Incidence and interventions for post-thrombotic syndrome
Introduction
Post-thrombotic syndrome (PTS) has the highest clinical significance as a long-term sequela of deep venous thrombosis (DVT). PTS is associated with high morbidity and decreased quality of life for affected patients. Patients with PTS present with edema, chronic leg pain, swelling, skin changes, and heaviness of the limb previously affected by DVT (1,2). The symptoms from PTS result from impaired venous blood return secondary to damaged venous valves and obstructive disease caused by a prior DVT event.
The annual incidence of venous thromboembolism is estimated at 1/1,000 persons per year (3) and studies have shown that 20% to 50% of these patients develop PTS as a long-term sequela (3). Severe manifestations of PTS include development of venous ulcer disease (2,4,5). Venous ulcer management in PTS patients is challenging. One long-term follow-up study demonstrated 5% of PTS patients during a 10-year course develop venous ulcers (5). Moreover, it is important to emphasize that PTS does not solely affect the adult population. The incidence of PTS in children after upper and lower extremity DVT has been reported as high as 26% (6,7). PTS treatment in the pediatric population is based upon guidelines in the adult population which are discussed below (8).
The deceased quality of life and productivity that PTS inflicts on patients overall health causes a significant cost to the healthcare system. In the United States, the average annual cost of treating a patient with PTS is estimated at $7,000 per patient per year (9). Regarding the loss of productivity, one paper estimated that venous ulcer complications result cumulatively in 2 million lost workdays in the United States annually (10). Another more recent manuscript focused on the relationship between chronic diseases and quality of life, concluding that PTS has a more significant impact on decreased quality of life compared to osteoarthritis, chronic lung disease, and/or angina (11).
Pathophysiology
Patients with acute DVT are usually treated with an anticoagulation regimen. The overall goal of this treatment approach is to prevent further extension of the DVT and to prevent new thrombus formation. Studies are suggesting that anticoagulation in DVT may partially but not completely resolve the entire thrombotic burden (12,13). The residual thrombus burden puts the patient at risk for PTS as a long-term sequela of DVT.
There are three proposed pathophysiologic pathways from development of acute DVT to PTS as a chronic disease. In the majority of cases, all 3 pathways contribute in different extent to the development of PTS. The first mechanism relates to direct damage to venous valves by the thrombus formation in acute DVT. The second mechanism relates to indirect damage to venous valves through inflammatory mediators. Shbaklo et al. showed that certain cytokines and adhesion molecules such as intercellular adhesion molecule-1 and interleukin-6 were associated with the development of PTS after a prior DVT (14). The third mechanism relates to the thrombus burden in acute DVT or residual burden post anticoagulation treatment since the thrombotic burden leads to venous outflow obstruction. These three processes ultimately result in valvular reflux, venous hypertension, and impaired venous blood flow return. The increased venous hypertension is associated with increased tissue permeability with the consequence of edema formation and subsequently with reduced arterial blood supply to the skeletal musculature of the affected limb. These mechanisms explain the clinical symptoms of PTS including edema, limb pain, swelling, skin changes, and heaviness of the affected limb (15). Visualized skin discoloration or pigmentation of the affected extremity on physical exam is related to breakdown of red blood cells which have leaked out of the venous system (16).
Based on the pathophysiology of the disease prompt, safe and effective clearance of the entire thrombotic burden is recommended to help to prevent PTS. During the treatment of acute DVT provocation of inflammatory responses and scarring should be minimized since these processes can lead to damaged venous valves, eventually increasing the risk of future PTS (17).
Risk factors
There are several known risk factors for developing PTS after acute DVT. Some suggested risk factors include age, sex, body mass index (BMI), thrombophilia, characteristics of initial venous thromboembolism, recurrent DVT episodes, residual thrombosis on ultrasound, and intensity/effectiveness/duration of the oral anticoagulation regimen.
