
Cutting balloon angioplasty for treatment of spontaneous coronary artery dissection: case report, literature review, and recommended technical approaches
Introduction
Spontaneous coronary artery dissection (SCAD) is an under-recognized and important cause of myocardial infarction (1). Conservative management remains the first-line recommended treatment strategy in the absence of ongoing ischemia, hemodynamic instability, or left main dissection. Percutaneous coronary intervention (PCI) of SCAD is associated with high rates of complications and relatively low technical success rates of ~60–70% (1-3). Treatment with coronary stenting with SCAD often requires multiple and very long stents, with subsequent high risk of in-stent restenosis. There is early and increasing interest in using cutting balloon (CB) angioplasty to fenestrate the false lumen to allow communication and back-bleed of intramural hematoma into the true lumen. We report a successful case of CB angioplasty for SCAD without the need for stenting, and provide a review of the published experience and recommendation for technical approaches with this strategy.
Case presentation
A 62-year-old post-menopausal woman with no cardiovascular risk factors presented with acute onset severe retrosternal chest pain with non-sustained ventricular tachycardia. Her electrocardiogram showed ST elevation in the lateral leads. She did not report any emotional or physical trigger for the event. She underwent emergent coronary angiography, which revealed type 2 SCAD of a large diagonal branch, with occlusion and thrombolysis in myocardial infarction (TIMI)-0 flow in the mid-distal vessel (Figure 1A). Left ventricular (LV) angiography revealed an ejection fraction (EF) of 45%, with dyskinetic apical and anterolateral segments. Non-selective catheter angiography showed fibromuscular dysplasia (FMD) involving the renal and iliac arteries.
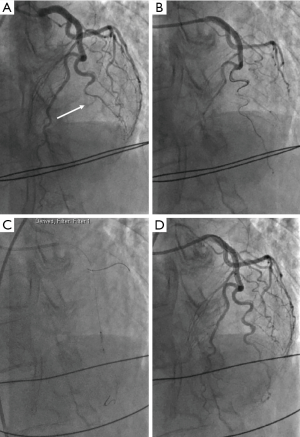
Given her ongoing chest pain and ischemia, the decision was made to proceed with PCI. A Balance Middle Weight (BMW) wire (Abbot Vascular, Santa Clara, CA, USA) was initially used to wire into the diagonal artery, but could not navigate into the distal segment of the artery. The Whisper wire (Abbot Vascular, Santa Clara, CA, USA) was then used to successfully access the distal diagonal artery true lumen, with improvement in coronary flow with wiring (Figure 1B). A 2.5/10 mm Flextome (Boston Scientific, Marlborough, MA, USA) CB was then inflated at the mid diagonal artery to 3 atm twice (Figure 1C). Following the inflations, there was normalization of flow to TIMI-3 to the distal diagonal artery (Figure 1D). There was evident intimal disruption of the dissection without compromising coronary flow, thus, coronary stent placement was not required. Her chest pain improved dramatically with resolution of the ST elevation.
She was admitted to the coronary care unit post-PCI and observed for 48 hours. She also had computed tomography angiogram of the head and neck vessels in-hospital, which demonstrated FMD of the internal carotid and vertebral arteries. Given the presence of FMD at multiple non-coronary vascular sites, this was felt to predisposing factor responsible for the patient’s presentation.
The remainder of her course in hospital was uneventful. She was discharged on dual anti-platelet therapy with ticagrelor and aspirin, as well as beta-blocker and ACE inhibitor. Echocardiogram performed 6 weeks after admission showed recovery of LVEF to 60% with no regional wall motion abnormality. She remained symptom-free at 5 months follow-up.
Discussion
We report a case of successful CB angioplasty in a patient with SCAD and ongoing ischemia of an occluded artery. Revascularization of patients with SCAD remains controversial and technically challenging. PCI in SCAD patients is associated with high rates of technical failure, dissection propagation and failure to cross the lesion (3,4). Furthermore, long-term outcomes with coronary stenting were poor, with successful and durable results in only 30% of cases (4). Coronary artery bypass graft (CABG) surgery for SCAD is also associated with high rates of technical failure. Tweet et al. reported that of 8 patients who underwent CABG for SCAD and underwent repeat coronary angiography in the course of follow-up, 11 of 15 grafts were occluded (3). PCI with CB angioplasty, especially without the need for stent placement, may be an alternative feasible option for SCAD revascularization.
