The specialty of pulmonary vascular medicine in China: Peking University’s emerging discipline
Pulmonary vascular diseases (PVD) refer to a series of pulmonary circulation disorders whose main manifestations are similar to respiratory diseases. They include various primary or secondary diseases as well as syndromes involving the pulmonary circulation. Apart from primary PVD, lesions related to the left and right heart as well as lung parenchyma may also affect anatomy and function of the pulmonary vascular system. Such diseases are featured by high incidence and disability rate along with sudden death rate, making them the most closely watched diseases worldwide in the past 10 years. In most cases, patients with severe PVD eventually die from acute right heart failure and chronic pulmonary hypertension (PH). Those who manage to pull through will yet suffer from severely impaired cardiopulmonary function, leading to poor living quality. Due to the fact that patients suffering from PVD are widely dispersed in departments of cardiology, respiratory, rheumatoid immunology, hematology, nephrology, obstetrics and many others, there is a lack of unified management, which makes the disease difficult to treat. The growing need for treatment cries out for establishment of the pulmonary vascular discipline, which would in turn improve patients’ prognosis.
The present state of PVD discipline in China
During the past few decades, attention paid on the PVD discipline has experienced rapid growth, resulting in its gradual evolution into a separate medical specialty. China’s recent progress on PVD mainly derives from three centers, each possessing its own features.
First of all is the national PVD center oriented from cardiology in Fuwai Hospital, Chinese Academy of Medical Sciences, which was founded by Professor Xiansheng Cheng, and enhanced by Professor Zhicheng Jing. Having a history of over 60 years, the center focuses on all kinds of PVDs and PH related to cardiovascular lesions. Due to prominent achievements, the Fuwai PVD center is perceived as the origin and leading team of pulmonary vascular discipline in China.
Beyond that, the PVD center in Beijing Chao-yang Hospital and Sino-Japanese Friendship Hospital, Ministry of Health set up by Professor Wang Chen bases its research on respiratory medicine. The center is characterized by its study on comprehensive treatment of pulmonary embolism (PE). Furthermore, Professor Wang Chen’s team is known as a representative of the internationalization of China’s PVD prevention in Pulmonary Vascular Research Institute (PVRI).
Peking University Youth League on PVD Prevention (PUYLPP), founded by Professor Hua Luo, aims to promote the comprehensive development of pulmonary vascular discipline on the basis of critical care medicine (CCM). Integrating clinical practice, research, and education as a whole, Luo’s team is characterized by multidisciplinary comprehensive treatment (MTD) of severe PVDs. PUYLPP is striving to become a model for PVD prevention reform in PVRI.
The establishment of PUYLPP
In 2001, Professor Dayi Hu, a famous cardiovascular expert and medical educator from PKU, began establishing the international PVD platform on the Great Wall International Cardiovascular Conference (1), which subsequently prompted all cardiologists in China to pay extensive attention on PVD. As a result, it laid the foundation for the development of pulmonary vascular science in Peking University Health Science Center (PKUHSC). With the support of well-known professors including Dayi Hu, Chaoshu Tang, Yong Huo, Junbao Du, and Youzhong An, Professor Hua Luo set up PUYLPP in 2012. As a college academic organization consisting of students, young physicians and experienced professors from PKU, PUYLPP intends to promote the prevention, treatment, patient management, and innovative education of PVD in China.
Despite having only 6 years of academic development, PUYLPP is dedicated to the research and construction of pulmonary vascular medicine as an independent discipline. Given that PVD involve various types of complicated lesions and critical illnesses, PUYLPP forms a multidisciplinary team based on CCM and absorbs the quintessence from various specialties. On account of its novel ideas and unique advantage, PUYLPP is making efforts to establish an independent discipline as well as a comprehensive PVD center with Chinese characteristics. It not only focuses on clinical work and scientific research, but also takes education as a breakthrough point. On the one hand, PUYLPP absorbs medical students and young doctors as the main force and backbone of primary prevention, which helped to turn the Chinese Student Association on PVD Prevention (CSAPP) along with the only PVD professional website in China into reality. On the other hand, it designed a series of PVD full-time online education programs for MDT doctors in China. PUYLPP’s effort paid off by achieving remarkable success in popularizing rudimentary knowledge concerning disease and health among patients.
