
Prevalence of obesity related hypertension among overweight or obese adults in River Nile State in Northern Sudan: a community based cross-sectional study
Highlight box
Key findings
• Prevalence of obesity related hypertension is high in River Nile State.
What is known and what is new?
• High prevalence of hypertension in River Nile State.
• There is a significant association between hypertension and obesity in River Nile State. Risk factors are age group above 40 years, unemployment, low education level, excessive coffee drinking, and marriage
What is the implication, and what should change now?
• Driving initiatives to mitigate the complications of hypertension.
• Primary care physicians may also need to pay more attention in obese individuals with hypertension to compliance with antihypertensive medications and improve awareness of patients about hypertension complications and to educate the public on prevention of hypertension and obesity and reducing salt intake.
• Study whether hypertension and obesity can be the driver behind the high prevalence of diabetes in River Nile state.
Introduction
Background
Hypertension is a major public health issue (1). It is estimated that nearly one quarter of the adults in the world have hypertension. The high prevalence of hypertension worldwide is due to different demographic and epidemiological factors particularly in the developing countries (2). Hypertension is the leading risk factor for disability and death (3). The risk factors for hypertension in Sudan and globally are age, obesity, alcohol consumption, smoking, behavioral, metabolic and genetic factors (4-6). The prevalence of hypertension is about 30% in in Sub-Saharan Africa and it increases over time (7,8). The prevalence and risk factors of hypertension were extensively studied in African countries (9-11). For instance, obesity is a well-recognized risk factor for development of hypertension (12) and hypertension is frequently associated with obesity (13,14). Furthermore, obesity increases the risk of death from type 2 diabetes mellitus (T2DM), cardiovascular disease, cancer, and chronic kidney disease (13). The existing relationship between hypertension and obesity is well studied in in both sexes (15). It has been suggested that high body mass index (BMI) and the increase of waist circumference are the strongest risk factors for developing hypertension and obese women have higher incidence of hypertension (16). Interestingly, maintaining a weight reduction of 4.5 kilograms for thirty months reduces the risk of developing hypertension by more than 60% (17) and elimination of obesity and high blood glucose could decrease the prevalence of hypertension (18). Treatment of hypertension in Obese patients is difficult because obese hypertensive patients need more antihypertensive medications (19). The prevalence of hypertension in Sudan was found to be 35.7 % (5,20) and the prevalence of obesity is also high in Sudan and this found to be 21.2% (21). Obesity is socially acceptable in Sudan and is considered a sign of wealth (21). Previous studies conducted in Khartoum, the capital of Sudan and Eastern Sudan showed the association of hypertension with obesity in Sudanese patients (21,22). For instance, in Eastern Sudan obesity in association with hypertension was found to be 32.7%, while in Khartoum, the capital of Sudan, the prevalence was 40.2%.
Rationale and knowledge gap
River Nile state is unique as large numbers of tribes of Sudan lives in the region, it is large agricultural hub for food and fruits with many workers travelling to and from the region. The study will be continuation of the series of previous studies conducted in the region about hypertension in urban, rural and different ethnic groups in River Nile state (4,5,20).
Objective
The aim of the present study is to determine the prevalence of hypertension in overweight and obese adults in the River Nile State and the associated other risk factors. This is first large study to assess the link between obesity and hypertension in River Nile State. We present the following article in accordance with the STROBE reporting checklist (available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-473/rc).
Methods
Study setting
This was a cross sectional community-based study conducted in in Shendi and Atbara cities at River Nile State, Sudan from January to June 2021. The study population was obese and overweight people living in Shendi and Atbara cities during the study period.
Inclusion criteria
Obese and overweight, aged 18 years and above and accepted to participate in the study were included in the study.
Exclusion criteria
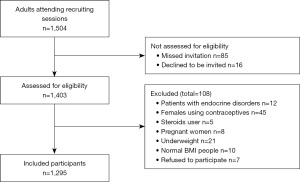
Individuals with diabetes and patients with other endocrine disorders, females using contraceptives, steroids user, pregnant women, underweight and normal BMI people and those who refused to participate in the study were excluded from this study to exclude the presence of confounders and any type of including selection bias (Figure 1).
