The challenges of cardiothoracic surgery practice in Nigeria: a 12 years institutional experience
Introduction
Cardiothoracic practice in Nigeria is developing but faces multiple challenges that need to be overcome to enable sustainable practice. There is limited information in the literature about cardiothoracic practice in Nigeria and the challenges to practice (1-6). The aim of this study was to highlight the challenges to cardiothoracic practice in Nigeria by an analysis of our institutional experience as well as performing a survey of open heart surgery (OHS) activity in other Nigerian centers.
Institutional setting
The Lagos State University Teaching Hospital (LASUTH) is one of two teaching hospitals in Lagos. It is a 550 bedded hospital and the estimated population of Lagos is 21 million people (7). Initial cardiothoracic activity started in March 2004 with cardiac missions which continued till March 2006. The cardiothoracic division was formally established in August 2006 with the appointment of a British trained surgeon who was later joined by another surgeon from the USA. The team was gradually built up to include Anesthesia, Perfusion, Theatre and Intensive Care nurse practitioners.
The LASUTH programme started initially with thoracic and vascular surgery between 2006 and 2009 and by 2009 was in a position to recommence the OHS programme, combining occasional Cardiac mission visits and surgery by the resident team. A seed fund of 20 million Naira (15,000 USD) was provided by the Lagos State Ministry of Health which was used as the start of a revolving fund for the Cardiothoracic Unit to cover stocking of consumables, equipment repairs and training. A cardiothoracic store was thereafter developed and staffed. Beneficiaries of specialized cardiac training abroad includes two cardiothoracic residents, two anesthetic residents, two perfusionists, three theatre nurses and eight intensive care nurses.
Methods
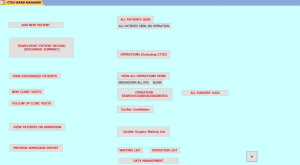
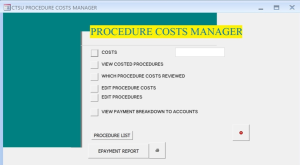
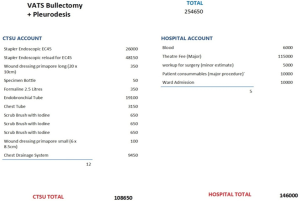
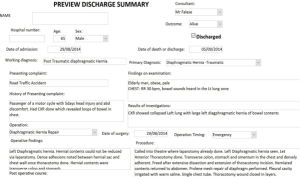
Various in-house Microsoft access databases were developed to support the cardiothoracic programme. These consisted of clinical databases (Open Heart Surgery, General Thoracic Surgery, Pacemaker implantation) as well as an accounting database to manage the revolving fund and a database for procedure costs to guide patients and the cardiothoracic staff in preparation for surgical procedures (Figures 1-3). Entry into the clinical databases was done prospectively and integrity of data continuously maintained as reports generated from the database were used for daily clinical review of patients and mandatory discharge summaries (Figure 4).
Data extraction from the clinical databases was performed. The study period was from March 2004 to December 2015. Data included patient demographics, clinical diagnosis, operative category, operation and mortality. All data was analyzed with Microsoft excel 2010. Summary data is presented as mean ± standard deviation or percentages as appropriate. Comparative analysis of categorical data was done using chi-squared or fishers test as appropriate and a P value of <0.05 was taken as significant.
A telephone survey of the clinical leads in the 15 institutions in Nigeria known to be performing OHS was done. Information requested was the type of institution (public or private), model of surgery (visiting team or a resident team), activity period and number of OHS procedures done.
Ethical approval
Data extraction for the purpose of this study was approved by the Institutional Ethics Committee of the LASUTH. There was no patient contact for the study so informed consent was not required. All the surgeons contacted for the survey gave verbal consent to participate in the survey.
Results
Distribution by clinical diagnosis
Various surgical procedures were done for 1,520 patients. Average age was 37±22.4 years. There were 813 males (53.5%). The ten most common clinical diagnoses were empyema thoracis (17.5%), malignant pleural effusion (14.7%), chest trauma (12%), hemodialysis access (6.1%), bradyarrhythmia (5.3%), aerodigestive foreign bodies (4.1%), vascular injury (3.9%), pericardial disease (3.8%), lung cancer (3.6%) and congenital heart disease (3.4%). Significant gender differences were noted only for blunt chest trauma (male 76.6%, female 23.4%), penetrating chest trauma (male 77.5%, female 22.5%), malignant pleural effusion (male 30%, female 70%) and vascular injury (male 87.9%, female 12.1%) (Table 1).

