African experiences of humanitarian cardiovascular medicine: a Kenyan perspective
Three models of humanitarian activities are described. The first model (hereby referred to as Model 1) is a school-based rheumatic fever and rheumatic heart disease (RF/RHD) prevention outreach program which offers diagnostic, preventive, educational and curative services to primary and secondary school children in various parts of the country. The second model (hereby referred to as Model 2) is a hospital-based cardiovascular outreach program located in Kericho, a highland tea growing region that has long been perceived as a “hot spot” for CVD. The third model (hereby referred to as Model 3) is a fixed clinic-based cardiovascular outreach in Kisumu, the lake shore town, about 400 kilometers west of Nairobi.
These programs provide: prevention services, early detection and prophylaxis, facilitation for further treatment, follow-up, early disease management, staff motivation, training in basic cardiology skills and increased local awareness of CVD to clinicians in there far-flung centers. Data from these programs is also presented, with two of the programs reporting Kericho County as a ‘hot spot’ in RF/RHD. Despite various challenges, the future is still bright with sustainable initiatives.
Key words: Cardiovascular disease (CVD); Kenya; Rheumatic heart disease (RHD); Congenital heart disease (CHD); Non-Communicable diseases (NCD)
Introduction
Cardiovascular services in Africa began in the 1970s. In Kenya, the first open heart surgery, closure of Atrial Septal Defect, was performed in 1973 (1). Although progress has been erratic and slow, diagnostic and curative services are currently being offered in most public and private institutions. However, most of the advanced services are still located in Nairobi, the capital city of Kenya. The rest of the population is left to travel long distances for these services. Those who manage to travel the distance find the public services congested and overwhelmed, while the private services are too expensive and therefore inaccessible and unaffordable. Humanitarian services reaching these vulnerable populations are therefore considered God sent by a majority of patients.
Rheumatic heart disease (RHD) is the most common heart disease in children and young adults in developing countries (2,3). It is primarily a disease of low income population, which explains its geographic occurrence. This often neglected condition remains a major problem in all age groups. Being a preventable disease, educating the community will significantly contribute to the reduction of its incidence. The other equally prevalent congenital heart diseases still pose a challenge to this community due to late presentation and scarcity of financial and human resources to effectively manage them. Humanitarian initiatives targeting people at grassroots level allow early detection and management of these conditions. Some of these activities need not be on a very large scale in order to make an impact because small but persistent humanitarian activities can help bridge the knowledge and service gap of cardiovascular diseases.
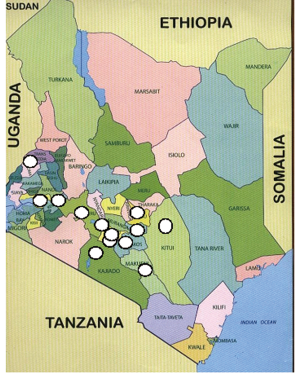
Centers of activity of the three Models described above are as follows:
Model 1 is the rheumatic fever and rheumatic heart disease awareness and prevention program carried out in primary and secondary school children in the country; it is run by the Mater Misericordie Hospital, Nairobi.
Model 2 involves providing regular (three monthly visits) cardiovascular outreach services to a rural hospital (Litein) in the highland region, about 350 kilometers south-western part of the country.
Model 3 is a clinic based cardiac outreach program in the lakeshore town of Kisumu Kenya, about 400 kilometers west of Nairobi. The map of Kenya Figure 1 indicates various locations in the country where these humanitarian activities have been carried out.
Program Model 1: the Mater rheumatic fever/rheumatic heart disease awareness and prevention project
This is a school-based rheumatic fever and rheumatic heart disease (RF/RHD) prevention outreach program run by the Mater hospital (4). It offers diagnostic, preventive, educational and curative services to primary and secondary school children in various parts of the country.
The Mater hospital was opened in 1962 by the Sisters
of Mercy, a Catholic order of Nuns, from Ireland. The
hospital was set up in Nairobi, to cater mainly for the
poor, indigenous Kenyans. With tremendous growth, the
hospital opened a cardiac unit in 1995 and its first open
heart surgery was performed in 1996. The hospital is now
well established with a successful cardiac program including
facilities and expertise required to investigate and carry out
corrective surgery (4). The RF/RHD program was initiated
by the Mater hospital management in 2008 as a charitable
community project wing of their cardiac program to serve
the primary schools of their neighboring slums dwellings.