Achievements of PUYLPP
Having gone through its initial phase, PUYLPP has already reached a rapid development stage. Its achievements in the past five years are mainly reflected in the aspects of clinical practice, scientific research and education.
Clinical practice
With regard to the clinical aspect, PUYLPP’s backbone members have accumulated rich experience in the tertiary prevention of PVD.
Given that 22–29% of the patients diagnosed with DVT may result in fatal PE, early prevention is considered to be of great significance (2). In 2001, Dr. Houshan Lv and Dr. Zhenpeng Guan from department of orthopedics, Peking University People’s Hospital, conducted the largest perioperative pulmonary thromboembolism prevention study in Asia. They carried out an average 3.5 years of follow-up among 309 patients who underwent joint surgeries. As a result, the two doctors developed a formula related to six primary indicators which predicts postoperative DVT possibilities (age, number of joints undergoing surgery, AST, Cr, PT, D-dimer ration) (3). The study has a profound effect on the development of clinical diagnosis and treatment, being widely acclaimed as a precursor and outstanding representative of the standardized surgical anticoagulation for the primary prevention of PVD in China.
In recent years, studies have shown that compared with idiopathic disorders, PH associated with connective tissue disease (CTD-PAH) show worse clinical symptoms and weaker response to targeted drugs. As a result, CTD-PAH leads to higher death rates (4). Professor Zhuoli Zhang and Professor Yanjie Hao from the Rheumatology Department, Peking University First Hospital, were the first clinicians to carry out a CTD-PAH clinic. Furthermore, they are the initiators of PHA project on Patients Leadership Training in China. It serves as a model of patient management, standardized treatment, and PVD secondary prevention in comprehensive hospitals.
Another significant achievement of PUYLPP in the aspect of secondary prevention comes from a clinical investigation on plateau diseases. Chronic high altitude heart disease (HAHD) refers to the increase of pulmonary circulation resistance caused by insufficient oxygen supply as well as other natural environment factors (5). This phenomenon is particularly common among plateau residents, resulting in PAH and myocardial anoxia. Dr. Chi Ren Dawa gained his doctorate’s degree in PKU in 2008, and is now working at the department of cardiology, People’s Hospital of Tibet Autonomous Region. Specialized in altitude sickness, he carried out a clinical trial on HAHD which covered 99 admitted patients, along with 50 patients without definite organic diseases acting as the control group. Most patients were residents living on the Tibet Plateau, 3,000 meters above sea level, therefore making the study’s perspective unique in the world. Results showed that thickness of the anterior right ventricular wall, inner diameter of right ventricular inner diameter and right ventricular outflow tract, together with interventricular septum thickness of patients with moderate and severe PH all increased significantly compared with the control group. Besides, left heart structure and function showed a slight degree of abnormality (6). Dr. Chi Ren Dawa’s finding provides clinical basis for early diagnosis and intervention of chronic HAHD.
It is generally held that left heart failure, such as mitral regurgitation, may lead to severe PH (7). Traditional therapies, often referred to thoracotomy, may to a certain extent relieve left cardio-associated PH. Nevertheless, surgeries turn out to be traumatic and costly. The EVEREST study (Endovascular Valve Edge-to-Edge Repair of Mitral Regurgitation) concluded that in terms of safety, percutaneous treatment turned out to be superior to surgery (8). Treating complicated heart diseases by interventional minimal invasive technique may also significantly reduce the incidence and mortality of PH; hence it has become a trend of the third stage prevention of cardio-associated PVD. Professor Yong Huo from the Department of Cardiology, Peking University First Hospital became the first clinician to complete a percutaneous ventricular reconstruction surgery in China (9). With the increasing number of patients receiving interventional cardiovascular surgeries, Professor Wei Ma, a member of Professor Huo’s team, completed a follow-up investigation covering 31 patients who were successfully implanted with left ventricular isolation device. Although no statistically significant difference lied in the clinical data (P>0.05), index related to PH such as left ventricular end-diastolic volume index, median of NYHA classification, index of Minnesota heart failure in the quality of life, 6 minutes’ walking distance test, LVEF, and other key indicators of the patents all showed improvement (10). Interventional therapy is believed to become an effective therapy for secondary prevention of PVD patients in China.