Sample size and sampling technique
Convenience sample by which available number (in clubs, market, khalwa) of obese and overweight individuals living in River Nile State during the study period and fulfilled the inclusion criteria of the study were selected. To obtain suitable and representative sample, 2% from each of the two cities out of the total population (obtained from the local authorities of the two cities) was selected. The total population of Atbara was 111,399 persons and we selected 2% of them (824 persons) while the total population of Shendi city was 89,947 and we selected 2% of them (471) persons, so the total sample size was 1,295 participants (23,24).
Method of recruitment of study participants
Study participant were recruited by self-selection through advertisements in markets and clubs in the study area.
Data collection
Data was collected from participant after taking written consent and questionnaire was filled by the researchers. The questionnaire was validated questionnaire including information about the patients’ socio-demographic characteristics, clinical history and examination and possible risk factors for developing hypertension (25). Standardized pretest questionnaire was used to record medical history social and life style (21).
Anthropometric measurements
Weight and height were measured using calibrated equipment and standardized technique. Body weight was measured to the nearest 0.1 kg using a digital scale, and height was recorded to the nearest 0.1 cm using a wall-mounted stadiometer. Measurements were taken for each participant with light clothing and without shoes, and BMI was calculated by the following formula: weight in kilograms divided by height in meters squared (26). According to WHO, normal weight is defined as BMI =18.5–24.9 kg/m2; overweight as BMI =25–29.9 kg/m2; and obesity as BMI ≥30 kg/m2 (27), while obesity was classified into: obese class I (30–34.9 kg/m2), obese class II (35–40 kg/m2), obese class III (>40 kg/m2). Hypertension is correlated with high BMI and elevated waist-hip ratio. Growing evidence showed that the use of waist-hip ratio is more sensitive in identifying health risk than using the BMI and is also associated with obesity control (28). Waist circumference of the study participants was measured at the iliac crest highest point during minimal respiration. Hip circumference was measured at the maximum posterior protuberance of the buttocks. Waist hip ratio is calculated as the ratio of Waist circumference (cm) to hip circumference (cm) (29). Central obesity is defined as a waist circumference of >94 cm in males and >80 cm in females, or a waist to hip ratio of >0.90 in males and >0.85 in females (30,31).
Measurement of blood pressure (BP)
Two readings of BP were obtained using a mercury sphygmomanometer in the sitting position following rest for 15 minutes, and the second reading was used to confirm the diagnosis of hypertension (32). The diagnosis of hypertension is established in those with BP of ≥140/90 mmHg (32).
Statistical analysis
Data was analyzed using Statistical Packages for Social Sciences (SPSS) version 23.0 (IBM, Chicago, USA). Frequencies and Chi squire test was used when appropriate. The P value was considered significant if <0.05. Logistic regression test was performed to predict the presence of hypertension (BP more than or equal to 140/90 mmHg at the second time); which was the primary outcome variable of interest, among studied obese populations. The independent variables were age of the participants, occupation, associated disorders, waist/hip ratio and BMI. The reference category for weight classification in the logistic regression analysis was those who were overweight, while the reference category for waist/hip ratio in the logistic regression analysis were those who have normal values, while age was assessed as a continuous variable.
Ethical considerations
Ethical clearance was obtained from the ethics committee of Sudan Medical Specialization Board-Khartoum. Written informed consent from patients was obtained before participation. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Results
Socio-demographic characteristics of the participants
The participants aged 40–59 years were 608 (46.9%). Males were 717 (55.4%) and secondary level of education was reported in 395 (30.5%) of the participants while university/post-graduate was reported in 338 (26.1%). Unemployed participants were 577 (44.6%), workers were 395 (30.5%). The participants from rural areas were 773 (59.7%). The majority of the participants 1,093 (84.4%) were married. High waist to hip ratio (central obesity) was reported in 1,118 (86.3%) of the participants obesity class I was reported in 556 (42.9%) of the participants and 507 (39.2%) were overweight (Table 1).