It gained an instant popularity among the hospital staff
and later attracted funding and participation by local and
international community. The objectives of this outreach
program are mainly:
• To raise awareness of RF/RHD among primary and
secondary schools.
• To enhance primary prevention of RF/RHD by
screening and treating sore throats amongst school going
children.
• To offer treatment and secondary prophylaxis to those
screened and found to have RHD.
• To perform full cardiovascular evaluation, treatment
and professional advice free of charge to the patients found
to have any other cardiac ailments.
• To offer preventive education to the schools through
open air meetings, booklets and posters hence reduce the
incidence of the problem in the long term.
• To recommend and organize surgical intervention to
those in need of further treatment.
• To offer follow-up services to those recommended to
have local secondary prophylaxis.
Currently this program has a fixed calendar visiting an average of fifteen schools in a year.
Preparations for the camps
The preparation for the RF/RHD outreach camp is tedious and technically demanding. It begins with setting of the date and the school venue for the camp. The criteria for selecting a region is usually rotator in different counties in the country, however, special request by various schools is also considered. An advance team is then sent to the area to make a feasibility study of the region. This includes locating all the primary and secondary schools within the region, with the view of estimating the number of children who are likely to be screened. If the area is extremely needy, other corporate and organizations are approached and included in the ‘Mission’. For example, if the advance team finds a lot of dental caries, then the Kenya Dental Society and relevant corporate organizations are contacted to assist in various capacities. In case the region has many schools then more medical personnel are approached-with an adequate number of pediatric cardiologists joining the team. The camps are often held for one or two days depending on distance of location from Nairobi. All camps are held over the weekends.
The host’s role before and on the day of the camp is equally crucial. They assist in mobilizing students and parents both from their school and neighboring schools. They target those who have been unwell or absent from school on account of illness. The young children are usually accompanied by their parents. Local authorities have to assist in sending messages much earlier and providing security for the day. Local political and administrative leaders are invited. Their role has been found crucial in facilitating the camps. They assist in organizing and controlling the crowds (Figure 2). Parents have to take responsibilities in cases of referrals.
The Set-up, workflow and staffing during the camp
All the activities except the initial assembly are conducted in the classrooms. These rooms are divided into: registration, triage, de-worming, and observation, examination, specialists, cardiologist, treatment, pharmacy and data collection rooms. In-charge nurse supervises the work flow and is responsible for recruiting the patients into the charitable heart trust fund wing of the hospital. Other nurses take care of triage station, weighing and observation of the vital and anthropometric parameters of the students. The registration stations are manned by volunteers and non-nursing staff while de-worming is done by nurses. An assortment of clinicians including pediatricians, general clinicians often numbering eight to ten are needed to examine the children and treat sore throat. Patients suspected to have cardiac ailments are immediately referred to the pediatric cardiologist for further evaluation including echocardiography. The Pediatric cardiologists use portable ultrasound machines. Marketing, photography, records and data collection are run by Mater hospital staff. After the camp, another assembly is set and feedback is given on: the findings of the camp, the way forward, mentoring and encouraging the pupils. Brief career and other preventive talks are held, emphasizing the value of hand washing, good oral and dental hygiene.
The project is currently funded for the next three years and the plans are to reach all 47 counties (5) in Kenya (Figure 1). The main Co-funding agent is the Terre Des Hommes of Netherlands. Other corporate bodies that fund the project include the Kenya Commercial Bank and a mobile phone company-Safaricom.
Outcome of the school-based RF/RHD outreach prevention program
The RF/RHD outreach program which started as a pilot program in November 2008 in Nairobi County had spread to eleven counties as of April 2012, covering 23% of the region. A total of twenty seven thousand six hundred and sixty one students from sixty schools were screened for pharyngo-tonsillitis. Other cardiovascular and medical conditions were also attended to. All the children were “de-wormed” as part of primary health care. Four thousand two hundred and three patients (15%) received primary prophylaxis based on physical and throat examinations (Table 1) while 0.4% had secondary prophylaxis for RF. The highest number of primary and secondary prophylaxis was reported in Kericho County. This region had more students confirmed to have congenital and rheumatic heart disease. Nairobi County, where the sponsoring hospital is located, had the highest number of centers and schools attended to. Echocardiography was performed in 2.6% of this population.