Full table
Distribution by operative categories and procedures
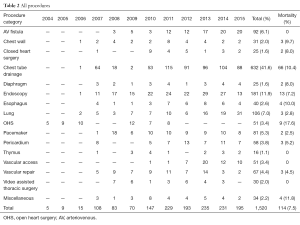
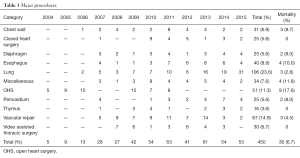
The operative categories were major (under general anesthesia), minor (under local anesthesia) and endoscopic procedures. The overall distribution of procedures (Table 2) was chest tube insertion (41.6%), endoscopy (11.9%), lung procedures (7%), arterio-venous fistula (6.1%), pacemaker implantation (5.3%), vascular repairs (4.4%), OHS (3.4%), vascular access for hemodialysis (3.4%), esophageal procedures (2.6%), miscellaneous procedures (2.2%), chest wall surgery (2%), video assisted thoracic surgery (2%), closed heart surgery (1.6%), diaphragmatic procedures (1.6%) and thymectomy (1%). The overall mortality was 112 (7.4%) (Table 2). The distribution by operative categories was 450 (29.6%) major procedures (Table 3), 889 (58.5%) minor procedures (Table 4) and 181 (11.9%) endoscopic procedures (Table 5). Mortality for major, minor and endoscopic procedures was 6.7%, 7.8% and 7.2% respectively. The causes of death in the different procedure categories are shown in Table 6.
Full table
Full table

Full table

Full table
Full table
Procedures
Major procedures [450]
Lung surgery [106]: procedures performed were decortication in 52 patients (49.1%), lobectomy in 31 patients (29.3%), bullectomy in 9 patients (8.5%), pneumonectomy in 8 patients (7.6%) and wedge resection in 6 patients (5.7%).
Decortication was performed for chronic empyema.
Lobectomy was performed for lung cancer in 20 patients (64.5%), suppurative lung disease in 8 patients (25.8%), congenital cystic adenomatous malformation in 2 patients (6.5%) and penetrating chest trauma in 1 patient (3.3%).
Bullectomy was performed for bullous lung disease in eight patients (88.9%) and thoracic endometriosis in one patient (11.1%).
Pneumonectomy was performed for suppurative lung disease in four patients (50%), lung cancer in three patients (37.5%) and for destroyed lung in one patient (12.5%).
Wedge excision was performed for penetrating chest trauma in two patients (33.3%), and for blunt chest trauma, interstitial lung disease, lung cancer and suppurative lung disease in 1 patient each respectively (16.7%).
There were three mortalities (2.8%). The causes of death were (I) respiratory failure following bullectomy for bullous lung disease, (II) respiratory failure following pneumonectomy for suppurative lung disease and (III) multiple organ failure following lobectomy for penetrating chest trauma.
Vascular repair [67]: these were performed for peripheral vascular injury in 59 patients (88.1%), leg ischaemia in 4 patients (6%), abdominal aortic aneurysm in 3 patients (4.5%) and Inferior Vena Cava Filter insertion in 1 patient (1.5%). The most frequent operations were for the brachial artery in 20 patients (29.8%), for the femoral artery in 11 patients (16.4%), for the popliteal artery in 5 patients (7.5%) and for the radial artery in 5 patients (7.5%) (Table 7).
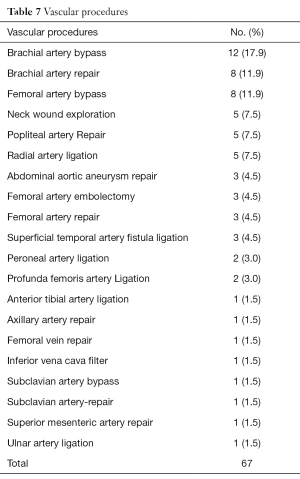
Full table
There were three mortalities (4.5%). The causes of death were (I) exsanguination following rupture of an abdominal aortic aneurysm, (II) postoperative myocardial infarction (MI) following popliteal artery repair in a patient with lower limb ischemia and (III) reperfusion injury and multiple organ failure following brachial artery repair in a patient with upper limb ischemia.
OHS [51]: OHS was introduced in March 2004 and continued till November 2011. A total of 51 cases were performed. There were 21 males (41.2%), mean age was 29±15.6 years and the mean logistic EuroScore was 3.8±2.1. Procedures done were mitral valve replacement in 15 patients (29.4%), ASD repair in 14 patients (27.5%), VSD repair in 8 patients (15.7%), aortic valve replacement in 5 patients (9.8%), atrial myxoma excision in 2 patients (3.9%), Tetralogy of Fallot repair in 2 patients (3.9%) and mitral valve repair in 1 patient (2%).
There were nine mortalities (17.6%). The causes of death and contributory co-morbidity were: (I) right ventricular failure following CABG [recent MI, right ventricular aneurysm, preoperative intra-aortic balloon pump (IABP)]; (II) unable to come off cardiopulmonary bypass (CPB) following VSD repair [patent ductus arteriosus (PDA) missed, circulatory arrest]; (III) right ventricular failure following VSD repair (severe pulmonary hypertension), (IV) right ventricular failure following correction of Tetralogy of Fallot (resection of pulmonary valve and pulmonary regurgitation); (V) renal failure following correction of Tetralogy of Fallot (severe pyrogenic blood transfusion reaction); (VI) cardiac arrest following ASD repair [postoperative supraventricular tachycardia (SVT)]; (VII) unable to wean off CPB following mitral valve replacement (severe pulmonary hypertension and right ventricular failure; (VIII) MI prior to intended mitral valve replacement (unable to achieve cardioplegic arrest); and (IX) unable to come off CPB following atrial myxoma excision (preoperative cardiogenic shock due to obstruction of the mitral valve).
