
Long term mortality and readmissions after transcatheter aortic valve replacement
Introduction
Transcatheter aortic valve replacement (TAVR) has revolutionized our approach to treating severe aortic stenosis (AS). Despite significant improvements in mortality, readmissions after TAVR are common (1) and associated with increased health costs (2). Previous studies have examined 30-day readmissions and have estimated a significant associated health burden (2). However, limited data are available on TAVR readmissions beyond this time frame.
According to the 2016 Annual Report of the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry (3), 54,782 patients had undergone TAVR in the United States from 2012 to 2015. Despite the increase in volume of TAVRs from 4,627 in 2012 to 24,808 by the end of 2015, observed in-hospital mortality and 1-year mortality rates had declined over that time period (3).
TAVR was initially approved for patients with severe symptomatic aortic stenosis with high or prohibitive risk for surgical aortic valve replacement (4). Given the advanced age and significant comorbidities of these patients, thirty-day all-cause readmissions rates have remained high and range from 14.6% to 20.9% (1,2,5-7). In a study by Kolte et al., (2), of 2,188 readmissions, the majority (61%) were due to a non-cardiac primary diagnosis. However, limited data are available on the causes and the temporal distribution of readmissions post-TAVR beyond this time frame. Further detailed analysis of longer outcomes beyond thirty days may provide better insight on the natural history of this patient population.
Unplanned readmissions to the intensive care unit are associated with higher rates of in-hospital mortality (8,9). Elderly individuals who survive their ICU stay have shown higher mortality than hospital controls (10). Several studies have shown a significant increase in mortality, re-hospitalizations, and increased healthcare utilization after an ICU admission (11,12). No data exists on long term outcomes in TAVR patients after unplanned ICU admissions.
Accordingly, the main objectives of our study were to characterize the incidence, causes, and outcomes of long-term readmissions for up to 3-year after TAVR. We also sought to examine outcomes in readmissions between different levels of care (ICU vs. non-ICU settings).
We present the following article in accordance with the STROBE reporting checklist (available at https://dx.doi.org/10.21037/cdt-20-916).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the UPMC Institutional Review Board Committee (No. 18120143) with a waiver of individual consent due to the retrospective nature of the study.
Study population
We included all consecutive patients with severe aortic stenosis referred for TAVR from 2011 through 2017 at the University of Pittsburgh Medical Center (UPMC) and affiliated hospitals. Patients underwent comprehensive clinical evaluation by the designated Heart Team and deemed appropriate to undergo TAVR as suggested by the current 2017 ACC expert consensus decision pathway guidelines for TAVR (13). Clinical, laboratorial and procedural data were collected. Patients were clinically followed up in our program at 1, 6-, and 12-month post-TAVR, and annually thereafter. A full description of the clinical care received by patients is described in the Supplementary Data (Appendix 1). Detailed demographics, baseline comorbidities, echocardiographic parameters, procedural characteristics, and outcomes were recorded.
Outcomes
All-cause readmission was defined as any readmission occurring after discharge from the index TAVR procedure hospitalization. All readmissions were tracked within a large 40-hospital system and adjudicated via review of the electronic heath records (MHS) and classified based on primary readmission diagnoses (cardiac versus non-cardiac) and level of care (ICU versus non-ICU). In the case of discrepancies between diagnosis codes or lack of clarity, a consensus agreement (MHS, AM, SM) was reached on the primary readmission diagnosis. Cardiac readmissions were classified into TAVR-related, coronary artery disease, heart failure, arrhythmia, valvular, and pericardial disease. Non-cardiac readmissions were categorized into sepsis/infection, respiratory, liver disease, gastrointestinal, renal, trauma, vascular, hematological, neurological, malignancy, musculoskeletal, or others (Table S1). Secondary readmission diagnoses were not included. We used overlapping Kaplan-Meier curves, each illustrating freedom from readmission for the whole cohort for cardiac and non-cardiac readmissions. All-cause mortality was obtained from the review of the expiration summary for patients who died during a readmission, and through the Social Security Death Index (obtained from the updated Social Security Administration Death Master file, where our health-care system is certified by the Social Security Administration as an organization that is exempt from the three-year delay) for patients who were not readmitted.