Table 1
| Basic information | N | % |
|---|---|---|
| Age group | ||
| <20 years | 18 | 1.4 |
| 20–39 years | 350 | 27.0 |
| 40–59 years | 608 | 46.9 |
| 60 years and above | 319 | 24.6 |
| Gender | ||
| Male | 717 | 55.4 |
| Female | 578 | 44.6 |
| Educational level | ||
| Not educated | 199 | 15.4 |
| Primary | 363 | 28.0 |
| Secondary | 395 | 30.5 |
| University/above | 338 | 26.1 |
| Employment history | ||
| Unemployed | 577 | 44.6 |
| Employed | 718 | 55.4 |
| Residence | ||
| Urban | 522 | 40.3 |
| Rural | 773 | 59.7 |
| Marital status | ||
| Married | 1093 | 84.4 |
| Not married | 202 | 15.6 |
| Waist/hip ratio | ||
| Normal | 177 | 13.7 |
| High | 1118 | 86.3 |
| Weight status | ||
| Overweight (25–29.9) | 507 | 39.2 |
| Obese class I (30–34.9) | 556 | 42.9 |
| Obese class II (35–40) | 139 | 10.7 |
| Obese class III (>40) | 93 | 7.2 |
| Symptoms | ||
| None | 353 | 27.3 |
| Headache | 385 | 29.7 |
| Dizziness | 58 | 4.5 |
| Headache + dizziness | 499 | 38.5 |
| Comorbidities | ||
| None | 926 | 71.5 |
| Asthma | 128 | 9.9 |
| Cardiac diseases | 76 | 5.9 |
| Renal diseases | 124 | 9.6 |
| Asthma + renal disease | 10 | 0.8 |
| Cardiac disease + renal disease | 22 | 1.7 |
| Asthma, cardiac and renal | 9 | 0.7 |
| Previous history of HTN | ||
| Yes | 767 | 59.2 |
| No | 528 | 40.8 |
| First BP reading | ||
| Normal | 451 | 34.8 |
| High | 844 | 65.2 |
| Second BP reading | ||
| Normal | 268 | 20.7 |
| High | 1027 | 79.3 |
| Smoking | ||
| Yes | 287 | 22.2 |
| No | 1008 | 77.8 |
| Alcoholic | ||
| Yes | 100 | 7.7 |
| No | 1195 | 92.3 |
| Excessive coffee intake | ||
| Yes | 627 | 48.4 |
| No | 668 | 51.6 |
| Physically inactive | ||
| Yes | 635 | 49.0 |
| No | 660 | 51.0 |
HTN, hypertension; BP, blood pressure.
Comorbidities and lifestyle habits
The reported symptoms of hypertension were headache with dizziness 499 (38.5%) and 353 (27.3%) of the participants did not show any symptom of hypertension. The majority of the participants were healthy, 926 (71.5%). Apart from asthma 128 (9.9%), renal diseases 124 (9.6%), cardiac diseases 76 (5.9%). The first measurement of BP revealed high BP in 844 (65.2%) of the participants. After 15 minutes, the reading indicated hypertension in 1,027 (79.3%) of the participants and 268 (20.7%) of the participants were normotensive. While 287 (22.2%) were smokers, 100 (7.7%) were alcohol drinkers, 627 (48.4%) excessive coffee drinkers and the physically inactive participants were 635 (49.0%) (Table 2).