Esophageal surgery [40]: procedures performed were modified Heller’s cardiomyotomy in 21 patients (52.5%), esophagectomy in 10 patients (25%), esophagotomy (for impacted foreign bodies with sharp edges) in 5 patients (12.5%), trachea-esophageal fistula repair in 3 patients (7.5%) and Nissen’s fundoplication in 1 patient (2.5%).
There were four mortalities (10%). The causes of death were (I) mediastinitis following esophagectomy for esophageal cancer, (II) multiple organ failure following esophagectomy for esophageal cancer, (III) malnutrition in a patient who had Heller’s cardiomyotomy for severe achalasia and (IV) respiratory failure following repair of trachea-esophageal fistula.
Miscellaneous procedures [34]: procedures performed were feeding gastrostomy 16 (47.1%), explorative thoracotomy 5 (14.7%), cervical lymph node biopsy 5 (14.7%), open pleural biopsy 5 (14.7%), feeding jejunostomy 2 (5.9%) and thoracotomy for thoracic duct ligation 1 (2.9%). There were four mortalities (11.8%). The cause of death was cancer in all four patients following feeding gastrostomy for oesophageal cancer in two patients, feeding jejunostomy for esophageal cancer in one patient and following open pleural biopsy in one patient with malignant mesothelioma.
Chest wall surgery [31]: procedures done were tumour excision and chest wall reconstruction in 15 patients (48.4%), rib resection in 13 patients (41.9%) and Eloesser window in 3 patients (9.7%).
There were 3 mortalities (9.7%). The causes of death were cancer in 2 patients that had biopsy of chest wall tumours and also cancer in a patient that had Eloesser window for chronic empyema.
Video assisted thoracic surgery [30]: there were 16 males (53.3%) and mean age was 42.5±15.8 years. The procedures performed were lung biopsy in 14 patients (46.7%), pleurodesis in 8 patients (26.7%), bullectomy and pleurodesis in 4 patients (13.3%), pleural biopsy in 3 patients (10%) and excision of bronchogenic cyst in 1 patient (3.3%). There were no mortalities.
Closed heart surgery [25]: there were 10 males (40%) and mean age was 5.8±3.8 years. Procedures performed were PDA ligation in 20 patients (80%) and Blalock-Taussig shunt in 5 patients (20%). There were no mortalities.
Diaphragmatic surgery [25]: there were 19 males (76%) and mean age was 32.8±18.1 years. Diaphragmatic repair was performed for 22 patients (88%) with traumatic diaphragmatic hernias and for 3 patients (12%) with congenital diaphragmatic hernia.
There were two mortalities (8%). The causes of death were multiple organ failure in one patient and sepsis in another patient, both following repair of diaphragmatic hernia following trauma (road traffic accident).
Pericardial surgery [25]: procedures performed were pericardial window in 16 patients (27.6%) and total pericardiectomy in 9 patients (15.5%) There were two mortalities (8%). The causes of death were multiple organ failure in both patients following total pericardiectomy for constrictive pericarditis.
Thymectomy [16]: there were 6 males (37.5%) and mean age was 45.1±16 years. Interestingly, all thymectomies were for thymoma rather than myasthenia gravis. There were no mortalities.
Minor procedures [889]
Chest tube insertion [632]: these were all minor procedures. The distribution by diagnosis was empyema thoracis in 209 patients (33.1%), malignant pleural effusion in 206 patients (32.6%), chest trauma in 171 patients (27%), bullous lung disease in 29 patients (4.6%) and congestive cardiac failure in 17 patients (2.7%).
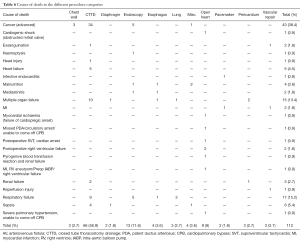
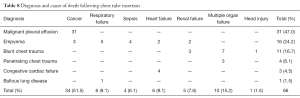
There were 66 mortalities (10.4%). Distribution by diagnosis was malignant pleural effusion 31 (47%), empyema 16 (24.2%), blunt chest trauma 11 (16.7%), congestive cardiac failure 4 (6.1%), penetrating chest trauma 3 (4.5%) and bullous lung disease 1 (1.5%). The causes of death (from associated co-morbidity) are shown in Table 8.
Full table
Arterio-venous fistula surgery [92]: there were 51 males (55.4%) and mean age was 50.1±15.3 years. All operations were done to create hemodialysis access vascular for patients with chronic renal failure. Basilic vein transposition was performed in 22 patients (23.9%) and Cimono fistula in 70 patients (76.1%). There were no mortalities.
Pacemaker implantation [81]: there were 39 males (48.1%). Mean age was 65.5±15.5 years. The indications for pacemaker implantation were complete heart block, second degree heart block and sick sinus syndrome. There were two mortalities. The causes of death were infective endocarditis in 1 patient and MI in the other patient.
Vascular access [51]: These procedures were done to insert subclavian long-term tunneled catheters for vascular access for hemodialysis (referrals from nephrologists). There were no mortalities.
Pericardiocentesis [33]: there was one mortality (3%) from progression of renal failure in a patient with chronic renal failure and massive pericardial effusion.