Statistical analysis
Continuous variables are presented as mean ± SD and categorical variables as frequency (percentage). We analyzed inpatient readmissions based on primary diagnosis, ICU versus non-ICU designations, and time to readmission from index discharge (≤30 days, 30–90 days, 90 days <1-year). Kaplan Meier curves were used to estimate survival and readmission for both cardiac and non-cardiac causes. Instantaneous hazard functions were obtained (calculated as percent/month) to estimate the hazard of experiencing a cardiac or non-cardiac readmission and mortality stratified by level of care (ICU and non-ICU). Instantaneous hazard has been used previously to describe temporal risk of outcomes in TAVR patient populations (14). We have used readmission and mortality hazard curves to depict risk gradients over time.
For mortality after readmission, time zero was the day of procedure for those patients who did not have an inpatient readmission. For all other patients, time zero was the first day of the readmission. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Study population
Baseline characteristics of the 1,037 TAVR patients who survived their index hospitalization are shown in Tables 1,2. The Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) was obtained on 942 of the 1,037 patients (mean STS Score 7.96±4.72). The mean age at the time of the procedure was 81.8±7.85 years, 518 (50%) were females. Patient comorbidities included diabetes (41.7%), hypertension (89.4%), history of heart failure (80.9%) current smoking status (5.2%), sleep apnea (16.5%), dialysis (4.8%), history of CVA (13.3%), history of TIA (10.5%), prior CABG (25.9%), prior valve surgery (11.1%), and prior MI (39%).
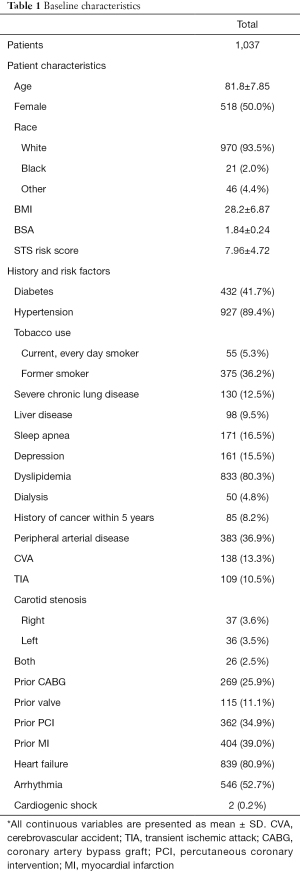
Full table

Full table
Over 75% of patients had NYHA Class III/IV at the time of the procedure. Initial presentation with cardiogenic shock was seen in 0.2% of the patients. Significant CAD (single vessel or more) was present in 65% of patients. Table S2 illustrates the echocardiographic characteristics of these patients. Pulmonary artery systolic pressure was 49.4±17.1 mmHg. Left ventricular ejection fraction (EF) was less than 50% in 28.1% of patients and 75.4% had aortic valve mean gradients of >40 mmHg. 11.3% of patients had an aortic mean gradient <40 mmHg and an EF <50%.
Outcomes
There were readmissions due to noncardiac causes in 350 (34.4%) and cardiac causes in 208 (20.5%) during a mean 1.96 years of follow-up. The most common non-cardiac causes of readmission were sepsis/infection (14.3%), gastrointestinal (8.3%), and respiratory (4.8%), whereas heart failure (14.0%) and arrhythmias (4.6%) were the most common cardiac causes of readmission (Table 3).
