Revascularization strategies in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease: urgent or staged?
Approximately 50% of patients with ST-segment elevation myocardial infarction (STEMI) who undergo primary percutaneous coronary intervention (PCI) have multivessel (MV) coronary artery disease (CAD) (1). These patients have higher risk of mortality in comparison with patients with single vessel CAD.
Up to date, several retrospective studies and few randomized trials have compared the different strategies of revascularization of these patients (Table 1), including: (I) infarct-related artery (IRA)-only PCI; (II) single procedure MV-PCI; and (III) staged MV-PCI, defined as PCI limited to the IRA during the index procedure followed by planned PCI of significant non-IRA lesions at a different time. However, most randomized trials were either underpowered for comparing the three revascularization strategies or compared only one type of complete revascularization. Therefore, up to 15 meta-analysis (6-20) have been conducted in order to clarify this issue (Figure 1), concluding most of them that complete revascularization is associated to a reduced need of new revascularizations, although no clear benefit of revascularization strategy respect to another one in terms of mortality has been demonstrated thus far.
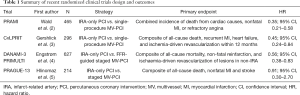
Full table
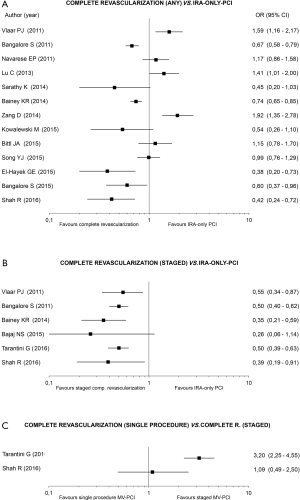
To solve this question, Tarantini et al. (7) conducted a pairwise and network meta-analysis of the three PCI strategies in patients with STEMI and MV disease. They identified 13 prospective and 19 retrospective studies including 54,148 patients. As result, there were 18 comparisons for IRA-only PCI versus single procedure MV-PCI; 15 comparisons for IRA-only versus staged MV-PCI; and nine comparisons for staged MV-PCI versus IRA-only PCI. The primary outcome of the meta-analysis was all-cause mortality. The researchers stratified the outcomes on pooled short-term mortality and pooled long-term mortality. In the pooled short-term mortality analysis, staged MV-PCI was associated with lower mortality in comparison with IRA-only PCI (1.9% vs. 4.9%, P=0.02), and in comparison with single-procedure MV-PCI (1.4% vs. 5.6%, P<0.001). IRA-only PCI was associated with lower mortality in comparison with single-procedure MV-PCI (4.9% vs. 6.9%, P=0.004). In the pooled long-term mortality analysis, lower mortality was shown in the staged MV-PCI strategy versus IRA-only PCI (4.1% vs. 6.8%, P=0.001) and in comparison with single-procedure MV-PCI (3.1% vs. 8.5%, P<0.0001). IRA-only PCI was associated with lower mortality in comparison with single-procedure MV-PCI (6.9% vs. 8.0%, P=0.04). The profit of staged MV-PCI continued after excluding patients with cardiogenic shock in comparison with both IRA-only and single-procedure MV-PCI, but no differences were found between IRA-only PCI and single-procedure MV-PCI.
Notably, this meta-analysis is the first to show that a staged MV-PCI is superior to a single-procedure MV-PCI in terms of mortality. However, as acknowledged by the researchers, many of the studies included were retrospective, and the decision to perform any strategy was driven by local and operator practice. Unfortunately, this conclusion, which would represent excellent news for the interventional community considering the complexity of MV-PCI in the setting of a STEMI, has not been confirmed by other recent meta-analysis that used only data from randomized clinical trials. Indeed, Shah et al. (8), using data from nine randomized trials conclude that MV-PCI either during primary PCI or as an staged procedure resulted in lower occurrences of major adverse cardiac events, revascularization, and cardiovascular mortality than IRA-only PCI. Because single-procedure MV-PCI also resulted in lower rates of recurrent myocardial infarction, they recommended single-procedure MV-PCI as the most efficacious revascularization strategy of the 3. Altogether, the meta-analyses performed by Tarantini et al. (7) and Shah et al. (8) are in agreement with a recent update of the American College of Cardiology and American Heart Association guidelines for patients with STEMI, that recommended complete revascularization (either at the index procedure or as a staged procedure) as a class IIB indication.
Of note, single-procedure MV-PCI may be associated to several advantages. First, it may increase myocardial salvage by increasing perfusion to watershed areas by relieving flow limiting stenosis in the non-IRA. Second, it is associated to lower rates of recurrent myocardial infarction by stabilizing other bystander vulnerable plaques. Third, it may reduce vascular complications from repeated vascular punctures which are required in a staged MV-PCI. Finally, it may be cost-effective by reducing the need of new devices in staged procedures as well as repeated hospitalizations. By contrast, as compared to staged MV-PCI, single-procedure MV-PCI may be associated to some disadvantages such as: (I) the use of high contrast volume, therefore increasing the risk of contrast-induced nephropathy and heart failure; (II) the use of high radiation dose; (III) operator fatigue, especially in working off-hours, may increase the risk of procedural complications.