Endoscopic procedures [181]
Procedures performed were flexible or rigid bronchoscopy in 61 patients (23.7%), rigid or flexible esophagoscopy in 51 patients (28.2%), flexible esophagoscopy and dilatation in 28 patients (15.5%), mediastinoscopy in 35 patients (19.3%) and esophageal stenting (with self-expanding metal stents) in 6 patients (3.3%).
Bronchoscopy was performed for foreign body removal in 38 patients (62.3%), suppurative lung disease in 9 patients (14.8%), lung cancer in 6 patients (9.8%), interstitial lung disease in 4 patients (6.6%) and malignant pleural effusion in 3 patients (4.9%).
Esophagoscopy was performed for foreign body removal in 20 patients (39.2%), oesophageal cancer in 14 patients (27.5%), stricture in 9 patients (17.6%), gastro-oesophageal reflux disease in 5 patients (8.2%) and achalasia in 3 patients (5.9%).
Flexible esophagoscopy and dilatation was performed with over the wire bougies or American bougies for benign esophageal strictures. Esophageal stenting with self-expanding metal stents was reserved for esophageal cancer.
Mediastinoscopy was performed for mediastinal lymphadenopathy in 16 patients (45.7%), lung cancer staging in 13 patients (37.1%) and mediastinal tumour biopsy in 3 patients (8.6%).
There were 13 mortalities (7.2%). The diagnosis was foreign body in the airway in 3 patients, lung cancer in 3 patients, isolated mediastinal lymphadenopathy in 2 patients, suppurative lung disease in 2 patients, esophageal stricture in 1 patient, foreign body in the esophagus in 1 patient and esophageal cancer in 1 patient. The causes of death are shown in Table 6.
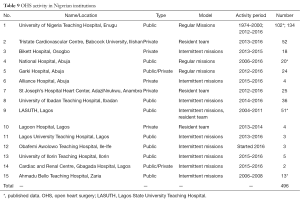
Survey of cardiac activity in other Nigerian institutions
Survey results showed that 496 OHS procedures were performed in 15 different centers between 1974 and 2016. The highest number were at the University of Nigeria Teaching Hospital Enugu with 236 cases (47.9%), Tristate Cardiovascular Centre in Babcock University with 52 cases (10.5%), LASUTH with 51 cases (10.3%), University of Ibadan Teaching Hospital with 36 cases (7.3%) and St Joseph’s Hospital Center with 25 cases (5.1%). Distribution of institution type shows that 8 are public (53.3%), 5 are private (33.3%) and 2 are public/private partnerships (13.3%). The models of practice show that only 4 institutions (26.7%) have resident teams capable of independent practice while 11 institutions (73.3%) rely on cardiac missions, either intermittently or regularly (Table 9).
Full table
Discussion
The distribution of clinical diagnoses seen and the consequent surgical activity at LASUTH closely reflect the fact that cardiothoracic practice in Nigeria still revolves around complications of infection, malignancy and trauma. A study by Aliyu et al. showed 89 major surgeries were performed over a 2-year period (8). The distribution of cases done were thoracotomy for chest trauma (21.4%), decortications for empyema thoracis (15.7%), esophagectomy for corrosive stricture (9.1%), feeding gastrostomy for stricture (6.7%), PDA ligation (6.7%) and bronchotomy for bronchial foreign body (4.5%). This is similar to our practice where the majority of surgery was for infection and trauma. We however have started using esophageal stents rather than feeding gastrostomies and don’t require bronchotomy for foreign body removal as we have a full bronchoscopy armamentarium. In another review of practice, Ekpe et al. reported on 714 procedures over a 5-year period [2008–2013] from Eastern Nigeria with a mean age of 37 years and a male to female ratio of 2:1 (9). The most common diseases seen were acquired and congenital cardiovascular disease (23%), surgical complications of pleuropulmonary tuberculosis (21.4%), thoracic trauma (21%), aerodigestive foreign bodies (10.1%), pyogenic disease (8.7%), esophageal lesions (6.4%), and pulmonary tumours (4.3%). Though they did not report many malignant conditions, the predominance of infective and traumatic disease is similar to the results of our practice in Lagos.
Some procedures practiced in our institution are relatively novel among Nigerian institutions. We have developed a video-assisted thoracic surgery (VATS) practice (10) and mediastinoscopy practice (11). Unfortunately, further development of these practices revolves around appropriate referrals and limited affordability by patients.
Misauno et al. reported on chest trauma seen in Jos Nigeria between 1999 and 2005 (12). There were 189 pts. Mean age was 34 years with a male to female ratio of 5:1. Blunt trauma was seen in 72.2% of the cases and penetrating chest trauma in 27.8%. Mortality was 4.5%. Thomas et al reported on 896 patients with chest trauma over a 10-year period in Lagos (13). Male to female ratio was higher at 8:1. Mean age in the series was 27 years. 82.4% required only tube thoracostomy, conservative treatment in 9.8%, and thoracotomy in 7.5% and median sternotomy in 0.3%. Mortality in the series was 1.2%. The male predominance in trauma cases seen and the high proportion that only required tube thoracostomy is similar to our findings.
There are few reported series on pacemaker implantation in Nigeria. This is a slowly evolving practice, mainly due to the cost of pacemaker implantation (14) and limited expertise (15). Both single and dual chamber implantation is performed. As the cost of pacemaker implantation reduces we are likely to see an increase in this practice.