Professor Hua Luo from Peking University Shenzhen Hospital established the normal professional platform of PVD in Peking University in 2009. Soon afterwards in 2012, he founded the first subspecialty of severe PVD in China, making a prospective and predictive discussion for the tertiary prevention of PVD. In 2015, Professor Hua Luo proposed the Bundle & Score therapy for PH crisis, which turned out to be a very innovative treatment (Table 1). Meanwhile, it is considered to be useful for improving clinical practice (http://www.pkupvd.com/article-6553557-1.html).
Overall, the above-mentioned progresses are at the vanguard of cutting edge PVD practice in China. Achievements in clinical field form the basis for large-scale clinical trials, which is a key step for PUYLPP to build up its patient database. The previous work will prove to be essential for making further advance in clinical research.
Scientific research
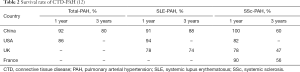
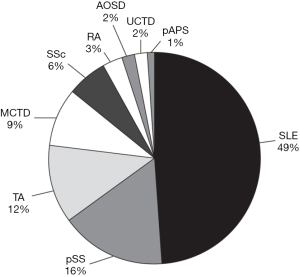
In the realm of scientific research, Professor Yanjie Hao conducted a study on the baseline characteristics and prognosis concerning large samples of connective tissue disease-associated PAH in 2014. The clinical data of 129 patients confirmed by right cardiac catheter was collected. Professor Hao pointed out that SLE-PAH accounts for the largest proportion of all CTD-PAH in China (about 50%). This phenomenon may be attributed to the higher morbidity of SLE in China, compared with western countries (Figure 1). As thus, it results in an apparent difference between the diagnosis and treatment of CTD-PAH in China and that of Europe and the United States (12). The survival rate of different CTD-PAH summarized from Professor Hao’s research is shown in Table 2.
In terms of diagnosis and treatment, Professor Zhang proposed that studies on targeted immunotherapy are likely to provide novel therapeutic strategies for CTD-PAH. Their research filled the gap in China’s research on CTD-PAH and became the first SCI clinical paper on PVD in the PKU team.
In 2015, Dr. Hua Luo designed a trial to analyze the diagnosis, treatment status and influencing factors on severe PVD in Shenzhen. Having nearly 1,000 patients selected, the trial turned out to be the first large-scale follow-up study in PUYLPP. In 2016, college student Gang Huang from PKUHSC completed China’s first undergraduate epidemiological investigation on PVD under the guidance of Dr. Luo. He designed the investigation in order to discover the social factors affecting the prognosis of PAH. Gang Huang carried out a follow up among patients with proven PAH in order to analyze their survival status. His results showed that prognosis of PAH could be affected by economic ability, family support, social aid channels, popularization of disease education, patient compliance, and level of healthcare, respectively. Gang Huang’s investigation stressed the significance of government funding on PVDs, and in the meantime, raised awareness on prevention and education. It won the third prize of college student innovation project in PKUHSC, and was posted on PVRI 2018 international meeting in Singapore.
Professor Junbao Du from Pediatric Department, Peking University First Hospital focuses on the combination of basic medicine with clinical practice.