Table 2
| Socio-demographics | Second reading of BP | P value | ||||
|---|---|---|---|---|---|---|
| Normal (n=268) | High (n=1,027) | |||||
| n | % | n | % | |||
| Age groups | ||||||
| <20 years | 3 | 1.1 | 15 | 1.5 | <0.001* | |
| 20–39 years | 117 | 43.7 | 233 | 22.7 | ||
| 40–59 years | 115 | 42.9 | 493 | 48.0 | ||
| 60 years and above | 33 | 12.3 | 286 | 27.8 | ||
| Gender | ||||||
| Male | 156 | 58.2 | 561 | 54.6 | 0.16 | |
| Female | 112 | 41.8 | 466 | 45.4 | ||
| Educational level | ||||||
| Not educated | 29 | 10.8 | 170 | 16.6 | <0.001* | |
| Primary | 80 | 29.9 | 283 | 27.6 | ||
| Secondary | 64 | 23.9 | 331 | 32.2 | ||
| University/above | 95 | 35.4 | 243 | 23.7 | ||
| Occupation | ||||||
| Unemployed | 107 | 39.9 | 470 | 45.8 | 0.05 | |
| Employee | 161 | 60.1 | 557 | 54.2 | ||
| Residence | ||||||
| Urban | 115 | 42.9 | 407 | 39.6 | 0.18 | |
| Rural | 153 | 57.1 | 620 | 60.4 | ||
| Marital status | ||||||
| Married | 208 | 77.6 | 885 | 86.2 | <0.001* | |
| Not married | 60 | 22.4 | 142 | 13.8 | ||
| Waist/hip ratio | ||||||
| Normal | 101 | 37.7 | 76 | 7.4 | <0.001* | |
| High (central obesity) | 167 | 62.3 | 951 | 92.6 | ||
| Weight status | ||||||
| Overweight (25–29.9) | 173 | 64.6 | 334 | 32.5 | <0.001* | |
| Obese class I (30–34.9) | 86 | 32.1 | 470 | 45.8 | ||
| Obese class II (35–40) | 0 | 0.0 | 139 | 13.5 | ||
| Obese class III (>40) | 9 | 3.4 | 84 | 8.2 | ||
| Associated diseases | ||||||
| None | 231 | 86.2 | 695 | 67.7 | <0.001* | |
| Asthma | 19 | 7.1 | 109 | 10.6 | ||
| Cardiac diseases | 4 | 1.5 | 72 | 7.0 | ||
| Renal diseases | 10 | 3.7 | 114 | 11.1 | ||
| Asthma + renal | 0 | 0 | 10 | 1.0 | ||
| Cardiac + renal | 4 | 1.5 | 18 | 1.8 | ||
| Asthma, cardiac and renal | 0 | 0 | 9 | 0.9 | ||
| Symptoms | ||||||
| None | 124 | 46.3 | 229 | 22.3 | <0.001* | |
| Headache | 81 | 30.2 | 304 | 29.6 | ||
| Dizziness | 5 | 1.9 | 53 | 5.2 | ||
| Dizziness + headache | 58 | 21.6 | 441 | 42.9 | ||
| Life style habits | ||||||
| Physically inactive | 121 | 45.1 | 514 | 50.0 | 0.87 | |
| Smoking habits | 52 | 19.4 | 235 | 22.9 | 0.12 | |
| Excessive coffee | 173 | 64.6 | 454 | 44.2 | <0.001* | |
| Alcoholic | 15 | 5.6 | 85 | 8.3 | 0.08 | |
*, P values <0.05 are considered significant. BP, blood pressure.
Chi-square test revealed that the socio-demographic characteristics of the participants that significantly associated with hypertension were aged group above 40 years, unemployment, rural residence and married participants (P<0.001). Among the participants with high readings of BP (n=1,027), central obesity (elevated waist to hip ratio) was reported in 951 (92.6%) (P<0.001) indicates significant association between central obesity and elevated BP. Among patients with high BP, 470 (45.8%) were in class I obesity, 334 (32.5%) overweight (P<0.001) indicates significant association between obesity and overweight and hypertension. The number of the participants with normal BP who had no comorbidities was more than the participants with high BP readings (P<0.001). Furthermore, the number of normotensive participants and had no any symptoms were more than those who had high BP (P<0.001) (Table 2).