| Table 1 Outcome of the school-based rheumatic fever awareness and prevention program | |||||||||
| Counties | No. Centres | Schools | No. Seen | 1° phy | 2° phy | Echo done | RF/RHD | CHD | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Nairobi | 5 | 14 | 4,831 | 444 | 14 | 66 | 6 | 4 |
| 2 | Kiambu | 3 | 8 | 3,416 | 308 | 16 | 50 | 16 | 3 |
| 3 | Kajiado | 1 | 2 | 907 | 80 | 0 | 0 | 0 | 1 |
| 4 | Machakos | 2 | 5 | 3,085 | 564 | 12 | 78 | 9 | 10 |
| 5 | Bungoma | 1 | 3 | 1,520 | 102 | 4 | 49 | 2 | 4 |
| 6 | Kitui | 3 | 8 | 3,556 | 303 | 15 | 119 | 20 | 25 |
| 7 | Kericho | 3 | 9 | 4,968 | 1,446 | 42 | 253 | 42 | 51 |
| 8 | Nakuru | 1 | 4 | 1,300 | 206 | 3 | 41 | 8 | 14 |
| 9 | Kisumu | 1 | 2 | 1,010 | 153 | 5 | 25 | 2 | 3 |
| 10 | Embu | 1 | 3 | 1,865 | 409 | 0 | 16 | 0 | 0 |
| 11 | Makueni | 1 | 2 | 1,203 | 188 | 3 | 23 | 3 | 4 |
| Totals | 22 | 60 | 27,661 | 4,203 | 114 | 720 | 108 | 119 | |
| Percentage of total seen | 15.19% | 0.41% | 2.60% | 0.39% | 0.43% | ||||
| Note: 1°, Primary; 2°, Secondary; Echo, Echocardiography; No, Numbers; Phy, Prophylaxis; RF, Rheumatic fever | |||||||||
Program Model 2: the hospital-based cardiovascular outreach program
This is a hospital-based cardiovascular outreach program located mainly in the highland (tea growing) region of the country. This region has long been perceived as a “hot spot” for cardiovascular diseases, based on previous referral patterns to the Mater Hospital heart units. The program is run from Litein hospital, located 350 kilometers south west of Nairobi.
This program was started in November 2006 at the Litein hospital because the hospital pediatrician regularly referred a high number of patients for cardiovascular evaluation to Nairobi. The Litein hospital is a mission hospital sponsored by the African Inland Church (AIC). It is situated in a highland region in Kericho County along the Kericho-Kisii highway. It was established in 1929 as a dispensary, and later upgraded to a cottage hospital. It is now a fully fledged hospital (since 1992) with a bed capacity of 200. It employs a pediatrician, a general surgeon and an obstetrician, with a visiting physician from the nearby government district hospital (6). It serves the surrounding districts of Kericho, Bomet, Kisii, Nyamira and also Olenguroni and Molo from the neighboring Nakuru district. The hospital also runs a nursing school. Other visiting teams include monthly visits from University of Nairobi, department of ophthalmology (7).
The cardiac clinic is run three to four times a year during the weekends so it does not interfere with routine hospital programs. The clinic days are scheduled for the whole year and are advertised within the hospital and the local language radio station. It uses the existing personnel in terms of nursing staff, medical personnel, laboratory and pharmacy. Inpatients are also attended to during the visits. The cardiologist uses a portable ultrasound machine while the hospital has its own ECG machine and radiology services. Most patients are booked by the hospital, with others walking in from nearby health facilities or even self-referrals. They are registered by the clerk, observed and monitored by nurses and then a twelve-lead single channel ECG is done before seeing the cardiologist. A highly subsidized package fee is offered to the patients but destitute ones get free evaluations and treatment.