Age has been evaluated as a potential risk factor for PTS; however, studies thus far have been inconclusive. Some investigations showed that there was an association between increasing age and higher risk of PTS (18,19) whereas other studies could not confirm this (1,19).
Obesity is a well-established risk factor for PTS. A study by Ageno et al. showed that patients with a higher BMI with symptomatic proximal DVT were more likely to develop PTS during a 12-month follow up interval (20).
Inherited or acquired thrombophilia disorders increase the risk of DVT and recurrent DVT; however, there is insufficient evidence to suggest an association between inherited or acquired thrombophilia and an increased risk of PTS as a sequela of prior DVT (1,19).
Studies demonstrated a relationship between location of the primary DVT and subsequent PTS development. Investigations have shown that up to 20–80% of patients were diagnosed with PTS after a distal calf DVT (21,22).
Subtherapeutic anticoagulation is another known risk factor. Several studies have demonstrated that patients may be at increased risk of developing PTS within weeks to months post DVT secondary to subtherapeutic anticoagulation. Particularly failure to initiate an early and appropriate anticoagulation regimen for DVT can lead to an increased risk for PTS (1).
Residual DVT identified on ultrasound examination after anticoagulation treatment is another risk factor associated with an elevated risk of PTS development (12,13).
Diagnosis
Clinical diagnosis
Diagnosing and recognizing PTS can be challenging since symptomatic presentation varies in individual patients. Presenting symptoms include pain, swelling, edema, heaviness, and skin changes in the affected extremity. The symptoms typically improve at rest while lying flat and with elevation of the affected extremity. The symptoms typically worsen while standing or walking. Other clinical signs include telangiectasia, hyperpigmentation, eczema, varicose veins, ulceration, or lipodermatosclerosis (23). Several clinical scales and surveys have been developed to aid in diagnosing and characterizing PTS. The Villalta scale (24) and Ginsberg measure (25) were created to specifically diagnose PTS after an established episode of acute DVT. Others scales focus primarily on chronic venous disease in general and include the CEAP (Clinical, Etiological, anatomic, and pathophysiological) classification (26), and Venous Clinical Severity Score (VCSS) (27).
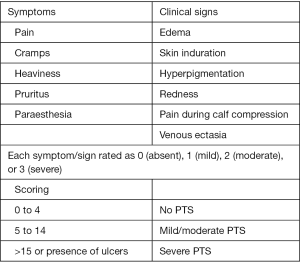
The Villalta scale (Figure 1) is the most widely used and accepted clinical tool for diagnosing, assessing the severity, and evaluating treatment of PTS. The International society of Thrombosis and Hemostasis subcommittee on Control of Anticoagulation has recommended the Villalta scale as the most appropriate measure to diagnose and evaluate PTS (28). The Villalta scale consists of five patient subjective rated categories and 6 clinician objective rated categories that are graded from 0–3 based on severity.
The Ginsberg measure characterizes PTS based on daily leg pain and swelling that lasts for 1 month and occurs at least 6 months after an acute DVT. Although less utilized than the Villalta scale in the clinical arena, the Ginsberg measure may better identify more severe forms of PTS than the Villalta scale (25).
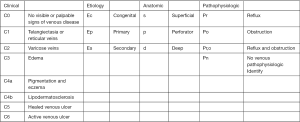
The CEAP classification (Figure 2) was designed to evaluate treatment outcomes for patients with venous diseases. This classification is fairly non-specific for the cause of chronic venous disease. The CEAP classification consists of 7 clinical, 3 etiological, 3 anatomical, and 4 pathophysiological classes. The specific classes are listed in Figure 2. CEAP has been used to diagnose PTS previously; however, several limitations exist which include assessment of disease severity, lack of a universally agreed cutoff for the diagnosis of PTS, and limited ability to follow changing clinical status post treatment in the course of the disease (26).
The VCSS (Figure 3) most recently updated by Vasquez et al., combines factors of compression therapy, number of ulcers, and the CEAP scale to assess venous disease. The VCSS is based on 9 clinical signs and 1 symptom which is pain. The VCSS is well suited for advanced cases of venous disease (27).
