
Effects of “plate model” as a part of dietary intervention for rehabilitation following myocardial infarction: a randomized controlled trial
Introduction
Recurrent coronary events are a common phenomenon following myocardial infarction (MI) (1). A large-scale national Swedish registry study showed that the risk of cardiovascular events appeared high beyond the first year post-MI, indicating a need for prolonged surveillance, particularly in patients with additional risk factors (1). Number of pharmacological and non-pharmacological rehabilitation programmes are known to reduce recurrent events and improve outcome in survivors of MI. Cardiac rehabilitation encompasses comprehensive programmes aimed at limiting physiological and psychological effects of cardiac illness and reintegrating the patients to a satisfactory functional status (2). The physiologic parameters targeted by cardiac rehabilitation interventions include an improvement in exercise tolerance and in exercise habit, optimization of coronary risk factors, including improvement in lipid and lipoprotein profiles, body weight, blood glucose levels, blood pressure levels and cessation of smoking. Psychological factors include reduction of stress and anxiety and lessening of depression (3). The benefits of cardiac rehabilitation include reduction in mortality, morbidity, improvement of quality of life and the cardiovascular risk profile (2,4). More importantly, a comprehensive programme initiated soon after a MI, can be economically justified (5). An effective implementation of a rehabilitation programme depends on addressing all the core components including dietary modifications, improving physical activity level and support for psycho-social health (6). Exercise (7) and dietary (8) interventions are such integral elements of cardiac rehabilitation and secondary prevention of cardiovascular disease.
Excess adiposity as measured by BMI is associated with an increased risk of recurrent coronary events following MI, particularly among those who are obese (9). Therefore hypo caloric diet aimed towards intentional weight loss in obese patients is recommended for cardiovascular disease prevention (10). Moreover, a targeted weight management intervention should be an integral part of a cardiac rehabilitation program (11). Low carbohydrate diet is known to decrease body weight as well as improve cardiovascular risk factors (12). Increased consumption of vegetables and fruits, characteristic to a prudent traditional diet is considered to be cardio protective (13). The Mediterranean diet which confers mortality and morbidity benefits to patients with cardiovascular disease, also consists of increased amounts of vegetables and plant based foods (14). Despite being a main macronutrient, there is sparse evidence on recommendation of protein intake for cardiac patients. However the Mediterranean diet as well as American Heart Association dietary guidelines recommend sufficient intake of protein rich foods especially fish (14).
Most of the evidence on these dietary recommendations is derived from the western world. However, a diet should undoubtedly be culturally sensitive for successful practical implementation. Cardiovascular diseases are the main cause of mortality among Sri Lankan adults (15). Unhealthy dietary habits could be one of contributing factor for high cardiovascular mortality rate in Sri Lanka. The pattern of energy and nutrient intake among Sri Lankans differs from that of western world as well as the other Asian countries. Sri Lankan adults consume a very high carbohydrate diet (16). In the Sri Lankan diet, 72% of calories are derived from carbohydrate whereas protein and fat are responsible for 10% and 18% of the total caloric intake respectively (17). Moreover, fruits and vegetables consumption is very low among Sri Lankan adults, with only 3.5% of population achieving the ‘five fruits and vegetable per day’ target (17). Hence a substantial proportion of adult population in the local setting, fail to follow recommended dietary guidelines (16). Although there are no published data as of yet on dietary habits of post MI patients in Sri Lanka, our previous data shows that there is no significant change in their dietary habits irrespective of socio-economic factors or presence of diabetes and obesity (16).
The concept “plate model” is one of the practical methods to overcome the prevailing dietary pattern by reducing the average portion size of staple food in main meals, which also could ensure the sufficient intake of vegetables and protein foods simultaneously. The plate introduced in this study is divided into five segments by printed lines so that one-quarter of the plate is for rice (Figure 1). Another quarter is for protein-containing foods and the remaining half is for non-starchy vegetables. The segment representing the vegetables is again divided into three equal areas: one-third for green leafy salads and the other two-thirds for two different vegetables, including one green (18). Since the plate is divided into segments it highlights the different types of foods that should be included in a healthy meal and it shows the ideal portions of starch food, protein food and vegetables for a balanced intake. Therefore, the study aims to evaluate the effects of a plate model on modification of selected cardio metabolic risk factors in overweight patients with a history of MI.