Outcome of Litein hospital visits
Three hundred and eighty nine patients were seen over the six-year period from November 2006 to February 2012. A total of 18 visits were made to Litein Mission hospital during this period. Seventy one percent of the patients were aged below 20 years. Fifty five percent were females. Rheumatic heart disease was the most frequent diagnosis 157 (40.4%), followed by CHD 80 (20.6%), isolated pulmonary hypertension and cor-pulmonale 39 (10%), hypertensive heart disease 34 (8.7%), ischemic heart disease 16 (4.1%), cardiomyopathies 11 (2.8%) and congestive heart failure 7 (1.8%). Pulmonary hypertension was also noted to complicate congenital and rheumatic heart disease in 25 cases (11 CHD; 14 RHD) (Table 2).
| Table 2 Proportions of cardiovascular diseases at Litein Mission hospital | |||||||
| Diagnosis/Year | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Total (%) |
|---|---|---|---|---|---|---|---|
| RHD | 23 | 18 | 31 | 31 | 30 | 24 | 157 (40.4%) |
| CHD | 20 | 9 | 22 | 19 | 6 | 4 | 80 (20.6%) |
| PHT | 4 | 4 | 7 | 9 | 7 | 8 | 39 (10%) |
| HHD | 2 | 9 | 9 | 7 | 2 | 5 | 34 (8.7%) |
| IHD | 4 | 6 | 1 | 1 | 3 | 1 | 16 (4.1%) |
| CM | 1 | 1 | 3 | 3 | 2 | 1 | 11 (2.8%) |
| CCF | 0 | 0 | 3 | 2 | 2 | 0 | 7 (1.8%) |
| Others | 4 | 0 | 1 | 4 | 2 | 0 | 11 (2.8%) |
| Normal heart | 2 | 8 | 6 | 7 | 5 | 6 | 34 (8.8%) |
| Total | 60 | 55 | 83 | 83 | 59 | 49 | 389 (100%) |
| Note: CCF, Congestive cardiac failure; CM, Cardiomyopathy; HHD, Hypertensive heart disease; PHT, Pulmonary hypertension | |||||||
Management and outcomes of CHD and RHD
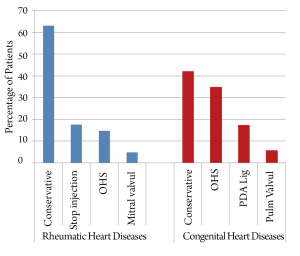
Of the 157 RHD cases, 63% were managed conservatively. This group either had mild or moderate valvular lesions requiring monthly injections or diuretics and digoxin. Another 17% were reassured and advised to stop their monthly prophylactic management after normal echocardiography follow-up findings. Open heart surgery was either indicated or performed in 15% of the patients. Closed heart intervention mainly mitral valvuloplasty was planned or performed in 5% of the cases (Figure 3). On the other hand, 42% of the CHD cases were managed conservatively especially in the small atrial and ventricular septal defects. Open heart surgery was planned or performed in 34.8% of the cases, with another 17.4% planned for Patent Ductus Arteriosus (PDA) ligation. Percutaneous pulmonary valvuloplasty was performed in 5.8% of the CHD cases (Figure 3).
Program Model 3: the Kisumu out-reach services
This is a fixed clinic-based cardiovascular outreach service. It is located in Kisumu, 400 kilometers west of Nairobi, along the shores of Lake Victoria. It is integrated with other services like neurology clinic, so as to cut cost and offer cross consultancy services. It offers cardiovascular services to the various general specialties and the local government hospital and serves a population which would otherwise have to travel long distances for a heart check-up. Being easy to reach by air, this self-sustaining unit offers consultancy services on a monthly basis. It serves about ten counties in three provinces, and uses the local hospitals to organize for simple procedures namely PDA ligation and pericardiocentesis.
Outcomes of Kisumu outreach program
Three hundred and sixty four (364) cardiac patients were seen at Kisumu between 2009 and 2012. Of these, 215 patients (59%) were females. Sixty three percent of the patients were aged below 20 years. Congenital heart disease was the most common diagnosis 81 (22.3%), followed by hypertensive heart disease 58 (15.9%), RHD 45 (12.4%) and isolated cor-pulmonale or pulmonary hypertension 33 (9.1%). Other diagnoses were: ischemic heart disease (IHD) 26 (7.1%), cardiomyopathy 20 (5.5%) and congestive cardiac failure 4 (1.1%). Fifty patients (13.7%) had other conditions such as infective endocarditis, atrio-ventricular block, among others. Forty seven patients (12.9%) referred for suspected cardiac disease had normal clinical and echocardiograph findings (Table 3).