In 2004, Professor Du designed an experiment that proved the role of H2S in regulation of hypoxic PH and pulmonary vascular reconstruction. The effect of H2S was monitored by the alteration of hemodynamics, pulmonary vascular morphology, and immunohistochemistry. Despite being considered to be a poisonous gas, results concluded that H2S significantly reliefs the symptoms of hypoxic PH by acting as an inhibitor of pulmonary artery smooth muscle cells (PASMC) proliferation (13). Moreover, in 2017 Professor Du conducted a retrospective analysis on 15 patients with methyl malonate diuresis (MMA) whose main manifestations were PH (PAH). He concluded that PAH is a serious complication of MMA, and is more likely to be found in male children. Its clinical manifestations are characterized by hyperventilation, dyspnea, cyanosis, and hypoxemia. In addition, PAH is often accompanied by renal disorders. Timely diagnosis and treatment of MMA together with appropriate anti-PAH treatment can restore normal pulmonary arterial pressure in a short period of time (14).
Education
PUYLPP has made outstanding innovations in the education sphere.
In 2009, Dr. Hua Luo built the first PVD bilingual e-learning website (www.pkupvd.com). It is known to be the first Chinese-English bilingual education platform for PVD in China, serving as a bridge for international communication between Peking University and the world. The establishment of the e-learning website facilitates the displaying of Peking University’s original achievements of studies on PVD and successfully draws attention from both PVRI and PHA. Hence, it laid the foundation for the development of the PVD center in PKU.
In 2012, Jingwen Li, an excellent student member of PUYLPP, assisted Dr. Hua Luo to summarize the first disciplinary history of pulmonary vascular medicine in China. Their summary was published in SCI journal Cardiovascular Diagnosis and Therapy. In the article, Dr. Hua Luo put forward the conception of comprehensive development of pulmonary vascular discipline in Peking University from various aspects including education, clinic and scientific research. In addition, he came up with the idea of building a tertiary prevention network for PVDs in developing countries, which attracted extensive attention from across the world (15).
In 2013, guided by PUYLPP, Dr. Peng Yu from PKUHSC set up the CSAPP. It is perceived as the first student association and public welfare organization on PVD prevention in the world. CSAPP members participate actively in education programs aimed at PVD prevention and treatments (Figure 2). On account of it’s evolving as the backbone of PVD primary prevention in China, outstanding PVRI leader Professor Ghazwan S. Butrous has expressed his expectations for CSAPP to play the role of a demonstration base for international student education on PVDs (Figure 3).
Since 2015, PUYLPP has been responsible for China’s e-learning projects “Diagnosis and therapy in PVD”. Its members have been exploring the path of educational reform in PKUHSC. They gradually summarized a theoretical framework of the discipline of PVDs, which is constituted of six important components (Table 3).
PUYLPP is yet the first to make an attempt on improving the education status in the realm of PVD. Therefore, its efforts in the education field are believed to be one of its predominant features, providing a remarkable template for the development of education in other medical institutions at home and abroad.
Conclusions and outlook
The arising and evolution of an emerging discipline will necessarily promote resource rearrangement as well as the complementary of strengths of traditional disciplines. The discipline of pulmonary vascular is no exception. Facilitating drug discovery as well as the development of PVD from basic research to translational medicine certainly will fill in the blank of secondary prevention drug system, along with targeted anticoagulant delivery system and reverse pulmonary vascular remodeling. As thus, this will help achieve the goal of individualized treatment and precision medicine. Promoting the integration of high technology with new disciplines, and moreover, realizing intelligent management by virtue of intellectualized medical “cloud” database will not only facilitate disease prediction and trend analysis, but also benefit the reduction of high morbidity rates while improving prognosis of the increasing number of patients with PVD.
In the past few years, the pulmonary vascular discipline of PKU has entered a period of rapid development. Having made prominent achievements in several aspects including scientific research, clinic and education, PUYLPP contributed significantly to the discipline construction of PVD in Peking University.