Various reports from Nigeria have shown that there is a large burden of upper aerodigestive tract foreign bodies that presents as emergencies (16,17) and the necessary equipment is not always available, necessitating invasive procedures like tracheostomy to establish an airway (16) and bronchotomy or esophagotomy to remove the foreign body (8,9). Fortunately, as our center has been able to invest in a full range of flexible and rigid scopes we apply endoscopy for the successful removal of most foreign bodies (17).
Adeoye et al. reported on peripheral vascular procedures in Ilorin over a 2-year period (18). 14 procedures were done with a mean age of 24. The male to female ratio was 2.5:1, the aetiology was trauma in 73% and the upper limb was involved in 63.6%. This is similar to our experience where the majority of vascular repairs were also in the upper limb and there was a male predominance in vascular injury.
Ezemba et al. from Enugu reviewed 51 cases of lung cancer seen over a 2-year period (19). Mean age was 56 years with a male to female ratio of 2.4:1. Half the patients presented with malignant pleural effusion. 10% were stage 3A, 70% stage 3B and 20% Stage 4. They performed exploratory thoracotomy in 12% of the patients and pneumonectomy in 2% of the patients. Thomas et al. also reported a larger series on lung cancer (20). Two hundred and sixty patients were seen between 1999 and 2007. There were 73.8% of the patients who were in the age of 50–69 years with a male to female ratio of 1.2:1. Sixty-nine percent were stage 4 and 92% of these presented with malignant pleural effusion. Curative surgery was only possible in 13.1% of patients seen. Unfortunately, lung cancer tends to present late in Nigeria with the majority presenting as malignant pleural effusion, as in our series, at which stage palliative chest tube drainage and pleurodesis is the only option. In our series 223 patients (14.7%) presented with malignant pleural effusions and 32.6% of chest drain insertions were for malignant pleural effusions. There were no exploratory thoracotomies for lung cancer in our series as complete workup and staging is possible, including mediastinoscopy and flexible or rigid bronchoscopy (11,17).
Corrosive oesophageal stricture tends to be the main indication for esophagectomy in most Nigeria series (21,22). This is thought to be related to late presentation of oesophageal carcinoma and feeding gastrostomies are commonly placed in most Nigerian institutions to enable parenteral nutrition, but do not palliate dysphagia. We prefer esophageal stenting with self-expanding metal stents as it allows patients oral intake.
Achalasia tends to be quite rare in Nigeria. Ahmed et al. in Zaria Nigeria reviewed their experience over a 15 year period between 1991 and 2006 (23). There were 47 patients and 66% were male with mean age of 34.6 years. Ezemba in Enugu Nigeria also reviewed a 15-year period [1990–2004] (24). They reported 43 patients with a mean age of 37 years and male to female ratio of 1:1. We treated 21 patients over the 11-year period of this study.
Our OHS activity has previously been reported (3,4). Fifty-one cases were done between 2004 and 2011 initially as part of cardiac missions and later by the resident team. The program was suspended in 2011 due to increasing difficulties with manpower, equipment, laboratory support, electrical power support and sustainable funding. These issues have now been addressed by our institution and activity is due to recommence later in 2016.
OHS activity in Nigeria is summarized in Table 9. It has been reported that there is an immense backlog of rheumatic valvular heart disease and congenital heart disease in emerging economies (25,26) as well as a rising prevalence of coronary artery disease as more facilities to accurately investigate ischemic heart disease are established (27-29).
It is striking to note the different types of institutions practicing OHS and the different models to deliver the practice. There has been a recent surge in OHS activity with 66.5% of the cases done in Nigeria occurring in the last 4 years [2012–2016]. This has largely been driven by increased cardiac missions and private sector participation. 7 of the 15 institutions with OHS activity (46.7%) are private or public/private partnerships. Eleven institutions (73.3%) are currently building their programs with cardiac missions. Cardiac missions have been taking place in Nigeria since 1974; despite this no institution has evolved into a regular sustainable practice (1,2). This shows that cardiac missions may take a long time to transfer skill (30). It has been proposed that different models are at play in Africa in setting up cardiac centers (31). Model 1 is where a senior local surgeon is able to set up a center as was successfully done in Ghana (32). Model 2 is that of surgeons visiting for short times to perform humanitarian surgery. This is the model currently being applied in most of the Nigerian centers but it has been shown to have a very long lead time in successful skills transfer. A third model less frequently practiced is one where expatriate surgeons are employed on contract to develop a cardiac program as was successfully done at the Agha Khan Hospital in Nairobi, Kenya. Our institution has largely practiced model 2 (cardiac missions) with limited success. We are currently working on making the transition to model 1 with a senior local surgeon to drive the program.
Limited attention has been paid to manpower capacity building. Cardiac missions introduce new skills and resources which impact positively but for a limited period. It has been shown in Nigeria that unless investment is made in local surgical manpower training and support cardiac activity cannot be sustained by cardiac missions (3-5,30). A cardiac mission provides hands on practical experience for the local team but building local capacity must be a long term strategy while could be boosted by private sector participation (4).