| Table 3 Proportions of cardiovascular diseases in Kisumu, Kenya | |
| Echocardiographic Diagnosis | No. of Patients (%) |
|---|---|
| Congenital heart disease | 81 (22.3%) |
| Hypertensive heart disease | 58 (15.9%) |
| Rheumatic heart disease | 45 (12.4%) |
| Pulmonary hypertension | 33 (9.1%) |
| Ischemic heart disease | 26 (7.1%) |
| Cardiomyopathy | 20 (5.5%) |
| Congestive cardiac failure | 4 (1.1%) |
| Normal heart | 47 (12.9%) |
| Others (AV Block, MS, IE, Post op, PE etc) | 50 (13.7%) |
| Total | 364 (100%) |
| Note: AV, Atrial-ventricular; IE, Infective endocarditis; MS, Mitral stenosis; PE, Pericardial effusion; Post op, Post operation | |
Discussion
Like any other developing country, Kenya faces a double burden of disease: the devastating infections (malaria, tuberculosis, AIDs) and the non communicable diseases (diabetes, heart diseases, chronic pulmonary disease and cancers) (8). Kenya lacks a comprehensive health insurance policy and hence medical care in Kenya is not accessible to all particularly for the majority poor. The poor depend on local health clinics and government hospitals none of which have meaningful cardiovascular services. They often wait too long to seek medical advice and when it comes to a cardiac problem they must be referred elsewhere, often too late. Currently cardiovascular services are predominantly located in Nairobi, making them even inaccessible to those who can afford them. Outreach services then become handy to the rich and poor alike as evidenced by the outcomes of the current humanitarian programs. The role of three humanitarian programs in creating awareness, preventing and managing CVD in Kenya is explored in this article.
Humanitarian activities can be achieved by mobilization of huge resources from sponsors and interested parties. However, cumulative individual efforts can equally impact on improvement of cardiovascular diagnosis and treatment. In the late 1970s and early 1980s, consultants from the teaching and referral hospitals in Kenya would be empowered to conduct district and provincial hospital ward rounds as a way of continuously improving service delivery in those regions and interacting with the hospital personnel. These services gradually faded away and were replaced by tedious referral systems to the national tertiary care hospitals. From Tables 1,2,3, it is obvious that CVD at grassroots level are present and serious.
Program outcomes
Despite the initial hurdles 23% of the counties have been covered within three years. This positive trend is likely to escalate as the hospital recently repositioned its fund raising program to leverage the eradication of rheumatic heart disease. The outcomes of both the school-based and Litein hospital programs have singled out the Kericho highland region as having high prevalence of rheumatic heart disease creating a need for more targeted interventions to that community probably similar to what is being done among the ‘Maoris’ of Australia (9).
Few patients were initiated on RF prophylaxis in Nairobi County. The lower prevalence of RF in Nairobi could be due to the already existing awareness and prevention programs of RF/RHD in the capital city. This follows the fact that more specialists and charitable organizations in Kenya are based in Nairobi. In particular, the Kenya National Heart Foundation, supported by the World heart Federation, already runs RF/RHD awareness and prevention campaigns in Nairobi through their ‘Talking Wall Campaigns’ (10).
Program benefits
These humanitarian services are associated with several contributions. The programs have assisted in early detection of cardiovascular diseases and early prophylaxis, thus a good prevention program. Because the program is conducted during the weekends, the school going children are often accompanied by their parents and other siblings who are also examined and treated. By targeting the whole family (younger vulnerable siblings and the old adults) it is possible to offer a wholesome prevention. The already sick patients were referred and followed up for further treatment. The programs thus provided specialized services within reach hence demystification of specialized services - which would otherwise only be found in the capital city.
The school-based screening programs played a key role in increasing local awareness by partnering with the local Media in Kericho (11). They dedicated the whole day to deliver cardiovascular disease messages and talks in local dialect, interviewed patients and doctors widening the coverage of the program to an entire community. The role of the media is thus crucial in sustainable effective prevention and awareness programs.
The hospital based programs led to staff motivation and training in basic skills, like electrocardiograms and cardiac monitoring. Local initiatives to support the RF/RHD awareness programs have also emerged. For instance, the Mater hospital team was requested to hold a school screening in Kiambu County. This was a local initiative that was supported by a local dairy products cooperative society.