The experience with CB angioplasty for SCAD is limited, only having been reported in 6 case reports to-date including ours (Table 1). Yumoto et al. reported a case of a 47-year-old woman with SCAD of the mid left anterior descending (LAD) artery with intramural hematoma confirmed by intravascular ultrasound (IVUS) (5). She underwent angioplasty with a 2.5 mm CB at 2 atm distally and 4 atm proximally. TIMI-3 flow was achieved immediately after balloon inflations. Optical coherence tomography (OCT) confirmed that incisions in the dissected intima successfully made communication between the true and false lumen. Repeat coronary angiography and OCT 6 months later revealed patency of the LAD, but with residual dissected intima. Ito et al. reported a 46-year-old woman with SCAD of the mid LAD confirmed by IVUS (6). PCI was attempted because of TIMI-0 flow and ST elevation, using a 2.0 mm Flextome CB. Following balloon inflation to 8 atm, TIMI-3 flow was restored and symptoms resolved. Computed tomography angiography demonstrated patent LAD 3 months post-angioplasty. Alkhouli et al. reported the use of CB in a 50-year-old woman with SCAD involving the mid LAD. She was initially managed conservatively, but developed recurrent chest pain with dynamic ECG changes (7). OCT confirmed the presence of a compressive hematoma. A 2.0/10 mm Flextome CB was used, followed by deployment of two 2.5/30 mm drug eluting stents (DES) with normal coronary flow after stent deployment. She remained symptom-free at 12 weeks follow-up. Lee et al. reported two SCAD cases using CB (8). The first was a 42-year-old woman with LAD SCAD confirmed with IVUS. This was treated with a 2.25/10 mm CB, which restored TIMI-3 flow. The second was a 46-year-old woman who presented with anterolateral ST elevation complicated by cardiac arrest. She had SCAD involving the mid-distal LAD treated with a 2.5 mm CB, followed by insertion of two DES in the mid-distal LAD with good angiographic result.

Full table
In the absence of data from randomized trials with long-term outcome results, revascularization strategies for SCAD remain contentious. Current expert consensus and observational data support conservative therapy as first-line therapy, since the majority of patients have no ongoing ischemia or sinister dissection anatomy, allowing spontaneous healing to occur without penalty, as part of the natural history of this condition with gradual resorption of the intramural hematoma. For cases with indication for revascularization, PCI is generally preferred over CABG if feasible. However, stenting is associated with significant risks, including stenting into false lumen, stent thrombosis, and long-term restenosis especially when long and multiple stents were used. Thus, a PCI strategy using angioplasty alone is attractive. However, with standard balloon inflations, the localized pressure against the arterial wall can propagate the intramural hematoma antegrade or retrograde, especially when there is no existing intimal disruption. Indeed, OCT studies have shown that most cases of SCAD involved intramural hematoma without intimal dissection (9). Therefore, intentional fenestration of the intima with CB to permit communication between the false and true lumen, allowing decompression of the intramural hematoma, is a potentially good strategy to improve true lumen patency.