Imaging diagnosis
For patients presenting with PTS, the first imaging test of choice to evaluate for thrombus or valvular reflux is duplex ultrasound of the affected extremity. The advantage of duplex US is that the exam is inexpensive and non-invasive. If the duplex US is inconclusive or additional anatomical information is required, CT or MR venography can be performed to evaluate for venous collaterals, masses that may cause extrinsic compression of veins, and venous asymmetries. If the above imaging modalities are inconclusive and the high clinical suspicion for PTS remains, intravascular ultrasound (IVUS) can be performed for further evaluation. IVUS can demonstrate intraluminal and mural details and echogenicity of any thrombus which can help for determining the age of the thrombus. However, IVUS is an invasive procedure that requires a 9 F sheath and should be reserved for cases in which other imaging modalities have be inconclusive. Percutaneous transfemoral or transpopliteal venography is the gold standard for evaluating for venous stenosis/occlusions. However, transfemoral or transpopliteal venography should be reserved for PTS cases in which endovascular intervention is planned.
Prevention of PTS
There are several preventive measures to avoid PTS. Prevention of the initial DVT if possible would be ideal and therefore, the use of pharmacologic or mechanical thromboprophylaxis in patients at risk for DVT is encouraged. If a patient already had a DVT event, prevention of a recurrent DVT is highly recommended since a recurrent ipsilateral DVT is a significant risk factor for the development of PTS (29). Frequent follow-up post initial acute DVT event is crucial to avoid subtherapeutic anticoagulation. Anticoagulation treatment for DVT has been shown to be most effective in the first 3 months following the initial presentation (29). Delayed anticoagulation therapy later than 3 months has been shown to increase the risk of PTS development (29).
Non-pharmacologic methods such as elastic compression stockings (ECS) have been studied. The theory behind ECS is that compression from the stockings would help return venous blood. Multiple studies have been performed on the effectiveness of ECS post-acute DVT for PTS prevention and the results are conflicting. One multicenter, randomized-controlled trial did not demonstrate any significant benefit for prevention of PTS in patients with a central DVT after 2 years of wearing active compression stockings (30). However, there have been at least two studies that supported wearing 30–40 mmHg knee-high ECS for PTS prevention in patients with proximal DVT (18,31). Therefore, it is reasonable to provide a trial of ECS in patients with proximal acute DVT as a preventive measure for PTS development.
In terms of thrombolytic therapy to prevent PTS, the use of thrombolysis with heparin has been shown to improve patency rates following acute DVT (32). Systematic thrombolytic therapy can be used. However catheter directed thrombolysis (CDT) with or without mechanical disruption (pharmacomechanical thrombolysis) of the thrombus in selected patients can be a safer approach with less systemic side-effects as opposed to systemic thrombolysis (33). Prompt clearance of thrombus burden in DVT decreases the risk of subsequent PTS, as it opens the vein, relieving venous outflow obstruction immediately, maintaining valvular function, and preventing venous hypertension. CDT or pharmacomechanical catheter directed thrombolysis (PCDT) has a decreased risk of systemic side effects (34). Current recommendations state that CDT and PCDT may be considered in a selected patient with acute (<14 days) symptomatic DVT, extensive proximal DVT with good functional capacity, >1 year life expectancy, and low expected bleeding risk (34). Systemic anticoagulation should be used before and after CDT or PCDT. Balloon angioplasty with or without stenting of underlying obstructing lesion after CDT/PCDT may be indicated in a limited subset of patients to prevent recurrent thrombosis. Systemic thrombolysis is not recommended for the treatment of DVT (34). For patients who are not good candidates for CDT/PCDT, surgical thrombectomy may be considered as an alternative (30).