The Nigerian population is conservatively estimated as 173 million people (33) and can therefore eventually support several cardiac centers. At this early stage in development it would be better if efforts could be amalgamated and consolidated to have fewer centers and pool patients, expertise and funding to those few centers. The funding and political nuances of each local center however often militate against a collaborative approach. More efforts need to be made to improve manpower requirements, streamline purchase of specialized consumables to drive down prices and increase referrals between centers. Collaborative efforts between some centers and some surgeons has started and needs to be encouraged to take place on a national level to better yield dividends, otherwise the loss to medical tourism will continue unabated.
We have described above a wide range of procedures practiced in our institution, some of which are not available in some other Nigerian institutions. General thoracic surgery, vascular surgery, closed heart surgery and OHS have all been established and practiced. Routine use of staplers, double lumen tubes for one lung ventilation, mediastinoscopy, and oesophageal stenting has been developed (11,34). Endoscopy for therapeutic and diagnostic purposes is available (17). VATS is being practiced (10). However, the Achilles’ heel of our practice, which is a common denominator to varying extents in different Nigerian cardiothoracic centers, is the low surgical volumes. The highest number of procedures done in any year was 2013 with 235 procedures. However, 46% of the activity was related to chest tube insertion for empyema, malignant pleural effusions and chest trauma. Considerably more minor than major surgery is performed, largely due to economic constraints. Though these are important interventions for the patients involved, this causes many cardiothoracic practices in Nigeria to be viewed unfavourably as “mere chest drain services”, especially if other practices as described above are not available which is the case in many institutions.
What are the major limitations to having more major surgical activity? In our institution trained surgical and nursing manpower has been developed, infrastructure is largely available or being upgraded and we are able to source all our consumables locally to a large extent. Strenuous efforts have been made to ensure surgery is accessible and affordable but the health care provision in Nigeria is largely unfunded by the Government. Higher end operations like OHS are naturally the most affected (35) and this greatly limits the numbers of these procedures (3-5). There is a poorly developed funding structure available and the vast majority of patients are self-funding. This severely restricts the numbers of procedures that are performed. This is extremely worrying, as it impacts on institutions’ ability to train residents. This has led to no cardiothoracic program in the country having full accreditation for training and the West African College mandating that trainees must spend time in high volume centers abroad to fulfil their training requirements. A vicious cycle is however created as these trainees return to centers with low volumes and become deskilled in procedures performed infrequently. The same of course applies to their trainers. Infrequently performed procedures cannot be performed safely with resultant loss of public confidence and increased loss to medical tourism (3). This is a situation which requires urgent remedy. Funding structures for surgery need to be in place which may require a combination of Government, Non-governmental organizations, charitable bodies, and robust insurance schemes (4,6).
There are several lessons to be gleaned from examination of the causes of death in our series (Table 6). The most common causes of death overall were cancer (38.4%), multiple organ failure (13.4%), respiratory failure (15.2%), sepsis (5.4%), heart failure (4.5%) and malnutrition (3.6%). The most common procedure of chest tube insertion had a 30-day mortality of 10.4%. Half of these mortalities had advanced cancer, a quarter had empyema with severe sepsis, those with chest trauma either had severe polytrauma or delayed presentations and some patients had end stage heart failure. The success of cardiothoracic practice is dependent on early referrals (so patients are being operated on with early rather than late disease) and adequate support systems which are often taken as the norm in more developed countries but require hard work and commitment to put in place in Nigeria. Many patients present with advanced cancer which is often the cause of death. Late presentation also contributed to respiratory failure, sepsis, heart failure and malnutrition as causes of death; this is often a balance between patients’ belief in traditional medicine and seeking orthodox medicine late in the course of their disease but at times small private hospitals with limited resources delay patient referral to maximize profit. Problems with availability of ICU support, functioning equipment in ICU and even availability of oxygen on occasion have been contributory to reducing the number of major procedures done due to concerns about the postoperative support which could affect the outcome negatively. This has often led to many potential major cases ending up in larger and better equipped private hospitals or going abroad. Other problems encountered at different periods were problems with availability of blood in the hospital blood bank which lead to the use of blood from outside laboratories with a higher risk of blood transfusion reactions, limited facilities for renal support, variable electrical power supply which lead to interruption of postoperative ventilator support. Limitation of supply of consumables, at the time, is highlighted by the OHS case where cardioplegic arrest was difficult due to non-availability of appropriate coronary perfusion catheters. Misdiagnosis due to low resolution echocardiography facilities led to missing a PDA preoperatively and resulted in a straightforward VSD repair requiring unplanned circulatory arrest for adequate visualization with subsequent myocardial ischemia and negative operative outcome.
Many of the challenges highlighted above have previously been discussed (3) and addressed by our institution and are now of historical interest only. However, some are outstanding and remain a work in progress, in our institution and others in Nigeria.
Prof Adebonojo’s monogram on the development of OHS in West Africa clearly highlights these problems (36). He asks, “Why did Heart Programmes in Nigeria fail”? He explains that the heavy financial outlay, intensive labor, high resource consumption and depressed economy and fragile and unstable Government were contributory factors. …disorganized planning, decentralization of efforts, lack of national health statistics, national health insurance scheme, national planning, medical, surgical and nursing manpower...” He also mentions that…”. The frequent equipment breakdown and the poor maintenance culture continue to be major problems. The lack of autonomy from hospital management and government interference with heavy reliance on external support will continue to be our Achilles’ heel”…Sadly this situation he described still remains the same, especially in the public sector in Nigeria.