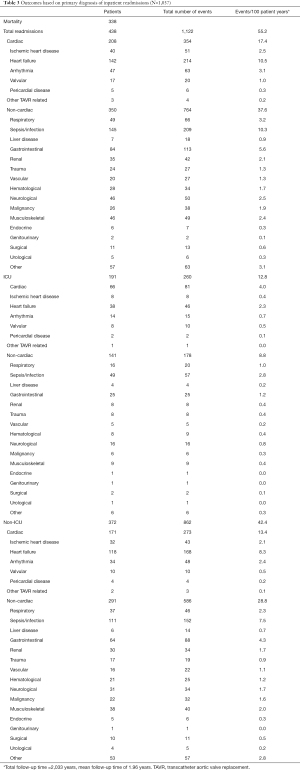
Full table
Overall, the rate of non-cardiac readmissions was greater than the rate of cardiac readmissions and this trend persisted up to three years from the time of index discharge (Figure 1). Figure S1 illustrates the instantaneous hazard function for overall readmission, and shows the risk of a noncardiac readmission was highest in the period immediately following TAVR (~4.6%/month) with an early high hazard phase that gradually declined to 2.5%/month at 6-month, 1.7%/month at 1-year, 1.3%/month at 2-year, and 0.7%/month at 3-year. However, the risk of cardiac readmission remained stable throughout the 3-year follow-up period ranging from 0.7% to 1.2% per month.
Non-cardiac readmissions remained more prevalent than cardiac readmissions whether admitted to the ICU or a non-ICU setting (Figures S2,S3). The risk of non-cardiac readmissions exhibited a similar early high hazard phase immediately following TAVR (Figures S4,S5) in both ICU and non-ICU readmissions.
The overall mortality was 14.9% at 1-year, 25.2% at 2-year, and 38.3% at 3-year (Figure 2). Instantaneous hazard estimates of mortality showed an early high hazard phase shortly after TAVR (3.3% per month) that declined and stabilized but gradually increased after three years (1.1%/month at 6 months, 1%/month at 1-year, 1.3% at 2-year, 2.1% at 3 years) (Figure S6).
Mortality for patients who had no readmissions was approximately 0.8–1.1%/month throughout the 3-year follow-up period (Figure 3). Instantaneous hazard function estimates for mortality after readmissions ranged from 2.0–3.9%/month. Mortality risk was higher following any type of readmission as compared to no readmission (Figure 3). The highest risk for mortality was in the period shortly after TAVR (Figure 3). In addition, TAVR patients exhibited an increased risk of mortality after any ICU readmission during the three-year follow up period (Figure 4). Mortality rates after ICU readmissions ranged from 2.2–7.6%/month (Figure 4).
Discussion
There are three important observations from this analysis. First, our data show that non-cardiac causes remain the most common reason for readmissions after long term follow up. Second, there is a strong association between any readmission and mortality and the highest risk of readmission and subsequent mortality occurs immediately after the TAVR procedure. Finally, there is a high risk of mortality after any readmission at any point within the 3-year follow-up period, but it is particularly high after an ICU readmission.
Readmissions after TAVR are common with approximately 15–17% of patients requiring hospital readmission within 30 days and nearly half within one year of their procedure (1,2,6). Several studies have explored the incidence and outcomes of TAVR patients within 30-day (2) and 1-year (6,15,16) and have shown predominant non-cardiac causes of readmissions. Our data are consistent with these findings but extend them to up to a 3-year follow-up period. Moreover, one advantage of our study is that the causes of readmissions were individually adjudicated which is a limitation in other studies.
Given the observation that non-cardiac readmission is a significant issue among post-TAVR patients, it is increasingly relevant for those involved in the evaluation of such patients to be attuned to the important non-cardiac issues, particularly in the highest risk patients. Patient baseline co-morbidities are an important consideration and play an ever-increasing role in patient selection and outcomes. In patients with end-stage renal disease who underwent TAVR, readmissions within 30 days was ~18.9% with significant post-procedure complications and 6-month mortality (25.6%) (17) which is greater than that seen in our mixed cohort (9.5% were dialysis dependent) (Table 1) All-cause mortality was found to be higher in patients with moderate to severe chronic lung disease despite improvement in functional class and quality of life (18) after TAVR which is an important consideration given that 12.5% of our population had severe lung disease. Cirrhotic patients showed readmission rates of ~16.2% with the majority of readmissions due to non-cardiac causes (85.7%) (19). Our data has shown that overall the most common non-cardiac causes of readmissions are due to sepsis/infection, gastrointestinal and respiratory causes.