Treatment of PTS
Non-interventional treatment
PTS treatment can be divided into non-interventional and interventional treatment approaches. Conservative non-interventional treatments include compression based therapies, pharmacotherapy, and lifestyle changes. The goal of compression based therapies is to alleviate symptoms. Even though there are only a limited number of controlled studies that have demonstrated the effectiveness of compression therapies, treating patients with compression therapy is still a viable option given the low risk profile of this treatment. A trial of 20–30 mmHg ECS can be attempted. Below the knee ECS have be showed to have similar effectiveness as above the knee ECS. Below the knee ECS are associated with increased patient compliance. If patients remain symptomatic, stronger ECS of 30–40 or even 40–50 mmHg can be tried (34).
Severe cases may require intermittent pneumatic compression sleeve units with 20–30 minutes duration for 2–3 times per day. A randomized control trial by Ginsberg et al. followed patients with severe PTS with intermittent pneumatic compression at 50 mmHg and demonstrated up to 80% improvement in edema over a four week period (35). There are several disadvantages of using intermittent pneumatic compression. First, the pneumatic compression therapy is inconvenient for patients. Patients need to spend several hours a day using the compression device to improve their symptoms. Also, the pneumatic compression devices are expensive. A trial of pneumatic compression therapy may be reasonable in immobile patients with severe PTS and edema who are not ideal candidates for interventional therapies.
Several venoactive drugs have been tried in the past as a pharmacologic therapy for PTS. Such venoactive drugs were rutosides, defibrotide, prostaglandin E2, thrombomodulin, and hidrosmin. Unfortunately, there is limited clinical trial evidence to demonstrate significant improvement of symptoms with these agents. Therefore, these medications are not recommended for treatment per current guidelines. Clinical trials proving effectiveness of these medications is needed in the future (36).
Several studies have shown that exercise with leg strengthening can help treat PTS. Patients benefit from exercise and leg strengthening by promoting venous blood return and initiating weight loss. A study by Padberg et al. demonstrated that 30 patients who completed a 6-month exercise program focused to increase leg strength showed improvement in PTS symptoms (37).
Endovascular treatment of PTS
For a select number of patients with PTS, endovascular or surgical management can be performed to improve symptoms. Endovascular options include angioplasty and stent placement. Surgical options include various venous bypass surgeries based on the location of the DVT. If patients with PTS suffer from chronic superficial venous reflux, venous stripping, foam sclerotherapy, or radiofrequency/laser ablation are surgical options for superficial venous reflux. Valvuloplasty is a surgical option for intact but incompetent venous valves. If the venous valves are completely destroyed, autotransplantion of the axillary vein is another surgical option (38). For purposes of this paper, more focus will be placed on endovascular management of PTS based on the authors’ institutional experience.
PTS patients who score >3 on the CEAP classification and failed conservative management are considered candidates for endovascular management. Patients with CEAP scores of 2 or less can be considered candidates for endovascular management if they have significant pain associated with their PTS (39,40).
Typically, local anesthesia and moderate sedation is sufficient for angioplasty and stenting of post-thrombotic venous occlusion disease. The two main approaches to angioplasty and stenting of Iliofemoral stenosis or occlusion from prior DVT include an ipsilateral transfemoral approach while the patient is in a supine position or an ipsilateral transpopliteal approach while the patient is in a prone position. If the thrombus extends into the IVC, a jugular vein approach can be considered. In addition, if the patient has an IVC filter in place, removal should be considered prior to angioplasty and stenting. Once access is gained into the vein, a venogram is performed to determine the amount of stenosis or occlusion. Greater than 60% stenosis is considered hemodynamically significant (41). Stiff Guidewires in conjunction with supporting catheters are advanced until the lesion of interest is completely crossed. Angioplasty is then performed to dilate the lesion prior to stenting. To prevent stent migration within Iliofemoral veins, the stent should extend 3–4 cm into the IVC. The 12–16 mm WallStents (Boston Scientific) are sufficient for Iliofemoral stenting while larger 18–24 mm Wallstents (Boston Scientific) are used for Iliocaval stenting (41). If stents have to be overlapped, 2 cm should be sufficient overlap of the stents to prevent detachment. After all the stents are deployed, repeat angioplasty should be performed. In addition, a post-stent venogram should be performed to demonstrate increased venous flow and improvement of the stenosis. (41).
