Conservative treatment of iatrogenic left main coronary artery dissection: report of two cases
Introduction
Although rare with a reported incidence of less than 0.1% (1), iatrogenic left main coronary artery (LMCA) dissection has devastating consequences because of rapid deterioration of antegrade coronary blood flow due to unpredictable nature of the dissection flap (2). Therefore, immediate revascularization strategy has been mostly considered as appropriate treatment of choice, even in patients with initial distal TIMI 3 flow and hemodynamic stability (2). On the other hand, conservative treatment of iatrogenic non-occlusive dissection of LMCA has been shown to be in association with quite satisfactory long-term outcomes in patients with distal TIMI 3 flow and hemodynamic stability (3). We present two case reports of iatrogenic non-occlusive LMCA dissection and wanted to highlight the importance of conservative treatment of iatrogenic LMCA dissections.
Case reports
Case 1
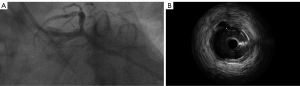
A 48-year-old man in whom right coronary artery (RCA) stent implantation was performed 1 year ago was admitted to our hospital because of typical chest pain continued for 1 hour. There was no significant ECG change and cardiac biochemical markers were within normal limits (troponin I <0.04 ng/mL). Elective coronary angiography was performed and revealed a significant stenosis in the proximal segment of left anterior descending (LAD) artery and percutaneous coronary intervention was decided. A 7F Judkins left 4.0 (JL4) guiding catheter (Cordis Corporation, a Johnson & Johnson company; Miami, Florida) was used and engagement of LMCA was established successfully. However, the guiding catheter was inadvertently deep engaged into the LMCA during the procedure and contrast injection revealed a type-A dissection (NHLB-I classification) in the distal LMCA (Figure 1). The patient was asymptomatic, hemodynamically stable and antegrade coronary flow was satisfactory with TIMI 3 flow distally. Therefore, any revascularization strategy was not considered. The patient was transferred to the coronary intensive care unit, monitored closely and given intravenous heparin infusion at recommended dosage. The patient was discharged in a very good condition with an optimal medical treatment after 3 days. At three-month follow-up, he did not have any complaint.
Case 2
A 60-year-old man with a history of coronary artery bypass grafting operation (Left internal mammary artery to LAD, saphenous vein graft to the RCA) was referred for cardiac catheterization with a history of atypical chest discomfort and an anterior perfusion defect on non-invasive stress testing. His ECG and biochemical test results were within normal limits. A coronary angiography, using a 4 Fr Judkins left 4.0 (JL4) diagnostic catheter (Cordis Corporation, a Johnson & Johnson company; Miami, Florida), revealed no significant stenosis in coronary arteries, but unfortunately resulted in a type-A dissection (NHLB-I classification) in the distal LMCA (Figure 2). The patient was asymptomatic, hemodynamically stable and antegrade coronary flow was satisfactory with TIMI 3 flow distally. The patient was closely monitored at coronary intensive care unit for 3 days with optimal medical treatment (anticoagulation and beta blocker) and discharged in a very good condition.

Discussion
Catheter-induced LMCA dissections are quite rare with very few reports in the literature. Unusual LMCA anatomy or location, presence of LMCA atherosclerosis, operator experience, vigorous hand injection of contrast medium, selection of catheter type (left Amplatz guiding catheters are associated with a higher risk of dissection), inappropriate positioning of the catheter in co-axial alignment with LMCA and subintimal passage of the guidewire (especially stiffer and less manageable guide wires) have all been associated with an increased risk of iatrogenic LMCA dissection (1-4). Iatrogenic LMCA dissection is twice as likely to occur during coronary intervention compared to diagnostic angiography (5) and the deep engagement of guiding catheters while the angioplasty balloon withdrawn is often suggested to be responsible for iatrogenic LMCA dissection (1).
The strategy for managing of LMCA dissection is variable and depends upon the mechanism, the co-morbidities of the patient and degree of hemodynamic stability. Revascularization strategy has been mostly considered, as appropriate treatment of choice and timing is dependent upon the clinical scenario. Hemodinamically unstable patients are most likely undergo percutaneous coronary intervention (PCI). Because PCI (bailout stenting) of LMCA can be performed rapidly shortly after iatrogenic LMCA dissection occurred and has high technical success. Nevertheless, some authors suggest a revascularization strategy even in hemodynamic stabile patients with initial distal TIMI 3 flow because of unpredictable nature of the dissection flap and the potential for rapid deterioration of antegrade coronary blood flow (2). But it must not be forgotten that although high technical success and low in-hospital mortality rate, PCI (bailout stenting) of iatrogenic LMCA dissection was reported in association with more frequent in-stent restenosis with a binary restenosis rate of 30% (6) and target vessel revascularization during long-term follow-up (5). Coronary artery bypass grafting (CABG) is particularly valuable in hemodinamically stable patient with extensive iatrogenic LMCA dissection (antegrade or retrograde extension into the aortic root) and multivessel disease. However emergent surgery for left main dissections comes with its inherent risks.
On the other hand, conservative treatment is rarely considered as potential therapeutic strategy for the treatment of iatrogenic LMCA dissection. Conservative treatment should be considered in hemodynamically stable patients with localized and low-grade dissection. Conservative treatment includes close monitoring with optimal medical treatment including beta-blocker and anticoagulation to prevent progressive dissection and superimposed thrombus formation. Thrombolytics can be administered to dissolve clot associated with dissection. In their study, Eshtehardi et al. (5) report 38 patients with iatrogenic LMCA dissections and 6 of 38 patients were treated conservatively. In another study, Awadalla et al. (1) report 5 patients with iatrogenic LMCA dissection and 1 of 5 patients was treated conservatively. A favorable safety profile during short- and long-term follow-up was reported in all of these patients treated conservatively. Also, it is obvious that conservative management may prevent unnecessary stenting and restenosis at the LMCA stent necessitating subsequent PCI and/or CABG, especially in patients with low-grade dissection. In our cases, the patients were asymptomatic and hemodinamically stable with TIMI 3 flow distally. Therefore, any intervention was not performed and the patients were managed conservatively.
In conclusion, iatrogenic LMCA dissection is a rare but life-threatening complication of cardiac catheterization. Firstly, a careful interventional technique is pivotal to prevent iatrogenic LMCA dissection. The therapeutic strategy largely includes revascularization with PCI or CABG. However, conservative treatment seems to be feasible and safe in hemodinamically stable patients with a low-grade dissection.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Awadalla H, Sabet S, El Sebaie A, et al. Catheter-induced left main dissection incidence, predisposition and therapeutic strategies experience from two sides of the hemisphere. J Invasive Cardiol 2005;17:233-6. [PubMed]
- Onsea K, Kayaert P, Desmet W, et al. Iatrogenic left main coronary artery dissection. Neth Heart J 2011;19:192-5. [PubMed]
- Kovac JD, de Bono DP. Cardiac catheter complications related to left main stem disease. Heart 1996;76:76-8. [PubMed]
- Slack JD, Pinkerton CA, VanTassel JW, et al. Left main coronary artery dissection during percutaneous transluminal coronary angioplasty. Cathet Cardiovasc Diagn 1986;12:255-60. [PubMed]
- Eshtehardi P, Adorjan P, Togni M, et al. Iatrogenic left main coronary artery dissection: incidence, classification, management, and long-term follow-up. Am Heart J 2010;159:1147-53. [PubMed]
- Lee SW, Hong MK, Kim YH, et al. Bail-out stenting for left main coronary artery dissection during catheter-based procedure: acute and long-term results. Clin Cardiol 2004;27:393-5. [PubMed]