Methods
An interventional, randomized, single-blinded study with parallel subject allocation was conducted among the patients with a history of troponin positive acute coronary syndrome (ACS). The details of the study have been discussed elsewhere (19). The present study was conducted with accordance to the guidelines laid down in the Declaration of Helsinki and was approved by the Ethics Review Committee (ERC), National Hospital of Sri Lanka and Faculty of Medicine, University of Colombo. This is registered under Sri Lanka Clinical Trials Registry (SLCTR/2016/22). Written informed consent was obtained from all the eligible subjects.
Inclusion and exclusion criteria
Recruitments were carried out from diagnosed patients with troponin positive MI admitted to Institute of Cardiology, National Hospital of Sri Lanka, Colombo. Study subjects fulfilling the inclusion and exclusion criteria were selected. (I) The patients included had a confirmed troponin positive ACS during the 1 month preceding the date of recruitment and were between the age of 20–70 years. (II) The subjects consumed rice for at least two main meals per day. Patients with end stage renal failure, congestive cardiac failure, chronic liver cell disease, severe anemia or other severe systemic disease, pregnant and breast-feeding mothers, patients with systemic infection were excluded. Patients who were already on a modified diet or dietary supplements were also excluded.
Assignment
The participants were randomly allocated to intervention and control groups. Then the participants were stratified according to gender and an even quota of male and female subjects in both groups were ensured. Detailed information on sampling has been previously described (19).
Justification of sample size
The sample size was selected on the basis of a pilot survey, and the number needed for recruitment was determined to account for a confidence level of 95%, a confidence interval of 10%, and 80% statistical power. A 10% hypothesized difference of participants’ body weight between the control and intervention groups following the plate model diet at the end of 12 weeks was taken as the primary outcome when calculating the sample size. Because the other biochemical parameters [blood pressure (BP), lipid profile (total, LDL and HDL cholesterol), triglyceride (TG), fasting blood sugar (FBS), and ALT] were prone to vary with medication and compliance with medication, they were not regarded in sample size calculations. A subsequent 5% withdrawal rate and another 40% loss to follow-up (total of 45%) were accounted for in the calculation. A total sample of 120 was recruited over an anticipated period of 3 months.
Intervention
Patients assigned to the control group received standard cardiac rehabilitation following MI. Intervention arm was provided with the ‘model plate’ in addition to routine rehabilitation care. The details of the plate model have been described elsewhere (19). In summary, the subjects received a plate made of melamine which is divided into segments to ensure adherence to a few dietary practices. Plate model encouraged consumption of non-starchy vegetables (half of the plate) and protein rich food such as fish (quarter of the plate) and discouraged over consumption of rice (only quarter of the plate) (Figure 1). Furthermore, a food poster was given to the patients following the plate model diet in order to enhance their knowledge on different food choices under each category. These patients were provided with nutrition advice customized according to patients’ social, economic and personal preferences.
The patient management team was blinded to the nature of intervention the patient was subjected to. The participants were thoroughly advised not to convey the information regarding the nature of intervention they were undergoing to other study participants to avoid breach of single blinded study design.
Measurements and follow-up
All the patients were given an interviewer administered questionnaire at recruitment through which demographic data, coronary risk factors, data on diagnosis and management were gathered. Baseline anthropometric measurements including body weight, height, waist circumference, hip circumference was measured using standard guidelines and blood pressure measurements were taken. Overnight fasting blood was collected to measure blood glucose, lipids and liver enzymes.