Intra-procedural and post-stenting anti-coagulation
Intra-procedural IV heparin is administered during iliofemoral and iliocaval angioplasty and stenting procedures. There are differing approaches with anticoagulation post-stenting. Some physicians will treat with 6 months of coumadin while others will start antiplatelet medications such as aspirin and Plavix. Patients with unexplained DVT should be worked-up for coagulopathies (42).
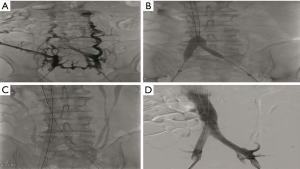
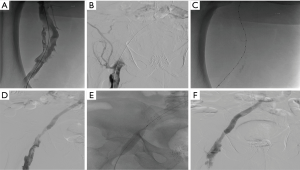
The following two cases in which endovascular management of proximal DVT was treated with a combination angioplasty, PCDT, and/or stenting based on our institutional experience. Case #1 is a 58-year-old male with chronic thrombosis of the infrarenal IVC and bilateral common and external iliac veins with CEAP classification of C3EsAdPo. Despite compression stockings and exercise therapy for 3 months, the patient still had persistent lower extremity pitting edema, and discoloration of feet and ankle with significant discomfort. Endovascular management of this patient is shown in Figure 4. Case #2 involves a 73-year-old male with left lower extremity DVT thrombosis of 5 weeks duration and CEAP of C3-4a/Es/Ad/Po. The patient underwent angioplasty, PCDT, and stenting (Figure 5).
Outcomes of Iliocaval and Iliofemoral stent placement for PTS
Several studies have been conducted to assess the patency rates and effectiveness of endovascular management of post-thrombotic venous occlusion disease. Primary patency rates following stenting of post-thrombotic occlusion have varied from 61–83% (43,44). In a study by Rosales et al., 34 patients with post-thrombotic symptoms following DVT underwent stenting for iliocaval or iliofemoral occlusion and chronic venous insufficiency. Two-year primary patency rate was 67%. With those who were successfully recanalized (94%) symptoms of edema and venous claudication resolved. Further, 4 out 7 ulcers that were document from the 34 patients healed (45). In a study by Raju et al., balloon dilatation and stent placement for iliac vein stenosis was performed in 304 symptomatic limbs. The results of this study included primary and secondary patency rates of 71% and 90% at 24 months. In addition, the ulcer healing rate was 62% at 24 months (46). Endovascular stenting for treating venous claudication, edema, and venous ulcer formation cause by post-thrombotic venous occlusion has demonstrated good patency rates and improvement of symptoms.
Conclusions
PTS is a complication of DVT which is associated with significant morbidity and decreased quality of life. PTS has a marked burden on the healthcare system. For diagnosis of PTS several measures have been created including the Villalta scale, Ginsberg measure, CEAP, and VCSS to help physicians diagnose the disease. Appropriate therapeutic anticoagulation status post DVT is of utmost importance to prevent PTS development. In addition, non-invasive measures for preventing and treating PTS include ECS, exercise, anti-coagulation, and pneumatic compression (34). Endovascular management of PTS includes angioplasty and stenting which has shown promising results for improving patency and resolving symptoms (34).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kahn SR, Kearon C, Julian JA, et al. Predictors of the post-thrombotic syndrome during long-term treatment of proximal deep vein thrombosis. J Thromb Haemost 2005;3:718-23. [Crossref] [PubMed]
- Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 1996;125:1-7. [Crossref] [PubMed]
- Silverstein MD, Heit JA, Mohr DN, et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med 1998;158:585-93. [Crossref] [PubMed]
- Kahn SR, Shrier I, Julian JA, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med 2008;149:698-707. [Crossref] [PubMed]
- Schulman S, Lindmarker P, Holmström M, et al. Post-thrombotic syndrome, recurrence, and death 10 years after the first episode of venous thromboembolism treated with warfarin for 6 weeks or 6 months. J Thromb Haemost 2006;4:734-42. [Crossref] [PubMed]
- Goldenberg NA, Donadini MP, Kahn SR, et al. Post-thrombotic syndrome in children: a systematic review of frequency of occurrence, validity of outcome measures, and prognostic factors. Haematologica 2010;95:1952-9. [Crossref] [PubMed]
- Monagle P, Chan AK, Goldenberg NA, et al. Antithrombotic therapy in neonates and children: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e737S-801S.
