moving (15). On the other hand, in the off-pump CABG the surgery is operated on the beating heart without the use of a pump; it does not have complications associated with the use of the pump and is a less invasive approach which has become popular in recent years (16). Several studies have been conducted about the superiority of this method and each study has given special consideration to a separate specific parameter.
Right ventricular dysfunction after cardiac surgery is a well-known phenomenon that can be observed immediately after cardiac surgery. Both contraction and filling of the right ventricular are impaired after CABG, however, the mechanism of this phenomenon is not yet known exactly. Right ventricular dysfunction is observed in all patients who undergo heart surgery, regardless of the use of CPB, the time of aortic clamping, the methods used for cardioplegia, and myocardial preservation (10). Although most studies have reported intraoperative and post-operative right ventricular dysfunction, but long-term results are not known. Although some studies have shown the recovery of ventricular function during the first 6 months after surgery (8), some other studies reported that the recovery of right ventricular function lasts up to 1 year after CABG (2,10).
Michaux et al. examined the effect of coronary artery bypass on right ventricular function in two groups of on-pump and off-pump surgery and reported that after the surgery, overall systolic function of right ventricle remained the same in the two groups, however, the diastolic function were reduced similarly in both groups and there was no significant difference between the two groups in terms of right ventricular echocardiographic findings. Accordingly, they stated that the effect of off-pump surgery on right ventricular systolic and diastolic functions was similar to those of on-pump procedures (3). Pegg et al. also examined the impact of on-pump and off-pump surgery methods on early and late right ventricular function. In their study, 60 patients with normal left ventricular function were randomly divided into two groups of on-pump and off-pump surgery and were examined 6 days after surgery and 6 months after surgery using cardiac magnetic resonance imagine. Right ventricular stroke volume index was reduced immediately after surgery in both groups and there was no difference between the two groups, however, after 6 months, all indices of right ventricular function in both groups got back to their preoperative levels. As a result, they found that although the changes in RV function happened after both types of surgery and with the same levels, in the long run these changes are reversible (8). Roshanali et al. studied right ventricular function after conventional CABG using TDI; they reported that right ventricular dysfunction after cardiac surgery remains up to a year after the operation (10).
As it was shown, various studies on right ventricular function after surgery with or without pump have resulted in different findings. Although right ventricular dysfunction after surgery is proven, the level and the duration of dysfunction in the postoperative period are still controversial. One of the reasons that can be cited in this context is the method of examining and measuring right ventricular function. Because different studies have used different methods to assess right ventricular function, hence different results have been obtained. The use of MRI is the best technique in this field; however, due to its high cost and lack of facilities in many health centers, it cannot be used as a conventional method for the evaluation of right ventricular function (17). Therefore, echocardiography, which is a noninvasive, inexpensive, and available method, is used for this purpose. However, assessing right ventricular function by echocardiography is not as easy as to assess left ventricular function. Nowadays, TDI and strain and SRI are used to assess right ventricular function (10,17). Since SRI shows clearer quantitative values and more objective parameters, especially when clinical status shows intangible results, it could indicate a more precise examination of right ventricle (18). Hence, in the present study to investigate the postoperative right ventricular function we used the strain and SRI, in addition to TAPS and TDI.
Consistent with previous studies, our results also indicated that the TAPS, TDI and strain and SRI of right ventricle had a significant decline 6 days after surgery, which was recovered slightly during 3 months after surgery. The level of recovery 3 months after surgery in comparison to 6 days after surgery was significant, which indicated the reversible nature of right ventricular function after cardiac surgery. However, the rate of dysfunction 3 months after the surgery was still significant, compared with its preoperative level. Rates of recovery to the initial state of each of these parameters were varied in such a way that the rate of recovery on the TDI was sharper and higher. Our study showed that there was more decline in right ventricle free wall (RVFW) strain rate (SR) and SRI in the middle (mid), compared to the base (basal). In addition to measuring these two parts, we algebraically calculated the mean of SR and SRI for both the middle and the base; consistent with other changes, they also showed reduced right ventricular function 6 days and 3 months after surgery. Although in most studies, many of the examined indicators are in line with each other, however, our study showed that the level of recovery of the right ventricle may vary based on different indicators. Therefore, it is recommended to conduct further studies to find the best and most appropriate indicators to assess and follow the right ventricle function. Our study was a single center study and was relatively unique in its time; strain echocardiography is a non-invasive modality; however, we enrolled only the patients who were fully consent after comprehensive explanation of the study for them. So, it was inevitable that a part of our candidate patients were not included in the study. On the other hand, off-pump cardiac surgery is less performed than on-pump cardiac surgery. This study could be as a pilot study and new window for future large and multicenter studies which will reveal more detailed results. Moreover, valuable clinical and systematic reviews could be published from results of various centers. It is recommended for future large sample-size studies to have long duration follow-up.