Patients were followed up at 4- and 12-week intervals. At these follow-up visits, blood pressure, anthropometric measurements were repeated. Fasting blood glucose and liver enzyme levels (ALT) were obtained at both follow-up visits. Lipid profile (total, LDL and HDL cholesterol) was repeated at 12 weeks.
Statistical analysis
The data were entered, coded and analyzed on SPSS version 23.0 (Armonk, NY: IBM Corp). After checking the data for normality, parametric and non-parametric statistical tests were applied for the data analysis. Summary statistics for both groups were calculated and presented as mean, standard deviation. Differences in baseline characteristics between the intervention and control groups were tested using chi-square tests and independent sample 2-sided t-tests. Effects with P<0.05 were considered significant. For the study BMI ≥23 kg/m2 was considered overweight or obese (20).
Results
Out of the 120 participants enrolled in both the groups, at the end of 12 weeks 66.6% (n=40) in the intervention group and 65% (n=39) in the control group completed the study (Figure 2). Results herein are reported for the 79 participants who completed the study. The study participants’ mean (± SD) age was 50.5±10.6 years and majority (n=71) were men. Baseline characteristics of the study population comprising of age, clinical, anthropometric, behaviour and biochemical parameters are presented in Table 1.
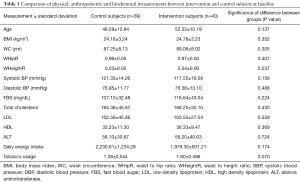
Full table
During the 12-week follow-up period a significant mean weight loss (intervention group: −1.27±3.58 kg; control group: −0.26±2.42 kg) was observed among the participants of the intervention group than the control group (P=0.029). Furthermore, the change in BMI measurements were significantly different between the groups (P=0.023) where the mean BMI reduction was significant among those who received the plate model (−0.48±1.31 vs. −0.10±0.89 kg/m2) (Table 2). Other anthropometric measurements such as waist circumference (IG: −1.66±4.35 cm; CG: −2.52±5.05 cm; P=0.421), hip circumference (IG: −0.36±4.54 cm; CG: −1.96±3.88 cm; P=0.095), waist hip ratio (IG: −0.01±0.04; CG: −0.01±0.03; P=0.365) and waist height ratio (IG: −0.01±0.03; CG: −0.02±0.03; P=0.401) remained unchanged or decreased in both the groups. But none of the reductions were statistically significant between the groups.
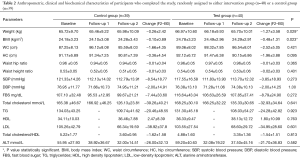
Full table
Systolic (IG: −7.85±18.76 mmHg; CG: −3.94±20.34 mmHg) and diastolic (IG: −2.61±15.32 mmHg; CG: −3.05±14.35 mmHg) blood pressure reduced slightly from baseline values in both the groups during the 12-week follow-up. Similarly, although the changes were not significant, bio chemical parameters such as FBS, TG, LDL cholesterol and total cholesterol levels also have dropped down from the baseline values at the end of the follow-up period in both the control and intervention groups.
In the subgroup analysis, the reduction in weight and BMI values were significantly different among overweight and obese subjects (BMI ≥23 kg/m2) in the intervention and the control groups. But there were no significant changes exhibited across parameters of non-overweight subjects (BMI ˂23 kg/m2) (Table 3). The proportion of overweight and obese patients who underwent a weight loss of ≥5% during a short time period was greater in the test group (35.7%) than in the control group (13.04%). The test value was nearly significant between the two groups (P=0.065).