The programs could also influence future establishment of research activities. For instance, the high prevalence of RF/RHD in Kericho County maps a centre for future genetic and environmental research towards understanding this disease better. It also maps out an area for establishing a permanent cardiac service to cater for the needs of the community.
The current humanitarian activities have informed patients about cardiovascular facilities available in Kenya. Patients are thus aware about the programs, and that they can access the services within a short distance. The programs in Kisumu and Litein are now self-sustaining since structures are already in place and with fewer logistics, since it only requires a portable echocardiogram, cardiologist and a clerk. Of note is that some of the local physicians have now opted to specialize in cardiovascular medicine and will soon take over the running of these facilities.
Barriers and challenges
Future directions
With all these in place, Rheumatic fever prevention is feasible in Kenya. Such programs can be duplicated in other regions in the developing world.
Conclusions
The burden of CVD is rising in Kenya. The greatest number of RF/RHD was reported in Kericho County (Rift valley province) by two of the programs. Humanitarian activities have gone a long way in creating awareness and preventing CVD in Kenya. These programs also provide an avenue to better understanding of the pattern of these diseases.
Acknowledgements
Support of the following group(s) is highly acknowledged: (I) Stitching Netherlands and Prof. Olaf Penn, for their kind donation of the portable ultrasound machine; (II) Mater Hospital in Nairobi, through the Chief executive Officer (CEO), Dr John Muriithi and the Medical Director, Dr. Dolan Marian; (III) Terres Des Hommes, Kenya for cofunding the Mater camps;(IV) Safaricom, through their previous and present CEO (Michael Joseph and Bob Collymore); (V) Kenya Commercial Bank Head office and country branches; (VI) Director and staff, Litein Hospital; (VII) Prof. James Jowi, for establishing the Kisumu outreach program; (VIII) Duncan M. Matheka, for assisting in data entry, analysis and preparation of this article; (IX) Paediatric cardiologists who have been active in the Mater program (Dr. Grace Aketch, Dr. Loice Mutai, Dr. Gachara, Dr. Celestine Okello), Pediatricians (Dr. Makewa, Dr. Wanyoike, Dr. Muthiga and Dr. Florence Murila) and the Pediatric department, Mater Hospital.
Disclosure: Dr. Christine Yuko-Jowi is a pediatric cardiologist and is involved in the three outreach programs described in this article.
References
- Odhiambo PA. The first ten years of heart surgery in Kenya--aspirations, dilemmas and possibilities. East Afr Med J 1992;69:520-4.
- WHO Regional Committee for Africa. Cardiovascular diseases in African region: current situation and perspectives-report of the regional director 2005. Available online: http://www.afro.who.int/rc55/ documents/afr_rc55_12_cardiovascular.pdf
- Yuko-Jowi C, Bakari M. Echocardiographic patterns of juvenile rheumatic heart disease at the Kenyatta National Hospital, Nairobi. East Afr Med J 2005;82:514-9.
- The Mater Hospital Cardiac Program. Available online: http://www.materkenya.com/index.php/about-cardiacprogramme. html. Accessed 9th June 2012.
- Counties in Kenya. Available online: http://www. softkenya.com/county/. Accessed 9th June 2012.
- AIC Litein Hospital. Available online: http://www. liteinhospital.org/clinics. Accessed 9th June 2012
- Litein Hospital Eye Clinic by Department of Ophthalmology University of Nairobi. Available online: http://www.archive.uonbi.ac.ke/departments/about. php?dept_code=JV&fac_code=61§ion=about. Accessed 9th June 2012.
- UN report (2011). Countries facing double burden with chronic and infectious diseases. Available online: http://www.un.org/apps/news/story. asp?NewsID=38379&Cr=disease&Cr1
- National Heart Foundation of Australia (RF/RHD guideline development working group) and the Cardiac Society of Australia and New Zealand. Diagnosis and management of acute rheumatic fever and rheumatic heart disease in Australia - an evidence-based review. 2006.
- Kenya Heart National Foundation: Rheumatic Heart Disease Prevention Program. Available online: http:// www.kenyanheart.or.ke/rhdpp.html. Accessed 9th June 2012.
- Kass FM. Available online: http://www.kassfm.co.ke/ kassmedia/about-kass-media. Accessed 10th June 2012.