Our data are consistent with previous findings of a preponderance of non-cardiac readmissions during early (<30 days) (2,6,7), and late (30 days to 1-year) (6,15,16) follow-up. Non-cardiac readmissions were predominant up to 3-year post-TAVR. Our data are unique in that we examined post-TAVR outcomes beyond 30-days to up to 3-year post procedure. The high incidence of noncardiac readmissions throughout this period is likely reflective of the advanced age and baseline comorbidities of the patients undergoing TAVR. This provides useful insight when informing patients of subsequent risks and projected outcomes.
There has been considerable change in the TAVR landscape over the past few years with improvements in TAVR technology, increased expertise, more high-volume centers (20), and wider selection of patients with less comorbidities. Since the advent of the SURTAVI (21) and PARTNER-2 intermediate risk trial (22), The United States Food and Drug Administration has expanded the use of TAVR for patients with severe aortic stenosis with intermediate surgical risk for surgical aortic valve replacement. This will potentially lead to including more patients with fewer comorbidities. Given the timeframe within which the present study performed these TAVR procedures, a high proportion of patients were of higher or prohibitive surgical risk as evidenced by the STS-PROM risk. Consequently, the evolving criteria for TAVR-eligible patients will lead to a shift of the characteristics of this population and future analyses will likely show better outcomes. Our analysis provides an important baseline comparator against which future studies could measure long-term outcomes following TAVR in the more modern era.
One advantage of our study is that all readmissions were adjudicated through the electronic medical records to determine the accuracy of the primary readmission diagnosis. 19 (1.7%) of the 1,123 readmissions were erroneously categorized. The primary readmission diagnosis was recategorized from noncardiac to cardiac in 12 of the readmissions.
The examination of both non-ICU and ICU readmissions after TAVR and their association with mortality has not been previously evaluated. Our analysis included instantaneous hazard function estimates for readmissions and mortality. There was an early high hazard phase with the highest risk for noncardiac readmissions immediately after the procedure which steadily declined thereafter. Overall, noncardiac readmissions were as high as 4.6%/month and declined to 0.7%/month by three years. In contrast, cardiac readmissions did not exhibit an early hazard phase and were stable over this time period. When comparing this with instantaneous hazard function estimates for mortality, there is a similar early hazard phase that coincides with the high non-cardiac readmission rate. One potential explanation is that there is a higher mortality associated with these early non-cardiac readmissions due to the patients’ baseline comorbidities. This will lead to an observed decrease in noncardiac readmissions because of mortality in this cohort due to competing risk. Mortality was higher for patients who had any type of readmission when compared to TAVR patients who were not readmitted. It is evident that mortality is highest amongst those TAVR patients who are readmitted to the ICU. Another important use of these observations is that it suggests that there may be opportunities to pay greater attention and divert more healthcare resources to patients who may have high risk for preventable readmissions. However, that will require further study.
It is important to consider the financial and economic burden of repeated admissions. Although TAVR costs were found to decrease over time while surgical replacement remained stable, aggregate costs of TAVR were significantly higher and dis not account for repeated readmissions (23).
Healthcare providers caring for TAVR patients should be cognizant of the many noncardiac issues that require a multidisciplinary approach for management. These comorbidities are significant factors not only in the pre-TAVR assessment but also ongoing care of the post-TAVR patient. Our study emphasizes the higher noncardiac readmission rates as well as increased mortality shortly after TAVR and after any readmission. This highlights the importance of robust discharge protocols and more intensive follow up and surveillance especially immediately after TAVR and after readmissions.