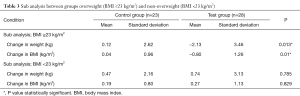
Full table
Discussion
Obesity adversely affects cardiac function, increases the risk factors for coronary heart disease, and is an independent risk factor for cardiovascular diseases (21). A “plate model” is one practical intervention to reduce the calorie intake by reducing the portion size of staple food in main meals. To our knowledge, this is the first randomized controlled single-blinded study to assess the effect of a ‘plate model’ as a dietary interventional study in patients after MI in Sri Lanka or South Asia. According to previous literature, similar plate models named “My Plate” and “healthy eating plate” have been introduced by the U.S. Department of Agriculture with Department of Health and Human Service and also by the Harvard Health Publishing, in conjunction with nutrition experts at Harvard School of Public Health (HSPH) (22). In “My Plate” the U.S. Department of Agriculture has introduced five food groups namely, fruits, vegetables, grains, proteins and dairy as the building blocks for a healthy diet (23). The “Healthy eating plate” has addressed important deficiencies in “My Plate” by replacing the dairy with healthy oils and water and also reminded that staying active is half of the secret to weight control (24). Therefore, it is apparent that several countries have recommended “plate” concept for their respective population.
The key findings of the study revealed that the intervention group who followed the plate model has a significant effect on weight and BMI reduction after 12 weeks than the control group. A significant result was witnessed among overweight and obese patients. As expected from the study, those who were not overweight had no reduction in weight but their weights were stable throughout the study period.
The consumption of vegetables, protein and cutting down excess carbohydrates is a healthy move for the secondary prevention of cardiovascular event (20). The intervention group served smaller portions on the plate model than the participants in the control group who used the regular plate. Portion control is an important aspect of reducing energy intake. During ad libitum feeding, a direct relationship is found between portion size served and intake; therefore, increasing the size of the portion served increases the amount of food consumed (25). In the present study the amount of food consumed by the intervention group who received the plate model was quite similar, regardless of the types of foods and the energy intake. The participants in the control group did not eat a consistent amount of food as they didn’t follow the plate model. This group may have eaten more when compared to intervention group when adults themselves or someone else determined the portion served on the plate.
Previous studies have shown that increasing portion sizes led to significantly increased energy intake (25,26) and body weight (27). To systematically assess the effect of portion size on food, Rolls et al. conducted a study where men and women were served different portions of macaroni and cheese on different occasions, they consumed 30% more energy (676 kJ; 162 kcal) when offered the largest portion (1,000 g) than when offered the smallest portion (500 g) (25).
The energy content of a diet is the primary determinant of weight loss. Although low-carbohydrate diets have become increasingly popular for weight loss and to reduce cardiovascular risks, Jayawardena et al. reported that Sri Lankan men consumed higher amount of starch compared to their female counterpart and also more than 12% of men consumed ≥25 starch servings/d while 1% of females consumed that amount. A study carried out by Foster and colleagues on the effect of low-carbohydrate diet revealed that subjects on the low-carbohydrate diet had lost more weight than subjects on the conventional diet at 3 months [mean (±SD), −6.8±5.0 vs. −2.7±3.7 percent of body weight; P=0.001], but the difference at 12 months was not significant (−4.4±6.7 vs. −2.5±6.3 percent of body weight, P=0.26) (28). In contrast to these findings Stern et al. found that participants on the low-carbohydrate diet maintained most of their 6-month weight loss, whereas those on a conventional diet continued to lose weight throughout the year (29).
A systematic review and meta-analysis showed that life style modification strategies (defined as any strategy focused on improving physical activity and/or diet to prevent diabetes through weight loss) implemented under real-world conditions are promising approaches for preventing diabetes (30). In this study the participants receiving an intervention had a 29% lower risk of developing diabetes, lost 1.5 kg more body weight, and reduced fasting blood glucose by 0.09 mmol/L more than participants not receiving one (30).
Apart from dietary interventions, evidence was available for motivational and behavioral intervention studies carried out to treat obesity in cardiac patients. A systemic review on motivational interviewing revealed that there is a significant reduction in body weight (kg) for those in the intervention group compared with those in the control group [weighted mean difference (WMD) =−1.47 kg (95% CI: −2.05, −0.88)]. For the BMI outcome, the WMD was −0.25 kg/m2 (95% CI: −0.50, 0.01) (31). Another study which investigated the effect of supervised cardiac rehabilitation programs over non-supervised programs revealed that there is a significant decrease in body weight, waist circumference, waist to hip ratio and body mass index in patients engaged in supervised program than the patients attended to the non-supervised program (32). In the systematic review by Klein et al. has stated that persons who are overweight or obese and physically active (participate in 30 minutes of moderate-intensity physical activity most days of the week) or who have moderate to high levels of cardio respiratory fitness (in the upper four fifths of the age and sex fitness distributions) have much lower death rates from cardiovascular disease and all-cause mortality than people who are sedentary and unfit (33).