When logistic regression test was performed, we found that obese patient with class III category were more likely to have uncontrolled BP readings 3.7 times more than overweight ones [P<0.001, odds ratio (OR) =3.7; 95% confidence interval (CI): 1.7–7.9]. Moreover, those who have high waist/hip ratio were more likely to have uncontrolled BP by 5.16 times than those who have normal range (P<0.001; OR =5.16; 95% CI: 3.4–7.8). Those who had cardiac disease and obese or overweight were more likely to have uncontrolled BP 4.4 times more than those who didn’t (P=0.008; OR =4.4; 95% CI: 1.4–13.2). So we can conclude that age of the participants, associated disorders, waist/hip ratio, BMI were the predictors of the presence of hypertension (Table 3).
Table 3
| Variables | P value | OR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | <0.001* | 1.055 | 1.041 | 1.068 |
| Gender (males) | 0.92 | 1.019 | 0.678 | 1.532 |
| Educational level | ||||
| Uneducated (reference category) | 0.15 | – | – | – |
| Primary level | 0.88 | 1.0 | 0.597 | 1.8 |
| Secondary level | 0.12 | 1.5 | 0.884 | 2.7 |
| University level and above | 0.92 | 1.0 | 0.563 | 1.8 |
| Employment (un-employed) | 0.33 | 1.2 | 0.806 | 1.8 |
| Waist/hip ratio (high) | <0.001* | 5.16 | 3.4 | 7.8 |
| Weight status | ||||
| Overweight (reference category) | <0.001* | – | – | – |
| Obese class II | <0.001* | 2.0 | 1.4 | 2.9 |
| Obese class III | <0.001* | 3.7 | 1.7 | 7.9 |
| Associated disorder | ||||
| None (reference category) | 0.049* | – | – | – |
| Asthma | 0.05 | 1.7 | 0.9 | 3.2 |
| Cardiac disease | 0.008* | 4.4 | 1.4 | 13.2 |
| Renal disease | 0.03* | 2.1 | 1.0 | 4.3 |
*, P values <0.05 are considered significant. OR, odds ratio.
Discussion
Key findings
The prevalence of hypertension among the study participants was 79.3%. Obesity was present in 92.6% in hypertensive patients. Higher prevalence of hypertension was observed in age group above 40. Other risk factor for developing hypertension in our study are unemployment, low education level. Marriage increases the risk of developing hypertension. Excessive coffee drinking was associated with high prevalence of hypertension.
Strengths and limitations
The major strength of this study is the large sample size because the larger the sample size, the more accurate the average values. Larger sample sizes identify outliers in data and provide smaller margins of error. However, this study has some limitations. The cross-sectional design of the study does not allow establishment of conclusive relationship between risk factors and the hypertension. The study participants were recruited from Northern Sudan; therefore, conclusions of this study cannot represent the situation in other regions of Sudan.
Comparison with similar studies
The current study recruited slightly higher number of male (55.4%) than females (44.6%). Similar to studies in Turkey (33) and Ethiopia (9). The prevalence of hypertension was higher in males compared to females. Similar observations were noted in previous studies (9,34-36).
Explanation of findings
The prevalence of hypertension among the study participants was 79.3%. Obesity was present in 92.6% in hypertensive patients. Our data endorsed the previous observations by Bushara et al., Omar et al. and Noor et al. that obesity is an important risk for developing hypertension in Sudan (5,20,22). We showed that higher prevalence of hypertension was observed in age group above 40. This likely the common trend in countries surrounding Sudan. For instance, Mufunda et al. in Eriteria showed that hypertension is also common among those over 40 years old (34). While in China, higher prevalence of hypertension is noted in those aged 50–59 age group (36). The other risk factors for developing hypertension in our study are unemployment, low education level. Unemployment can cause stress and overfeeding which can cause obesity. The combination of obesity and stress can lead to hypertension. Previous studies reported an inverse relationship between obesity and level of education (37,38) and low prevalence of high BP is associated with higher education level (39,40). Noor et al. showed that low education level in Sudan is associated with high prevalence of hypertension (20). Similarly, in this study, we showed that low education level is associated with high prevalence of hypertension.