PUYLPP, with its unique perspective in PVD prevention, has gradually attracted attention from abroad, which in turn made it a member of the authoritative organization of PVD. In recent years, PUYLPP keeps on good terms with pulmonary vascular medical institutions and academic association worldwide, meanwhile enhancing academic exchange. Among those institutions are the International institute of PVD, the Cardiovascular Center of Cleveland, the International Association for Pulmonary Hypertension, Johns Hopkins Medical Institutions, the American Heart Association and the Medical Center of UCSD, etc.
Notwithstanding the achievements recently made, a huge gap lays between PUYLPP and other well-known research centers in the world. In view of the fact that PUYLPP is still in its developing stage, expenditure as well as the number of patients admitted annually is far from expectation. In the current state, researchers of PUYLPP might encounter difficulties in carrying out large-scale clinical trials due to the lack of cases. PUYLPP is seeking further development relying on affiliated hospitals of PKU. Therefore, continuous exploration and ongoing effort is required so as to improve the status quo.
Acknowledgements
Our deepest gratitude goes first and foremost to Professor Paul Schoenhagen for his enthusiastic support and guidance in Chinese Medicine. Professor Schoenhagen’s efforts have promoted the development of pulmonary vascular medicine in China. Besides, we would like to extend our appreciation to European Respiratory Journal for providing us with the chart displaying predisposing factors of CTD-PAH in China.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chu X, Hu D. Building a Great Wall against cardiovascular disease. Chinese Journal of Cardiovascular Review 2003;2:158-60.
- Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004;126:338S-400S. [Crossref] [PubMed]
- Fei Z, Guan Z, Guo W, et al. Preoperative multivariate analysis of risk factors for deep vein thrombosis after hip and knee arthroplasty. Orthopedic Journal of China 2012;20:1001-5.
- Shahane A. Pulmonary hypertension in rheumatic diseases: epidemiology and pathogenesis. Rheumatol Int 2013;33:1655-67. [Crossref] [PubMed]
- Li S, Gao Y. Plateau pathology. Beijing: People’s Medical Publishing House, 2006.
- Dawa CR, Norbu K, Zhuoma CR, et al. Effects of pulmonary artery systolic blood pressure on cardiac structure and function in patients with chronic high altitude heart disease. Chin J Cardiol 2013;41:761-5.
- Ling LH, Enriquez-Sarano M, Seward JB, et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417-23. [Crossref] [PubMed]
- Feldman T, Wasserman HS, Herrmann HC, et al. Percutaneous mitral valve repair using the edge-to-edge technique: six-month results of the EVEREST Phase I Clinical Trial. J Am Coll Cardiol 2005;46:2134-40. [Crossref] [PubMed]
- Wang Jinhua. Professor Yong Huo's team from Peking University First Hospital performs the first percutaneous ventricular reconstruction in China. Chin J Front Med Sci 2013;5:50. [Crossref]
- Ma W, Hong T, Li J, et al. Percutaneous ventricular reconstruction. Chin J Interven Cardiol 2013;21:274-6.
- Hua Luo. Comprehensive therapy for pulmonary hypertension crisis. 7th Critical Care Medicine Forum of Peking University, Beijing, August 21, 2015.
- Hao YJ, Jiang X, Zhou W, et al. Connective tissue disease-associated pulmonary arterial hypertension in Chinese patients. Eur Respir J 2014;44:963-72. [Crossref] [PubMed]
- Chen X, Du J, Zhang C, et al. The regulatory effects of new gas signal molecular hydrogen sulfide on hypoxic pulmonary hypertension and pulmonary vascular structure reconstruction. Chin J Pediatr 2004;4:65-6.
- Liu X, Yan H, Qiu J, et al. Clinical characteristics and gene mutation of hypertensive pulmonary hypertension associated with methyl malonate diuresis. J Peking Univ 2017;49:768-77. (Health Sci).
- Luo H, Li J. The specialty of pulmonary vascular medicine in China: historical development and future directions. Cardiovasc Diagn Ther 2012;2:240-5. [PubMed]
- Hua Luo. The development of pulmonary vascular diseases in China: Past, Present and Future. The 26th Great Wall International Congress of Cardiology, Beijing, October 29, 2015.