A recent survey of Cardiothoracic Surgeons and Residents on the challenges being encountered in establishing Pediatric Cardiac Centers in Nigeria was conducted (6). Nearly all children requiring Cardiac intervention are currently referred abroad. The dearth of pediatric cardiac surgical centers in Nigeria was attributed to a weak health system, absence of skilled manpower, funds and equipment. These are unfortunately now very familiar refrains.
Few cardiothoracic publications from Nigeria make mention of outcomes of surgical procedures (3-5). This requires accurate data, if possible risk stratified. We have been able to do this in our institution by developing in-house databases which can calculate risk stratification. The average logistic EuroScore of the OHS cases done at the LASUTH was 3.8±2.1 with an observed mortality of 17.6% (3) while that of the cases done in Northern Nigeria between 2006−2008 was 5 with a mortality of 12.5% (5). Early publications on OHS activity in Nigeria make no mention of risk score or outcomes of the procedures (1,2). Now that OHS has begun to take root in Nigeria it is vital to find a mechanism to collate regional and national statistics on OHS activity and outcomes as this will guide the development of evidence-based practice. At this early stage, Microsoft Access databases which come with Microsoft Office could be a good option as practiced in our institution where all activity is inputted on the database and was the source of data for this article. Large databases as maintained by the American Society for Thoracic Surgery and the European Association for Cardiothoracic Surgery allow data collection which is required as a benchmark to achieve quality control. Data collection is a gradual process which should not penalize or hinder the developing, struggling or emerging cardiac programs (37). “South Africa has developed a national database… to keep pace with international developments in cardiothoracic surgery… and meet the growing demand for service from the profession and the public by having an increased evidence base to guide clinical decision making” (38). A similar national database is crucial to further the development of sustainable and affordable cardiac surgery in Nigeria. Without data, stakeholders cannot invest in the development of cardiac programs.
Conclusions
Surgery for infection, malignancy and trauma still make up the bulk of cardiothoracic practice in Nigeria with surgical activity showing a predominance of minor procedures and comparatively minimal OHS activities. Identified challenges to increasing cardiothoracic surgical activity are limitations in manpower development, infrastructure, laboratory support, local availability of consumables, cost of surgery, funding mechanisms for surgery, multiple models for development of cardiac surgery, decentralization of efforts and lack of outcome data. Operating a revolving fund model as we do may militate against some of these challenges. These challenges result in low surgical volumes which has a significant knock-on effect on services and training. It is encouraging to see the recent surge in OHS activity but we need to transit from cardiac missions and cardiothoracic practice needs to more collaborative and less decentralized to accelerate this growth and improve outcomes. Data collection and reporting of results must be encouraged to enable development of more evidence-based practice.
Acknowledgements
We are grateful for the contributions of the members of the cardiothoracic team in the Lagos State University Teaching Hospital (LASUTH) without whom the work on which this paper is based would not have been possible. We also wish to acknowledge the financial support of the Lagos State Government who have funded the cardiothoracic division and enabled the activity described. We are grateful to all the Nigerian cardiothoracic surgeons who responded positively to our requests for information about the current status of OHS in their institutions.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Ethics Committee of the Lagos State University Teaching Hospital (LASUTH) and there was no patient contact for the study so informed consent was not required.
References
- Anyanwu CH, Ihenancho HN, Okoroma EO, et al. Initial experience with Open Heart Surgery in Nigeria. Trop Cardiol 1982;8:123-7.
- Eze JC, Ezemba N. Open-heart surgery in Nigeria: indications and challenges. Tex Heart Inst J 2007;34:8-10. [PubMed]
- Falase B, Sanusi M, Majekodunmi A, et al. Open heart surgery in Nigeria; a work in progress. J Cardiothorac Surg 2013;8:6. [Crossref] [PubMed]
- Nwiloh JO, Oludara MA, Adebola PA. Heart Surgery Practice in Sub Saharan Africa: Single Nigerian Institutional Midterm Results and Challenges. WJCS 2014;4:35-41. [Crossref]
- Nwiloh J, Edaigbini S, Danbauchi S, et al. Cardiac surgical experience in northern Nigeria. Cardiovasc J Afr 2012;23:432-4. [Crossref] [PubMed]
- Okonta KE, Tobin-West CI. Challenges with the establishment of congenital cardiac surgery centers in Nigeria: survey of cardiothoracic surgeons and residents. J Surg Res 2016;202:177-81. [Crossref] [PubMed]
- Lagos population 2016. Available online: http://worldpopulationreview.com/world-cities/lagos-population, accessed 10th May 2016.
- Aliyu I, Inuwa IM. Common indications for major cardiothoracic surgeries in Aminu Kano Teaching Hospital, Kano, Nigeria: A 2-year review. J Med Tropics 2015;17:27-9. [Crossref]
- Ekpe EE, Ette VF, Akpan A. Pattern of cardiothoracic surgical diseases in a new cardiothoracic surgery unit in Nigeria. Niger J Med 2014;23:77-82. [PubMed]
- Falase BA, Majekodunmi AA, Ismail S, et al. Video-assisted thoracic surgery in a Nigerian teaching hospital: Experience and challenges. Niger J Clin Pract 2016;19:233-6. [Crossref] [PubMed]
- Falase B, Ogadinma M, Majekodunmi A, et al. The role of cervical mediastinoscopy in Nigerian thoracic surgical practice. Pan Afr Med J 2016;24:135. [Crossref] [PubMed]
- Misauno MA, Sule AZ, Nwadiaro HC, et al. Severe chest trauma in Jos, Nigeria: pattern and outcomes of management. NJOT 2007;6:64-6.