One interesting finding of our study is that marriage increases the risk of developing hypertension. This might be explained by the stress due to poor quality of life in the developing countries (41). It worth mentioning, part of the Sudanese culture is that newly married couples tend to be invited by extended families to different social events and meals within the first and second year of their marriage. Therefore, it is not surprising that marriage in some individuals can be associated with an increase in weight and obesity.
Coffee drinking can increase the BP (42) while other researchers showed that coffee can have protective effect against high BP (43). In our study excessive coffee drinking was associated with high prevalence of hypertension. Excessive coffee drinking could reduce the production of nitric oxide from the vascular endothelium leading to hypertension (44).
Implications and actions needed
Our study will alert the ministry of health in Sudan to design strategies and conduct more research on how to decrease the prevalence of hypertension and complications. We have previously shown in the River Nile state the admission to Atbara Teaching Hospital with non-communicable disease is more than the hospital admission with communicable disease (45). Therefore, this study is expected to have huge implications among health professional and individuals living in the region, in driving initiatives to mitigate the complications associated with hypertension like stroke and renal failure. Perhaps primary care physicians may also need to pay more attention in obese individuals with hypertension. It is imperative to check compliance with antihypertensive medications, improve awareness of patients about hypertension complications and to educate the public on prevention of hypertension and obesity and reducing salt intake. This study will also open the horizons to study whether hypertension and obesity can be the driver behind the high prevalence of diabetes in the River Nile State and whether it is important to educate public and health professional about management of diabetes and hypertension in Ramadan (46).
Conclusions
The study showed that there is a significant association between hypertension and obesity among the Sudanese population in Atbara and Shendi cities. Prevalence of hypertension among the study participants was 79.3%, while hypertension was present in 92.6% among those with central obesity. In order to control the high BP in obese patients, BP of these patients should be measured regularly. The most common risk factors associated with obesity related hypertension among adults were age group above 40 years, unemployment, low education level, excessive coffee drinking, and marriage.
Acknowledgments
The corresponding author would like to thank Ajman University for all supports.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-473/rc
Data Sharing Statement: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-473/dss
Peer Review File: Available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-473/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cdt.amegroups.com/article/view/10.21037/cdt-22-473/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sun J, Wang X, Terry PD, et al. Interaction effect between overweight/obesity and alcohol consumption on hypertension risk in China: a longitudinal study. BMJ Open 2022;12:e061261. [Crossref] [PubMed]
- Mills KT, Bundy JD, Kelly TN, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation 2016;134:441-50. [Crossref] [PubMed]
- GBD 2015 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1659-724. Erratum in: Lancet 2017;389:e1. [Crossref] [PubMed]
- Bushara SO, Noor SK, Elmadhoun WM, et al. Undiagnosed hypertension in a rural community in Sudan and association with some features of the metabolic syndrome: how serious is the situation? Ren Fail 2015;37:1022-6. [Crossref] [PubMed]