The small sample size, short time of the study, and lack of a comparison with patients who underwent on-pump surgery are the limitations of this study, however, it seems that our study to be one of the few studies on right ventricular function after cardiac surgery using the strain and SRI. Hence, it is recommended to conduct further broader, multi-center studies, to determine appropriate indicators to measure and follow the right ventricle function.
Conclusions
The present findings are consistent with other studies in this area and showed that a decline occurs in right ventricular function after the coronary artery surgeries. However, more detailed quantitative strain and SRI parameters which were measured in our study showed that at the early days after the OPCAB surgery there is a decline in right ventricle function which is relatively reversible at longer intervals (3 months after surgery). Hence, it is recommended to conduct longer studies to evaluate right ventricular function after this type of surgery.
Acknowledgements
The authors would like to acknowledge the support of Cardiovascular Research Center of Shahid Beheshti University of Medical Sciences in all steps of the investigation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Dávila-Román VG, Waggoner AD, Hopkins WE, et al. Right ventricular dysfunction in low output syndrome after cardiac operations: assessment by transesophageal echocardiography. Ann Thorac Surg 1995;60:1081-6. [Crossref] [PubMed]
- Hedman A, Alam M, Zuber E, et al. Decreased right ventricular function after coronary artery bypass grafting and its relation to exercise capacity: a tricuspid annular motion-based study. J Am Soc Echocardiogr 2004;17:126-31. [Crossref] [PubMed]
- Michaux I, Filipovic M, Skarvan K, et al. Effects of on-pump versus off-pump coronary artery bypass graft surgery on right ventricular function. J Thorac Cardiovasc Surg 2006;131:1281-8. [Crossref] [PubMed]
- Reichert CL, Visser CA, van den Brink RB, et al. Prognostic value of biventricular function in hypotensive patients after cardiac surgery as assessed by transesophageal echocardiography. J Cardiothorac Vasc Anesth 1992;6:429-32. [Crossref] [PubMed]
- Ascione R, Caputo M, Angelini GD. Off-pump coronary artery bypass grafting: not a flash in the pan. Ann Thorac Surg 2003;75:306-13. [Crossref] [PubMed]
- Rose EA. Off-pump coronary-artery bypass surgery. N Engl J Med 2003;348:379-80. [Crossref] [PubMed]
- Mishra M, Swaminathan M, Malhotra R, et al. Evaluation of Right Ventricular Function During CABG: Transesophageal Echocardiographic Assessment of Hepatic Venous Flow Versus Conventional Right Ventricular Performance Indices. Echocardiography 1998;15:51-8. [Crossref] [PubMed]
- Pegg TJ, Selvanayagam JB, Karamitsos TD, et al. Effects of off-pump versus on-pump coronary artery bypass grafting on early and late right ventricular function. Circulation 2008;117:2202-10. [Crossref] [PubMed]
- Wranne B, Pinto FJ, Hammarström E, et al. Abnormal right heart filling after cardiac surgery: time course and mechanisms. Br Heart J 1991;66:435-42. [Crossref] [PubMed]
- Roshanali F, Yousefnia MA, Mandegar MH, et al. Decreased right ventricular function after coronary artery bypass grafting. Tex Heart Inst J 2008;35:250-5. [PubMed]
- Cheng DC, Bainbridge D, Martin JE, et al. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology 2005;102:188-203. [Crossref] [PubMed]
- Puskas J, Cheng D, Knight J, et al. Off-Pump versus Conventional Coronary Artery Bypass Grafting: A Meta-Analysis and Consensus Statement From The 2004 ISMICS Consensus Conference. Innovations (Phila) 2005;1:3-27. [Crossref] [PubMed]
- Raja SG, Benedetto U, Chudasama D, et al. Long-term follow-up of off-pump and on-pump coronary artery bypass grafting. Innovations (Phila) 2014;9:122-9; discussion 129.
- Hanekom L, Cho GY, Leano R, et al. Comparison of two-dimensional speckle and tissue Doppler strain measurement during dobutamine stress echocardiography: an angiographic correlation. Eur Heart J 2007;28:1765-72. [Crossref] [PubMed]
- Kshettry VR, Flavin TF, Emery RW, et al. Does multivessel, off-pump coronary artery bypass reduce postoperative morbidity? Ann Thorac Surg 2000;69:1725-30; discussion 1730-1.
- Wan S, Yin AP, Arifi AA. Reducing inflammatory injury during cardiac surgery: off pump or on a better pump? Intensivmedizin und Notfallmedizin 2000;37:736-40. [Crossref] [PubMed]
- Manno BV, Iskandrian AS, Hakki AH. Right ventricular function: methodologic and clinical considerations in noninvasive scintigraphic assessment. J Am Coll Cardiol 1984;3:1072-81. [Crossref] [PubMed]
- Chow PC, Liang XC, Cheung EW, et al. New two-dimensional global longitudinal strain and strain rate imaging for assessment of systemic right ventricular function. Heart 2008;94:855-9. [Crossref] [PubMed]