- Thomas MO, Ogunleye EO. Etiopathology and management challenges of blunt chest trauma in Nigeria. Asian Cardiovasc Thorac Ann 2009;17:608-11. [Crossref] [PubMed]
- Thomas MO. Cost issues in pacemaker surgery in Nigeria. NQJHM 2004;14:140-2.
- Falase B, Sanusi M, Johnson A, et al. Analysis of a five year experience of permanent pacemaker implantation at a Nigerian Teaching Hospital: need for a national database. Pan Afr Med J 2013;16:16. [Crossref] [PubMed]
- Onotai LO, Ibekwe MU. A survey of upper aerodigestive tract emergencies seen in a Nigerian Tertiary Teaching Hospital. Int J Med Med Sci 2012;2:092-6.
- Falase B, Sanusi M, Majekodunmi A, et al. Preliminary experience in the management of tracheobronchial foreign bodies in Lagos, Nigeria. Pan Afr Med J 2013;15:31. [Crossref] [PubMed]
- Adeoye PO, Adebola SO, Adesiyun OA, et al. Peripheral vascular surgical procedures in Ilorin, Nigeria: indications and outcome. Afr Health Sci 2011;11:433-7. [PubMed]
- Ezemba N, Ekpe EE, Eze JC. Challenges of lung cancer management in a developing country. Niger J Med 2012;21:214-7. [PubMed]
- Thomas MO. Aetiopathology and management challenges of Lung Cancer in developing world. East Afr Med J 2011;88:40-3.
- Thomas MO, Ogunleye EO, Somefun O. Chemical injuries of the oesophagus:aetiopathological issues in Nigeria. Journal of Cardiothoracic Surgery 2009;4:56. [Crossref] [PubMed]
- Thomas MO, Ogunleye EO, Somefun O. Chemical injuries of the oesophagus: aetiopathological issues in Nigeria. J Cardiothorac Surg 2009;4:56. [Crossref] [PubMed]
- Ahmed A, Yusufu LM, Ukwenya YA, et al. Surgical management of achalasia in Zaria, Northern Nigeria. S Afr J Surg 2008;46:48-51. [PubMed]
- Ezemba N, Ekwunife CN, Eze JC. Achalasia in Nigeria. Current status. Chirugia 2007;20:125-9.
- Pezella TA. Global Expansion of Cardiac Surgery in the New Millennium. Asian Cardiovasc Thorac Ann 2001;9:253-6. [Crossref]
- Mocumbi AO. The challenges of cardiac surgery for African children. Cardiovasc J Afr 2012;23:165-7. [Crossref] [PubMed]
- Nwaneli CU. Changing trend in coronary heart disease in Nigeria. Afrimedic J 2010;1:1-4.
- Johnson A, Falase B, Ajose I, et al. A cross-sectional study of stand-alone percutaneous coronary intervention in a Nigerian Cardiac Catheterization Laboratory. BMC Cardiovasc Disord 2014;14:8. [Crossref] [PubMed]
- Falase B, Johnson A, Animasahun A, et al. Clinical and angiographic profile of Nigerians with coronary artery disease. Exp Clin Cardiol 2014;20:398-410.
- McKavanagh P, Booth K, Blair L, et al. Addressing discrepancies: personal experience of a cardiac mission programme in Africa. Int J Cardiol 2014;177:794-9. [Crossref] [PubMed]
- Yankah C, Fynn-Thompson F, Antunes M, et al. Cardiac surgery capacity in sub-saharan Africa: quo vadis? Thorac Cardiovasc Surg 2014;62:393-401. [Crossref] [PubMed]
- Edwin F, Tettey M, Aniteye E, et al. The development of cardiac surgery in West Africa--the case of Ghana. Pan Afr Med J 2011;9:15. [Crossref] [PubMed]
- Nigeria overview. Available online: http://www.worldbank.org/en/country/nigeria/overview, accessed 10th May 2016.
- Majekodunmi AA, Falase BA, Udom BO, et al. One lung ventilation using double-lumen tubes: Initial experience from Lagos, Nigeria. Niger J Clin Pract 2015;18:227-30. [Crossref] [PubMed]
- Falase B, Sanusi M, Majekodunmi A, et al. The cost of open heart surgery in Nigeria. Pan Afr Med J 2013;14:61. [PubMed]
- Adebonojo SA. Open Heart Surgery in Nigeria. In: Adebonojo SA, editor. Development of Open Heart Surgery in West Africa: a historical perspective. Eruwa: Acecool Medical Publishers Nigeria, 2008:21-36.
- Pezzella AT. Open heart surgery in a developing country. Asian Cardiovasc Thorac Ann 2006;14:355-6. [Crossref] [PubMed]
- Linegar A, Smit F, Stroebel A, et al. A South African national database in cardiothoracic surgery. Cardiovasc J Afr 2010;21:153-4. [PubMed]