- Bushara SO, Noor SK, Ibraheem AA, et al. Prevalence of and risk factors for hypertension among urban communities of North Sudan: Detecting a silent killer. J Family Med Prim Care 2016;5:605-10. [Crossref] [PubMed]
- Vardell E. Global Health Observatory Data Repository. Med Ref Serv Q 2020;39:67-74. [Crossref] [PubMed]
- Ataklte F, Erqou S, Kaptoge S, et al. Burden of undiagnosed hypertension in sub-saharan Africa: a systematic review and meta-analysis. Hypertension 2015;65:291-8. [Crossref] [PubMed]
- Ranzani OT, Kalra A, Di Girolamo C, et al. Urban-rural differences in hypertension prevalence in low-income and middle-income countries, 1990-2020: A systematic review and meta-analysis. PLoS Med 2022;19:e1004079. [Crossref] [PubMed]
- Abebe S, Yallew WW. Prevalence of hypertension among adult outpatient clients in hospitals and its associated factors In Addis Ababa, Ethiopia: a hospital based cross-sectional study. BMC Res Notes 2019;12:87. [Crossref] [PubMed]
- Galson SW, Staton CA, Karia F, et al. Epidemiology of hypertension in Northern Tanzania: a community-based mixed-methods study. BMJ Open 2017;7:e018829. [Crossref] [PubMed]
- Manus MB, Bloomfield GS, Leonard AS, et al. High prevalence of hypertension in an agricultural village in Madagascar. PLoS One 2018;13:e0201616. [Crossref] [PubMed]
- Landsberg L, Aronne LJ, Beilin LJ, et al. Obesity-related hypertension: pathogenesis, cardiovascular risk, and treatment: a position paper of The Obesity Society and the American Society of Hypertension. J Clin Hypertens (Greenwich) 2013;15:14-33. [Crossref] [PubMed]
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Kardiol Pol 2019;77:71-159. [Crossref] [PubMed]
- Ahmed M, Kumari N, Mirgani Z, et al. Metabolic syndrome; Definition, Pathogenesis, Elements, and the Effects of medicinal plants on it's elements. J Diabetes Metab Disord 2022;21:1011-22. [Crossref] [PubMed]
- Faulkner JL, Belin de Chantemèle EJ. Sex Differences in Mechanisms of Hypertension Associated With Obesity. Hypertension 2018;71:15-21. [Crossref] [PubMed]
- Sun JY, Hua Y, Zou HY, et al. Association Between Waist Circumference and the Prevalence of (Pre) Hypertension Among 27,894 US Adults. Front Cardiovasc Med 2021;8:717257. [Crossref] [PubMed]
- Stevens VJ, Obarzanek E, Cook NR, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med 2001;134:1-11. [Crossref] [PubMed]
- Babaee E, Tehrani-Banihashem A, Eshrati B, et al. How Much Hypertension is Attributed to Overweight, Obesity, and Hyperglycemia Using Adjusted Population Attributable Risk in Adults? Int J Hypertens 2020;2020:4273456. [Crossref] [PubMed]
- Shupenina E, Vasyuk Y, Namazova G. Observational Prospective Study of Azilsartan Medoxomil/ Chlortalidone Compared with Irbesartan/ Hydrochlorothiazide Combination Therapy in Obese Hypertensives (Puzzle). J Hypertens 2022;40:e300. [Crossref]
- Noor SK, Elsugud NA, Bushara SO, et al. High prevalence of hypertension among an ethnic group in Sudan: implications for prevention. Ren Fail 2016;38:352-6. [Crossref] [PubMed]
- Ahmed MH, Ali YA, Awadalla H, et al. Prevalence and trends of obesity among adult Sudanese individuals: Population based study. Diabetes Metab Syndr 2017;11:S963-7. [Crossref] [PubMed]
- Omar SM, Musa IR, Osman OE, et al. Prevalence and associated factors of hypertension among adults in Gadarif in eastern Sudan: a community-based study. BMC Public Health 2020;20:291. [Crossref] [PubMed]
- Andrade C. The Inconvenient Truth About Convenience and Purposive Samples. Indian J Psychol Med 2021;43:86-8. [Crossref] [PubMed]
- Azzeh FS, Bukhari HM, Header EA, et al. Trends in overweight or obesity and other anthropometric indices in adults aged 18-60 years in western Saudi Arabia. Ann Saudi Med 2017;37:106-13. [Crossref] [PubMed]
- Pelosi C, Kauling RM, Cuypers JAAE, et al. Daily life and psychosocial functioning of adults with congenital heart disease: a 40-53 years after surgery follow-up study. Clin Res Cardiol 2022; Epub ahead of print. [Crossref] [PubMed]