In conclusion, given that a complete revascularization approach seem to improve survival, the question remaining to be answered by appropriately designed and powered clinical trials is when, not whether, complete revascularization should be performed.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Deora S, Kumar T, Ramalingam R, et al. Demographic and angiographic profile in premature cases of acute coronary syndrome: analysis of 820 young patients from South India. Cardiovasc Diagn Ther 2016;6:193-8. [Crossref] [PubMed]
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115-23. [Crossref] [PubMed]
- Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963-72. [Crossref] [PubMed]
- Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665-71. [Crossref] [PubMed]
- Hlinomaz O. Multivessel coronary disease diagnosed at the time of primary PCI for STEMI: complete revascularization versus conservative strategy: the Prague 13 trial. Available online: multivessel-coronary-disease-diagnosed-at-the-time-of-primary-pci-for-stemi-complete-revascularisation-versus-conservative-strategy-the- prague-13-trialhttp://www.Pcronline.Com/lectures/2015/
- Vlaar PJ, Mahmoud KD, Holmes DR Jr, et al. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction: a pairwise and network meta-analysis. J Am Coll Cardiol 2011;58:692-703. [Crossref] [PubMed]
- Tarantini G, D'Amico G, Brener SJ, et al. Survival After Varying Revascularization Strategies in Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease: A Pairwise and Network Meta-Analysis. JACC Cardiovasc Interv 2016;9:1765-76. [Crossref] [PubMed]
- Shah R, Berzingi C, Mumtaz M, et al. Meta-Analysis Comparing Complete Revascularization Versus Infarct-Related Only Strategies for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease. Am J Cardiol 2016;118:1466-72. [Crossref] [PubMed]
- Bajaj NS, Kalra R, Patel N, et al. Comparison of Approaches for Stroke Prophylaxis in Patients with Non-Valvular Atrial Fibrillation: Network Meta-Analyses of Randomized Controlled Trials. PLoS One 2016;11:e0163608. [Crossref] [PubMed]
- Lu C, Huang H, Li J, et al. Complete versus culprit-only revascularization during primary percutaneous coronary intervention in ST-elevation myocardial infarction patients with multivessel disease: a meta-analysis. Kaohsiung J Med Sci 2013;29:140-9. [Crossref] [PubMed]
- Navarese EP, De Servi S, Buffon A, et al. Clinical impact of simultaneous complete revascularization vs. culprit only primary angioplasty in patients with st-elevation myocardial infarction and multivessel disease: a meta-analysis. J Thromb Thrombolysis 2011;31:217-25. [Crossref] [PubMed]
- Zhang D, Song X, Lv S, et al. Culprit vessel only versus multivessel percutaneous coronary intervention in patients presenting with ST-segment elevation myocardial infarction and multivessel disease. PLoS One 2014;9:e92316. [Crossref] [PubMed]
- Song YJ, Shin HC, Yang JI, et al. Preventive versus culprit-only percutaneous coronary intervention in ST-elevation myocardial infarction patients with multivessel disease: a meta-analysis. J Interv Cardiol 2015;28:1-13. [Crossref] [PubMed]
- Sarathy K, Nagaraja V, Kapur A, et al. Target-vessel versus multivessel revascularisation in ST-elevation myocardial infarction: a meta-analysis of randomised trials. Heart Lung Circ 2015;24:327-34. [Crossref] [PubMed]
- Kowalewski M, Schulze V, Berti S, et al. Complete revascularisation in ST-elevation myocardial infarction and multivessel disease: meta-analysis of randomised controlled trials. Heart 2015;101:1309-17. [Crossref] [PubMed]
- Bangalore S, Toklu B, Wetterslev J. Complete versus culprit-only revascularization for ST-segment-elevation myocardial infarction and multivessel disease: a meta-analysis and trial sequential analysis of randomized trials. Circ Cardiovasc Interv 2015;8:e002142. [Crossref] [PubMed]
- Bittl JA, Tamis-Holland JE, Lang CD, et al. Outcomes after multivessel or culprit-Vessel intervention for ST-elevation myocardial infarction in patients with multivessel coronary disease: a Bayesian cross-design meta-analysis. Catheter Cardiovasc Interv 2015;86 Suppl 1:S15-22. [Crossref] [PubMed]
- Bainey KR, Mehta SR, Lai T, et al. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J 2014;167:1-14.e2. [Crossref] [PubMed]
- Bangalore S, Kumar S, Poddar KL, et al. Meta-analysis of multivessel coronary artery revascularization versus culprit-only revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease. Am J Cardiol 2011;107:1300-10. [Crossref] [PubMed]
- El-Hayek GE, Gershlick AH, Hong MK, et al. Meta-Analysis of Randomized Controlled Trials Comparing Multivessel Versus Culprit-Only Revascularization for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Disease Undergoing Primary Percutaneous Coronary Intervention. Am J Cardiol 2015;115:1481-6. [Crossref] [PubMed]