There are a few important factors to consider when using CB for SCAD PCI (Table 2). First, the dissected arterial wall is frail and can be susceptible to perforation, thus, CB should be used cautiously with small diameter balloons and low inflation pressures. The Flextome balloons range from 2–4 mm in diameter, in 0.25 mm increments. We suggest using CB diameter that is at least 0.5 mm smaller than the caliber of the artery, and to avoid CB in vessels <2 mm in diameter. We also suggest inflating the CB to low pressures up to 4 atm, to minimize risk of perforation. Second, arteries affected by SCAD tend to be relatively tortuous, which makes it challenging to navigate stiff long blades into position. The lengths of Flextome balloons are available in 6, 10, or 15 mm, and we suggest the use of shorter lengths with either the 6 or 10 mm balloons. Third, optimal results with CB should include normalization of TIMI-3 flow and improvement of clinical symptoms. This may require a few low inflations to achieve TIMI-3 flow, in which case, coronary stenting would not be required. If coronary flow remains suboptimal after CB inflations, then, deployment of DES may be considered. Fourth, since CB angioplasty results in intimal disruption, potent antiplatelet therapy should be administered to minimize platelet adhesion to the ruptured intimal surface. We recommend the use of ticagrelor and aspirin for at least a month until vessel healing, followed by aspirin alone long-term. The use of heparins, GIIb/IIIa inhibitors and thrombolytics should not be used to avoid worsening of intramural hematoma (1). Finally, in terms of anatomic criteria for CB, the arterial segment involved and coronary flow should be taken into consideration. The use of CB in left main has not been explored to our knowledge. Given the usually large size of left main artery, the available CB sizes may not be adequate. Furthermore, the potential of creating large dissection flaps with large CB in the left main may be particularly risky for vessel occlusion. Typically, dissections involving the left main require CABG for optimal therapy (1). In terms of coronary flow, vessels with TIMI-0 or those with ≤2 flow plus symptoms, may particularly benefit from CB angioplasty.

Full table
Conclusions
Although the first-line therapy for patients with SCAD is conservative therapy, patients with ongoing ischemia, hemodynamic instability and left main dissection often requires urgent revascularization. Cautious CB angioplasty is a reasonable option as a PCI strategy in appropriately-sized arteries, and may achieve normalization of coronary flow without stent placement.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Saw reports having received unrestricted research grant supports (Canadian Institutes of Health Research, Heart & Stroke Foundation of Canada, National Institutes of Health, University of British Columbia Division of Cardiology, AstraZeneca, Abbott Vascular, Boston Scientific, and Servier), speaker honoraria (AstraZeneca, St Jude Medical, Boston Scientific, and Sunovion), consultancy and advisory board honoraria (AstraZeneca, and Abbott Vascular), and proctorship honoraria (Abbott Vascular and Boston Scientific). Dr. Lombardi reports being consultant (Boston Scientific, Abbott Vascular, Teleflex, Philips, Asahi Intec, Corindus), owns equity (Corindus), and spousal employment with Philips. Dr. Main has no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Saw J, Mancini GBJ, Humphries KH. Contemporary Review on Spontaneous Coronary Artery Dissection. J Am Coll Cardiol 2016;68:297-312. [Crossref] [PubMed]
- Alfonso F, Paulo M, Lennie V, et al. Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a "conservative" therapeutic strategy. JACC Cardiovasc Interv 2012;5:1062-70. [Crossref] [PubMed]
- Tweet MS, Eleid MF, Best PJ, et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777-86. [Crossref] [PubMed]
- Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645-55. [Crossref] [PubMed]
- Yumoto K, Sasaki H, Aoki H, et al. Successful treatment of spontaneous coronary artery dissection with cutting balloon angioplasty as evaluated with optical coherence tomography. JACC Cardiovasc Interv 2014;7:817-9. [Crossref] [PubMed]
- Ito T, Shintani Y, Ichihashi T, et al. Non-atherosclerotic spontaneous coronary artery dissection revascularized by intravascular ultrasonography-guided fenestration with cutting balloon angioplasty. Cardiovasc Interv Ther 2017;32:241-3. [Crossref] [PubMed]
- Alkhouli M, Cole M, Ling FS. Coronary artery fenestration prior to stenting in spontaneous coronary artery dissection. Catheter Cardiovasc Interv 2016;88:E23-7. [Crossref] [PubMed]
- Lee R, Ben-Dor I. Revascularization methods in spontaneous coronary artery dissection: A focused review. Cardiovasc Revasc Med 2017;18:544-8. [Crossref] [PubMed]
- Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. J Am Coll Cardiol 2012;59:1073-9. [Crossref] [PubMed]