Limitations
There are limitations to our study which include the inherent drawbacks of any retrospective chart review. Despite adjudication of readmissions, categorization of primary readmission diagnosis was dependent on information available in the medical chart, however, we were encouraged by the consistent admissions diagnosis reporting of billing codes after chart review. Mortality data was obtained from the Social Security Death Index which does not provide detailed information regarding the cause of death.
We studied patients who had undergone TAVR at a quaternary referral center and affiliated hospitals. Our data does not include readmissions in hospitals outside the system, however many of these patients are subsequently transferred to our health care system. Given the size of our healthcare system within Western Pennsylvania we believe this represents a small proportion of the patient population.
The role of TAVR has expanded to include patients with intermediate risk and has shown similar 5-year outcomes to surgical aortic valve replacement (24). More recent trial have shown patients with aortic stenosis and low surgical risk having improved one year outcomes compared to surgery (25,26). With this ever-changing landscape it is unclear what the role of readmissions will play.
Another limitation of our study is the lack of details on subsequent discharge location [discharged home (self-care) or to nursing facilities] which could play a role in readmissions and mortality. Most of our patients were higher surgical risk patients with advanced age and baseline comorbidities. In light of changing cohorts referred for TAVR we expect lower non cardiac readmissions, but it is unclear whether cardiac readmissions will be more prevalent. High noncardiac readmissions may not be as prominent in intermediate risk patients who undergo TAVR. Future studies looking at readmissions in this patient population are warranted.
Conclusions
In a cohort of TAVR patients, non-cardiac readmissions were more prevalent than cardiac readmissions which persisted up to three years post procedure. The risk of readmission and mortality is highest immediately post-procedure and declines thereafter. Readmission to the ICU portends the highest risk of subsequent death in this cohort. Patient baseline co-morbidities are an important consideration for TAVR patients and play a significant role in readmissions and outcomes.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://dx.doi.org/10.21037/cdt-20-916
Data Sharing Statement: Available at https://dx.doi.org/10.21037/cdt-20-916
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/cdt-20-916). Dr. Mulukutla reports funding for Biostatistics Core (unrelated to this project), and serving on Advisory Board (unrelated to this project). Ibrahim Sultan reports Research support from Medtronic. Investigator initiated, and research grant from AtriCure (no personal fees). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the UPMC Institutional Review Board Committee (No. 18120143) with a waiver of individual consent due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holmes DR Jr, Brennan JM, Rumsfeld JS, et al. Clinical outcomes at 1 year following transcatheter aortic valve replacement. JAMA 2015;313:1019-28. [Crossref] [PubMed]
- Kolte D, Khera S, Sardar MR, et al. Thirty-Day Readmissions After Transcatheter Aortic Valve Replacement in the United States: Insights From the Nationwide Readmissions Database. Circ Cardiovasc Interv 2017;10:e004472 [Crossref] [PubMed]
- Grover FL, Vemulapalli S, Carroll JD, et al. 2016 Annual Report of The Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. J Am Coll Cardiol 2017;69:1215-30. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017;70:252-89. [Crossref] [PubMed]
- Forcillo J, Condado JF, Binongo JN, et al. Readmission rates after transcatheter aortic valve replacement in high- and extreme-risk patients with severe aortic stenosis. J Thorac Cardiovasc Surg 2017;154:445-52. [Crossref] [PubMed]