- Chetoui A, Kaoutar K, Boutahar K, et al. Prevalence of overweight/obesity and its associated factors among a sample of Moroccan type 2 diabetes patients. Afr Health Sci 2021;21:23-31. [Crossref] [PubMed]
- Gurunathan U, Myles PS. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth 2016;116:319-21. [Crossref] [PubMed]
- Moges B, Amare B, Fantahun B, et al. High prevalence of overweight, obesity, and hypertension with increased risk to cardiovascular disorders among adults in northwest Ethiopia: a cross sectional study. BMC Cardiovasc Disord 2014;14:155. [Crossref] [PubMed]
- Wang Y, He J. Correlation of cardiovascular risk predictors with overweight and obesity in patients with familial hypercholesterolemia. Front Cardiovasc Med 2022;9:1026243. [Crossref] [PubMed]
- Molla MD, Wolde HF, Atnafu A. Magnitude of Central Obesity and its Associated Factors Among Adults in Urban Areas of Northwest Ethiopia. Diabetes Metab Syndr Obes 2020;13:4169-78. [Crossref] [PubMed]
- Alberti KG, Zimmet P, Shaw J, et al. The metabolic syndrome--a new worldwide definition. Lancet 2005;366:1059-62. [Crossref] [PubMed]
- Cooper RS, Wolf-Maier K, Luke A, et al. An international comparative study of blood pressure in populations of European vs. African descent. BMC Med 2005;3:2. [Crossref] [PubMed]
- Ardahan M, Konal E. The prevalence of hypertension and obesity and effective factors: A cross-sectional bazaar study. J Pak Med Assoc 2019;69:1018-21. [PubMed]
- Mufunda J, Mebrahtu G, Usman A, et al. The prevalence of hypertension and its relationship with obesity: results from a national blood pressure survey in Eritrea. J Hum Hypertens 2006;20:59-65. [Crossref] [PubMed]
- Wang J, Zhang L, Wang F, et al. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014;27:1355-61. [Crossref] [PubMed]
- Zhang Y, Hou LS, Tang WW, et al. High prevalence of obesity-related hypertension among adults aged 40 to 79 years in Southwest China. Sci Rep 2019;9:15838. [Crossref] [PubMed]
- Newton S, Braithwaite D, Akinyemiju TF. Socio-economic status over the life course and obesity: Systematic review and meta-analysis. PLoS One 2017;12:e0177151. [Crossref] [PubMed]
- Heraclides A, Brunner E. Social mobility and social accumulation across the life course in relation to adult overweight and obesity: the Whitehall II study. J Epidemiol Community Health 2010;64:714-9. [Crossref] [PubMed]
- Erceg M, Ivicević-Uhernik A, Kern J, et al. Is there any association between blood pressure and education level? The CroHort study. Coll Antropol 2012;36:125-9. [Crossref] [PubMed]
- Leng B, Jin Y, Li G, et al. Socioeconomic status and hypertension: a meta-analysis. J Hypertens 2015;33:221-9. [Crossref] [PubMed]
- Birditt KS, Newton NJ, Cranford JA, et al. Stress and Negative Relationship Quality among Older Couples: Implications for Blood Pressure. J Gerontol B Psychol Sci Soc Sci 2016;71:775-85. [Crossref] [PubMed]
- Noordzij M, Uiterwaal CS, Arends LR, et al. Blood pressure response to chronic intake of coffee and caffeine: a meta-analysis of randomized controlled trials. J Hypertens 2005;23:921-8. [Crossref] [PubMed]
- Yamaji T, Harada T, Hashimoto Y, et al. Relationship of Daily Coffee Intake with Vascular Function in Patients with Hypertension. Nutrients 2022;14:2719. [Crossref] [PubMed]
- Higashi Y. Coffee and Endothelial Function: A Coffee Paradox? Nutrients 2019;11:2104. [Crossref] [PubMed]
- Noor SK, Elmadhoun WM, Bushara SO, et al. The Changing Pattern of Hospital Admission to Medical Wards: Burden of non-communicable diseases at a hospital in a developing country. Sultan Qaboos Univ Med J 2015;15:e517-22. [Crossref] [PubMed]
- Ahmed M, Badi S, Elidrisi A, et al. Safety and effectiveness of newer antidiabetic medications during Ramadan fasting and safety of Ramadan fasting after bariatric surgery. J Diabetes Metab Disord 2022;21:1991-2004. [Crossref] [PubMed]