- Barnes C, Newall F, Monagle P. Post-thrombotic syndrome. Arch Dis Child 2002;86:212-4. [Crossref] [PubMed]
- MacDougall DA, Feliu AL, Boccuzzi SJ, et al. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm 2006;63:S5-15. [Crossref] [PubMed]
- Bergan JJ, Schmid-Schönbein GW, Smith PD, et al. Chronic venous disease. N Engl J Med 2006;355:488-98. [Crossref] [PubMed]
- Kahn SR, Shbaklo H, Lamping DL, et al. Determinants of health-related quality of life during the 2 years following deep vein thrombosis. J Thromb Haemost 2008;6:1105-12. [Crossref] [PubMed]
- Piovella F, Crippa L, Barone M, et al. Normalization rates of compression ultrasonography in patients with a first episode of deep vein thrombosis of the lower limbs: association with recurrence and new thrombosis. Haematologica 2002;87:515-22. [PubMed]
- Prandoni P, Lensing AW, Prins MH, et al. Residual venous thrombosis as a predictive factor of recurrent venous thromboembolism. Ann Intern Med 2002;137:955-60. [Crossref] [PubMed]
- Shbaklo H, Holcroft CA, Kahn SR. Levels of inflammatory markers and the development of the post-thrombotic syndrome. Thromb Haemost 2009;101:505-12. [PubMed]
- Kahn SR. The post-thrombotic syndrome: progress and pitfalls. Br J Haematol 2006;134:357-65. [Crossref] [PubMed]
- Beckman JA. Cardiology patient page. Diseases of the veins. Circulation 2002;106:2170-2. [Crossref] [PubMed]
- Roumen-Klappe EM, den Heijer M, van Uum SH, et al. Inflammatory response in the acute phase of deep vein thrombosis. J Vasc Surg 2002;35:701-6. [Crossref] [PubMed]
- Prandoni P, Lensing AW, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med 2004;141:249-56. [Crossref] [PubMed]
- van Dongen CJ, Prandoni P, Frulla M, et al. Relation between quality of anticoagulant treatment and the development of the postthrombotic syndrome. J Thromb Haemost 2005;3:939-42. [Crossref] [PubMed]
- Ageno W, Piantanida E, Dentali F, et al. Body mass index is associated with the development of the post-thrombotic syndrome. Thromb Haemost 2003;89:305-9. [PubMed]
- Schulman S, Granqvist S, Juhlin-Dannfelt A, et al. Long-term sequelae of calf vein thrombosis treated with heparin or low-dose streptokinase. Acta Med Scand 1986;219:349-57. [Crossref] [PubMed]
- McLafferty RB, Moneta GL, Passman MA, et al. Late clinical and hemodynamic sequelae of isolated calf vein thrombosis. J Vasc Surg 1998;27:50-6; discussion 56-7. [Crossref] [PubMed]
- Kurz X, Kahn SR, Abenhaim L, et al. Chronic venous disorders of the leg: epidemiology, outcomes, diagnosis and management. Summary of an evidence-based report of the VEINES task force. Venous Insufficiency Epidemiologic and Economic Studies. Int Angiol 1999;18:83-102. [PubMed]
- Villalta S, Bagatella P, Piccioli A, et al. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome Haemostasis 1994;24:158a. (abstract).
- Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med 2001;161:2105-9. [Crossref] [PubMed]
- Eklöf B, Rutherford RB, Bergan JJ, et al. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg 2004;40:1248-52. [Crossref] [PubMed]
- Vasquez MA, Rabe E, McLafferty RB, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg 2010;52:1387-96. [Crossref] [PubMed]
- Schulman S, Kearon C; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692-4. [Crossref] [PubMed]
- Kearon C, Akl EA, Comerota AJ, et al. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e419S-94S.
- Kahn SR, Shapiro S, Wells PS, et al. Compression stockings to prevent post-thrombotic syndrome: a randomised placebo-controlled trial. Lancet 2014;383:880-8. [Crossref] [PubMed]
- Brandjes DP, Büller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet 1997;349:759-62. [Crossref] [PubMed]
- Vedantham S. Valvular dysfunction and venous obstruction in the post-thrombotic syndrome. Thromb Res 2009;123 Suppl 4:S62-5. [Crossref] [PubMed]
- Watson L, Broderick C, Armon MP. Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst Rev 2016;11:CD002783. [PubMed]
- Kahn SR, Galanaud JP, Vedantham S, et al. Guidance for the prevention and treatment of the post-thrombotic syndrome. J Thromb Thrombolysis 2016;41:144-53. [Crossref] [PubMed]
- Ginsberg JS, Magier D, Mackinnon B, et al. Intermittent compression units for severe post-phlebitic syndrome: a randomized crossover study. CMAJ 1999;160:1303-6. [PubMed]
- Cohen JM, Akl EA, Kahn SR. Pharmacologic and compression therapies for postthrombotic syndrome: a systematic review of randomized controlled trials. Chest 2012;141:308-20. [Crossref] [PubMed]
- Padberg FT Jr, Johnston MV, Sisto SA. Structured exercise improves calf muscle pump function in chronic venous insufficiency: a randomized trial. J Vasc Surg 2004;39:79-87. [Crossref] [PubMed]
- Khanna AK, Singh S. Postthrombotic syndrome: surgical possibilities. Thrombosis 2012;2012:520604.
- Neglén P, Hollis KC, Olivier J, et al. Stenting of the venous outflow in chronic venous disease: long-term stent-related outcome, clinical, and hemodynamic result. J Vasc Surg 2007;46:979-90. [Crossref] [PubMed]
- Raju S. Endovenous treatment of patients with iliac-caval venous obstruction. J Cardiovasc Surg (Torino) 2008;49:27-33. [PubMed]
- Jones DW, Schneider DB. Endovascular management of chronic inferior vena cava and iliac vein obstruction. Vasc Dis Manag 2012;9:E33-8.
- Raju S, Neglén P. Percutaneous recanalization of total occlusions of the iliac vein. J Vasc Surg 2009;50:360-8. [Crossref] [PubMed]
- Wahlgren CM, Wahlberg E, Olofsson P. Endovascular treatment in postthrombotic syndrome. Vasc Endovascular Surg 2010;44:356-60. [Crossref] [PubMed]
- AbuRahma AF, Perkins SE, Wulu JT, et al. Iliofemoral deep vein thrombosis: conventional therapy versus lysis and percutaneous transluminal angioplasty and stenting. Ann Surg 2001;233:752-60. [Crossref] [PubMed]
- Rosales A, Sandbaek G, Jørgensen JJ. Stenting for chronic post-thrombotic vena cava and iliofemoral venous occlusions: mid-term patency and clinical outcome. Eur J Vasc Endovasc Surg 2010;40:234-40. [Crossref] [PubMed]
- Raju S, Owen S Jr, Neglen P. The clinical impact of iliac venous stents in the management of chronic venous insufficiency. J Vasc Surg 2002;35:8-15. [Crossref] [PubMed]