- Nombela-Franco L, del Trigo M, Morrison-Polo G, et al. Incidence, Causes, and Predictors of Early (≤30 Days) and Late Unplanned Hospital Readmissions After Transcatheter Aortic Valve Replacement. JACC Cardiovasc Interv 2015;8:1748-57. [Crossref] [PubMed]
- Danielsen SO, Moons P, Sandven I, et al. Thirty-day readmissions in surgical and transcatheter aortic valve replacement: A systematic review and meta-analysis. Int J Cardiol 2018;268:85-91. [Crossref] [PubMed]
- Roch A, Wiramus S, Pauly V, et al. Long-term outcome in medical patients aged 80 or over following admission to an intensive care unit. Crit Care 2011;15:R36. [Crossref] [PubMed]
- Frost SA, Davidson PM, Alexandrou E, et al. Unplanned admission to the intensive care unit in the very elderly and risk of in-hospital mortality. Crit Care Resusc 2010;12:171-6. [PubMed]
- Wunsch H, Guerra C, Barnato AE, et al. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA 2010;303:849-56. [Crossref] [PubMed]
- Campbell AJ, Cook JA, Adey G, et al. Predicting death and readmission after intensive care discharge. Br J Anaesth 2008;100:656-62. [Crossref] [PubMed]
- Guidet B, Leblanc G, Simon T, et al. Effect of Systematic Intensive Care Unit Triage on Long-term Mortality Among Critically Ill Elderly Patients in France: A Randomized Clinical Trial. JAMA 2017;318:1450-9. [Crossref] [PubMed]
- Otto CM, Kumbhani DJ, Alexander KP, et al. 2017 ACC Expert Consensus Decision Pathway for Transcatheter Aortic Valve Replacement in the Management of Adults With Aortic Stenosis: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol 2017;69:1313-46. [Crossref] [PubMed]
- Miller DC, Blackstone EH, Mack MJ, et al. Transcatheter (TAVR) versus surgical (AVR) aortic valve replacement: occurrence, hazard, risk factors, and consequences of neurologic events in the PARTNER trial. J Thorac Cardiovasc Surg 2012;143:832-843.e13. [Crossref] [PubMed]
- Franzone A, Pilgrim T, Arnold N, et al. Rates and predictors of hospital readmission after transcatheter aortic valve implantation. Eur Heart J 2017;38:2211-7. [Crossref] [PubMed]
- Arai T, Yashima F, Yanagisawa R, et al. Hospital readmission following transcatheter aortic valve implantation in the real world. Int J Cardiol 2018;269:56-60. [Crossref] [PubMed]
- Szerlip M, Kim RJ, Adeniyi T, et al. The outcomes of transcatheter aortic valve replacement in a cohort of patients with end-stage renal disease. Catheter Cardiovasc Interv 2016;87:1314-21. [Crossref] [PubMed]
- Crestanello JA, Popma JJ, Adams DH, et al. Long-Term Health Benefit of Transcatheter Aortic Valve Replacement in Patients With Chronic Lung Disease. JACC Cardiovasc Interv 2017;10:2283-93. [Crossref] [PubMed]
- Dhoble A, Bhise V, Nevah MI, et al. Outcomes and readmissions after transcatheter and surgical aortic valve replacement in patients with cirrhosis: A propensity matched analysis. Catheter Cardiovasc Interv 2018;91:90-6. [Crossref] [PubMed]
- Khera S, Kolte D, Gupta T, et al. Association Between Hospital Volume and 30-Day Readmissions Following Transcatheter Aortic Valve Replacement. JAMA Cardiol 2017;2:732-41. [Crossref] [PubMed]
- Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or Transcatheter Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2017;376:1321-31. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or Surgical Aortic-Valve Replacement in Intermediate-Risk Patients. N Engl J Med 2016;374:1609-20. [Crossref] [PubMed]
- Goldsweig AM, Tak HJ, Chen LW, et al. Relative Costs of Surgical and Transcatheter Aortic Valve Replacement and Medical Therapy. Circ Cardiovasc Interv 2020;13:e008681 [Crossref] [PubMed]
- Makkar RR, Thourani VH, Mack MJ, et al. Five-Year Outcomes of Transcatheter or Surgical Aortic-Valve Replacement. N Engl J Med 2020;382:799-809. [Crossref] [PubMed]
- Mack MJ, Leon MB, Thourani VH, et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N Engl J Med 2019;380:1695-705. [Crossref] [PubMed]
- Gonzales H, Douglas PS, Pibarot P, et al. Left Ventricular Hypertrophy and Clinical Outcomes Over 5 Years After TAVR: An Analysis of the PARTNER Trials and Registries. JACC Cardiovasc Interv 2020;13:1329-39. [Crossref] [PubMed]






