Aortic valve repair with autologous pericardium for traumatic aortic valve regurgitation
Aortic valvuloplasty (AVP) remains a technically challenging operation. Therefore, in contrast to mitral valvuloplasty, which is a well established procedure for mitral valve regurgitation, AVP is performed in a small percentage of patients with aortic valve regurgitation (AR). We report the case of a patient with aortic regurgitation (AR) secondary to traumatic chest injury, who that successfully underwent AVP with autologous pericardial patch closure.
A 26-year-old man was referred to our hospital for consideration of surgical management six years earlier he was severely injured in a motorbike accident, with loss of consciousness and multiple bone fractures. He was taken to a local hospital, where he underwent bilateral chest tube drainage for hemothorax without definitive source. After stabilization and recovery, he was discharged, without symptoms of cardiovascular complications. However, during a follow-up visit as an outpatient, a new heart murmur was detected.
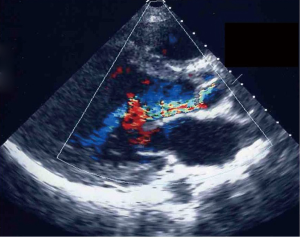
On admission to our hospital, he was in New York Heart Association functional class II. Transthoracic echocardiogram (TTE) revealed that AR was severe. Color Doppler echocardiography showed regurgitation flow, with a jet limited to the noncoronary cusp (Figure 1). The jet correlated to a tear localized in the noncoronary cusp. Cusp anatomy was otherwise normal with no evidence of annulus dilatation or vegetations. Aortography confirmed severe AR and normal coronary anatomy. These findings suggested that the mechanism of AR was a traumatic tear in the noncoronary cusp leaflet. Preoperatively, we considered the possibility to employ aortic valvuloplasty.
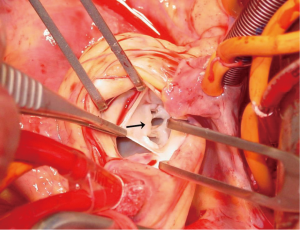
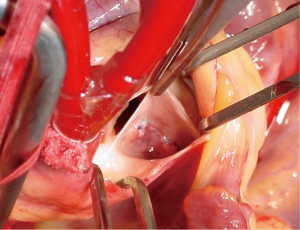
After establishing cardiopulmonary bypass, the aorta was clamped. Cardiac arrest was induced by cold blood cardioplegia and an oblique aortotomy was made. Intraoperative inspection revealed a tear (12 mm × 6 mm) of the aortic valve leaflet in noncoronary cusp. The rim around the tear was mildly elastic and stiff with some elastic bridging tissues, consistent with a chronic lesion in this patient 6 years after a motor-vehicle accident (Figure 2). Annulus dilatation was not seen and the other two leaflets were normal with good coaptation. In summary, the geometry of aortic valve apparatus was well preserved except for a leaflet tear of the noncoronary cusp. Therefore, we decided to perform AVP preserving leaflets. Fresh autologous pericardial patch was harvested and augmented to an oval shape for the repair of the tear. Polypropylene 6-0 stitches were placed in both its edges followed by continuous sutures for patch closure of the cusp tear (Figure 3).
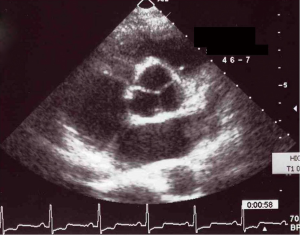
Good coaptation of three aortic valve leaflets with symmetry was obtained. After closing the aortotomy, we assessed the function of repaired aortic valve by TEE under beating heart conditions on cardiopulmonary bypass. The postoperative course was uneventful. There was no residual regurgitate flow across the valve with good coaptation of leaflets (Figure 4). Coumadin was prescribed for two months and then discontinues. Ten years later after surgery, the patient is in good condition.