When practicing the plate model concept several limitations were identified which may have hindered the accuracy of the outcome of final results. In the current study the patient compliance was not measured. Therefore, if a participant did not follow the instructions in the way that is required, the results collected from that participant would not be a valid assessment. Further the results may differ due to other limitations such as, economic barriers, myths and beliefs. The participants may also have difficulties in following the advices due to relative high cost of vegetables and proteins rich food items compared starchy foods in Sri Lanka. As the participants consumed different types of foods, the energy intake may differ affecting the results of the study. Since most vegetables are consumed as curries in Sri Lanka, the fat and total calorie content of the dish may differ with the mode of preparation. Moreover, the participants might have other dietary (cut down on saturated fats) and exercises habits given in the standard rehabilitation program, which may also interfere the results. Here the participants were not necessarily attempting to lose weight, so results may have differed for participants motivated to choose smaller portions for weight loss. The notable strengths of this study were the intervention being very simple and inexpensive.
Conclusions
Plate model is an effective dietary intervention in view of weight reduction in post-MI patients especially for overweight and obese patients. Compared to other complicated weight loss strategies, plate model is ideal for many people because of its simplicity and easiness to follow. Also, it is an effective way of introducing meal planning which is an alternative to the traditional way of exchange-based teaching and meal planning.
Acknowledgements
Authors would like to thank all research assistants including Dr. Pasindu Fernando and Mrs. Nishanthi Wijayathunge. This work was funded by the Cardiology Trust Fund, Institute of Cardiology, National Hospital of Sri Lank.
Footnote
Conflicts of Interest: R Jayawardena has written a book based on plate model concept namely My Rice Plate. It has been published by Colombo Medical Faculty Publisher, University of Colombo, Sri Lanka. R Jayawardena has already applied for patent for the melamine rice plate and his application is under review. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ethics Review Committee (ERC), National Hospital of Sri Lanka and Faculty of Medicine, University of Colombo. This is registered under Sri Lanka Clinical Trials Registry (SLCTR/2016/22). Written informed consent was obtained from all the eligible subjects.
References
- Jernberg T, Hasvold P, Henriksson M, et al. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J 2015;36:1163-70. [Crossref] [PubMed]
- Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ 2015;351:h5000. [Crossref] [PubMed]
- Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther 2012;2:38-49. [PubMed]
- Oldridge N, Guyatt G, Jones N, et al. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol 1991;67:1084-9. [Crossref] [PubMed]
- Oldridge N, Furlong W, Feeny D, et al. Economic evaluation of cardiac rehabilitation soon after acute myocardial infarction. Am J Cardiol 1993;72:154-61. [Crossref] [PubMed]
- Mampuya WM. Cardiac rehabilitation past, present and future: an overview. Cardiovasc Diagn Ther 2012;2:38-49. [PubMed]
- Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004;116:682-92. [Crossref] [PubMed]
- Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937-52. [Crossref] [PubMed]
- Rea TD, Heckbert SR, Kaplan RC, et al. Body mass index and the risk of recurrent coronary events following acute myocardial infarction. Am J Cardiol 2001;88:467-72. [Crossref] [PubMed]
- Lichtenstein AH, Appel LJ, Brands M, et al. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82-96. [Crossref] [PubMed]