Comments
In our institution, mitral valvuloplasty is employed for most of patients with mitral valve regurgitation. In contrast, we have no significant experience with. While operative techniques for AVP have been described in advanced centers (1,2), their use is limited compared to repair of atrioventricular valves. AVP remains a challenging operation, because successful repair requires detailed restoration of the geometry of the valvular apnparatus.
Typically, a combination of multiple factors including deformity and calcification of leaflets, dilatation of annulus, failure of coaptation between leaflets and avulsion of commissure contribute to AR. Therefore, it is difficult to restore valvular geometry completely by reconstructive procedures in most cases of AR.
In our patient with a history of blunt chest injury, the aortic valve had an isolated tear in noncoronary cusp, but no other deformity of configuration as a valve apparatus. The mechanism of traumatic AR is thought to be sudden elevation of intraaortic pressure during early diastole causing tension on the close aortic valve, leading to a tear or an avulsion of the leaflet. Similar to our patient, review of cases described in the literature confirms that the injury of the aortic valve is typically limited, with otherwise normal geometry (3-5). This isolated pattern of injury appears to favor the use of AVP in patients with traumatic AR compared to other etiologies.
There is remaining controversy whether to employ aortic valve replacement (AVR) or AVP for traumatic AR. Historically in the 1960s, when prosthetic valves were not available, AVP was performed for traumatic AR. However, most patients treated with AVP died in the hospital or AR recurred after surgery. In the 1970s, AVR with mechanical valve developed as the standard procedure for traumatic AR because of its feasibility and good outcome (4). However, complications associated with implantation of a prosthetic valve including thromboembolism and infections remain a concern. Recently, based on improved surgical techniques and experience, successful reports of AVP for acute traumatic AR have been described (5-7).
Intraoperative TEE is a major technological advance for the precise intra-operative evaluation of the valvular pathology and immediate success of repair, facilitating AVP for traumatic AR. AVR remains the standard procedure for traumatic AR with acute heart failure or complicated lesions. However, AVP should be attempted especially for younger patients with a simple, isolated tear and otherwise normal valve.
Leaflet tears are repaired with direct closure with or without pericardial patch reinforcement (5,6). Our case was unique because of the time lag between the trauma and the surgery, with development of a fibrous, stiff rim around the tear, allowed to secure running sutures. Carefully suturing the pericardial patch to the defect allowed to restore the shape of the injured cusp identical to the other two normal leaflets.
To our knowledge, reports have been sparse describing the repair of chronic traumatic AR. While traumatic AR is very rare, we suspect that some cases might be mistaken for ordinary AR. Therefore attention should be paid to the past history in patient with elective AR and an episode of trauma. Feasibility of AVP in these patients could avoid prosthetic valve implantation and lifetime anticoagulant.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Cosgrove DM, Rosenkranz ER, Hendren WG, et al. Valvuloplasty for aortic insufficiency. J Thorac Cardiovasc Surg 1991;102:571-6; discussion 576-7. [PubMed]
- Duran C, Kumar N, Gometza B, et al. Indications and limitations of aortic valve reconstruction. Ann Thorac Surg 1991;52:447-53; discussion 453-4. [PubMed]
- Najafi H, Dye WS, Javid H, et al. Rupture of an otherwise normal aortic valve. Report of two cases and review of the literature. J Thorac Cardiovasc Surg 1968;56:57-62. [PubMed]
- Loop FD, Hofmeier G, Groves LK. Traumatic disruption of the aortic valve. Cleve Clin Q 1971;38:187-94. [PubMed]
- Prêtre R, Faidutti B. Surgical management of aortic valve injury after nonpenetrating trauma. Ann Thorac Surg 1993;56:1426-31. [PubMed]
- Halstead J, Hosseinpour AR, Wells FC. Conservative surgical treatment of valvular injury after blunt chest trauma. Ann Thorac Surg 2000;69:766-8. [PubMed]
- Pettersson GB, Crucean AC, Savage R, et al. Toward predictable repair of regurgitant aortic valves: a systematic morphology-directed approach to bicommissural repair. J Am Coll Cardiol 2008;52:40-9. [PubMed]