- Bader DS, Maguire TE, Spahn CM, et al. Clinical profile and outcomes of obese patients in cardiac rehabilitation stratified according to National Heart, Lung, and Blood Institute criteria. J Cardiopulm Rehabil 2001;21:210-7. [Crossref] [PubMed]
- Hu T, Bazzano LA. The low-carbohydrate diet and cardiovascular risk factors: Evidence from epidemiologic studies. Nutr Metab Cardiovasc Dis 2014;24:337-43. [Crossref] [PubMed]
- Sivasankaran S. The cardio-protective diet. Indian J Med Res 2010;132:608-16. [PubMed]
- Walker C, Reamy BV. Diets for cardiovascular disease prevention: what is the evidence? Am Fam Physician 2009;79:571-8. [PubMed]
- Organization WH. Sri Lanka noncommunicable diseases profile 2014. Available online: http://www.who.int/nmh/countries/lka_en.pdf?ua=1
- Jayawardena R, Byrne NM, Soares MJ, et al. Food consumption of Sri Lankan adults: an appraisal of serving characteristics. Public Health Nutr 2013;16:653-8. [Crossref] [PubMed]
- Jayawardena R, Thennakoon S, Byrne N, et al. Energy and nutrient intakes among Sri Lankan adults. Int Arch Med 2014;7:34. [Crossref] [PubMed]
- Jayawardena DR. My Rice Plate – An evidence based approach to lose excess body weight. Sri Lanka: Colombo Medical Faculty Publishers, 2017:28.
- Jayawardena R, Fernando P, Lokunarangoda N, et al. Effects of the “plate model” as part of dietary intervention on modification of selected cardiometabolic risk factors in post-myocardial infarction patients: study protocol for a randomized controlled trial. Trials 2017;18:314. [Crossref] [PubMed]
- Behl S, Misra A. Management of obesity in adult Asian Indians. Indian Heart J 2017;69:539-44. [Crossref] [PubMed]
- Van Gaal LF, Mertens IL, Christophe E. Mechanisms linking obesity with cardiovascular disease. Nature 2006;444:875. [Crossref] [PubMed]
- Datz T, Communications HSoPH. Harvard serves up its own ‘Plate’. Available online: https://news.harvard.edu/gazette/story/2011/09/harvard-serves-up-its-own-plate/
- United States Department of Agriculture 2019. What is myplate? Available online: https://www.choosemyplate.gov/WhatIsMyPlate
- Harvard Health Publishing 2011. Harvard researchers continue to support their healthy eating plate, Harvard Medical School. Available online: https://www.health.harvard.edu/staying-healthy/harvard-researchers-launch-healthy-eating-plate
- Rolls BJ, Morris EL, Roe LS. Portion size of food affects energy intake in normal-weight and overweight men and women. Am J Clin Nutr 2002;76:1207-13. [Crossref] [PubMed]
- Rolls BJ, Roe LS, Meengs JS. Larger portion sizes lead to a sustained increase in energy intake over 2 days. J Am Diet Assoc 2006;106:543-9. [Crossref] [PubMed]
- Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health 2002;92:246-9. [Crossref] [PubMed]
- Foster GD, Wyatt HR, Hill JO, et al. A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003;348:2082-90. [Crossref] [PubMed]
- Stern L, Iqbal N, Seshadri P, et al. The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: One-year follow-up of a randomized trial. Ann Intern Med 2004;140:778-85. [Crossref] [PubMed]
- Galaviz KI, Weber MB, Straus A, et al. Global Diabetes Prevention Interventions: A Systematic Review and Network Meta-analysis of the Real-World Impact on Incidence, Weight, and Glucose. Diabetes Care 2018;41:1526-34. [Crossref] [PubMed]
- Armstrong MJ, Mottershead TA, Ronksley PE, et al. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta‐analysis of randomized controlled trials. Obes Rev 2011;12:709-23. [PubMed]
- Nalini M, Moradi B, Esmaeilzadeh M, et al. Does the effect of supervised cardiac rehabilitation programs on body fat distribution remained long time? J Cardiovasc Thorac Res 2013;5:133. [PubMed]
- Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2004;110:2952-67. [Crossref] [PubMed]



