
Effects of complete revascularization on long-term treatment outcomes in patients with multivessel coronary artery disease over 80 years of age admitted for acute coronary syndrome
Introduction
The number of very elderly patients has dramatically increased in recent years worldwide. According to current predictions, the world’s total number of people aged 80 or older will double by 2050 (1). Treatment of very elderly patients is a serious issue in cardiology practice because of numerous comorbidities, the psychosocial aspects of this age group, and the complex anatomy of the coronary artery system and peripheral vessels in these patients (2). This highlights the need for studies in this patient population.
Besides, a higher percentage of patients in this age group have multivessel coronary artery disease, as compared with younger individuals. A number of studies have demonstrated that multivessel coronary artery disease is associated with poor prognosis (3,4). Earlier studies revealed that complete revascularization (CR) decreased the incidence of ischaemic events in younger subjects (5). However, the impact of complete and incomplete revascularization (ICR) on long-term outcomes in patients over 80 years of age has not been adequately investigated. On the one hand, CR can decrease the rate of ischemic events and subsequent interventions; on the other hand, it is associated with a high risk of renal failure and periprocedural complications. The high risk of complications is due to the complex coronary artery disease and hypersensitivity to contrast media, as well as combined comorbidities, in this age group. Nevertheless, the SHINANO Registry have shown that even in elderly patients over 75 years old, multivessel revascularization appears to suppress mid-term ischemic events, especially in the subgroup of patients presenting with acute coronary syndrome (6). More recently, study by de La Torre Hernandez et al. demonstrated that multi-vessel percutaneous coronary intervention (PCI) was related with better outcomes especially after staged procedures in patients with ST-segment elevation myocardial infarction (MI) over 75 years of age (7). However, the current clinical guidelines recommend an individual approach to patients with multivessel coronary artery disease depending on the patient’s general condition, severity of coronary artery disease, and myocardial involvement (8,9). Thus, the effects of CR on long-term treatment outcomes in patients over 80 years of age with acute coronary syndrome due to multivessel coronary artery disease have not been sufficiently investigated.
Aim
Our objective was to evaluate the outcomes of CR and ICR in patients with multivessel coronary artery disease over 80 years of age, who were admitted for acute coronary syndrome.
Methods
Study population
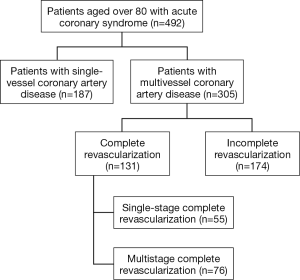
We conducted a prospective cohort analysis of short-term and long-term treatment outcomes obtained in patients with multivessel coronary artery disease over 80 years of age, who underwent a PCI for acute coronary syndrome in the period from January 2014 to August 2017. There were no exclusion criteria in this study. The study was approved by the ethics committee. During the study period, 492 patients aged over 80 had a coronary intervention for acute coronary syndrome. In this study sample, 305 subjects suffered from multivessel coronary artery disease. The patients were divided into two groups: CR was performed in 131 patients, and 174 subjects had intervention on the symptomatic artery only. Fifty-five subjects underwent CR in primary procedure, and 76 patients had CR in staged procedure (Figure 1). The procedures were performed according to the preferences of each operator.
Primary and secondary endpoints and definitions
The primary endpoint was 1-year occurrence of the major adverse cardiac events (MACE), including death, non-fatal MI, and stroke. We also recorded cases of repeat coronary artery intervention, major bleeding events, contrast-induced nephropathy and stent thrombosis that occurred within a period of 1 year.
Acute coronary syndrome was defined as one of the following events: ST-segment elevation MI, non-ST-segment elevation MI, or unstable angina. ST-segment elevation MI was diagnosed in the presence of anginal pain or its equivalents with an ST segment elevation of at least 1 mV in at least two contiguous leads, newly detected left bundle-branch block, and elevated cardiac specific enzyme levels (a rise of cardiac troponin with at least one value above the 99th percentile upper reference limit). Non-ST-segment elevation MI was diagnosed in the presence of anginal pain or its equivalents and elevated cardiac specific biomarker levels and permanent or temporary ST segment depression, T-wave inversion, short-term ST segment elevation on ECG. Unstable angina was diagnosed in patients with anginal pain at rest or at night. Multivessel coronary artery disease was defined as stenosis of more than 70% in two or more epicardial branches with a diameter exceeding 2 mm. Successful PCI was defined as Thrombolysis in Myocardial Infarction (TIMI) 3 flow in the symptomatic artery and post-interventional residual stenosis <20%. CR was characterized by elimination of hemodynamically important lesions in epicardial coronary arteries with a diameter exceeding 2 mm. A major bleeding event was a gastrointestinal bleeding, access site bleeding, or hemopericardium resulting in cardiac tamponade or transfusion of blood components (BARC 3 according to the Bleeding Academic Research Consortium classification). Contrast-induced nephropathy was diagnosed in patients with renal impairment who had a serum creatinine increase of at least 25% from baseline and/or an absolute elevation in serum creatinine of 0.45 mg/dL 48–72 hours after contrast medium administration.
Statistical analysis
Statistical analyses of study results were performed using the SPSS 24 for Mac application package. Continuous variables were presented as arithmetic means and squared deviations from the mean (М ± σ). Categorical variables were presented as absolute values and percentages of the number of patients in the analyzed group. We compared continuous variables using Student’s t-test or the Wilcoxon signed-rank test based on the distributions. Categorical variables were compared with the help of the chi-square test or Fisher’s exact test. The Kaplan-Meier estimator was employed to evaluate the cumulative probability of achieving the endpoints. Multivariate Cox regression analysis was utilized to determine the death risk coefficients and evaluate the effects of independent variables on this risk. The critical level of statistical significance was set at P<0.05.
Results
Baseline patient characteristics
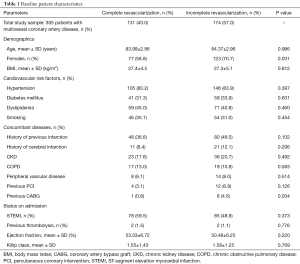
This study enrolled 305 patients with multivessel coronary artery disease over 80 years of age, who had a diagnosis of acute coronary syndrome and underwent a percutaneous coronary intervention. The patients were divided into two groups: CR was performed in 131 patients, and 174 subjects had intervention on the symptomatic artery only. The baseline patient characteristics are included in Table 1. No statistically significant characteristics between the groups were observed. The mean age of patients was 83.99 in the CR group and 84.37 in the ICR group. It should be mentioned that women (CR 58.8% vs. ICR 70.7%, P=0.031) and patients with previous coronary artery bypass graft (CABG) (CR 0.8% vs. ICR 4.6%, P=0.034) prevailed in the ICR group.
Full table
Characteristics of coronary artery disease and PCI
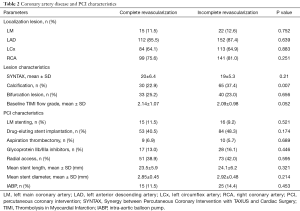
Table 2 shows the characteristics of coronary artery disease and PCI. Lesions were more calcified in the ICR group (CR 22.9% vs. ICR 37.4%, P=0.007). However, we observed no significant differences in the location of stenotic lesions, presence of bifurcation lesions, and lesion severity assessed with the SYNTAX score.
Full table
Analysis of study results and PCI complications
Table 3 summarizes the complications and clinical outcomes of PCI. No significant differences were observed in post-intervention blood flow evaluated with the TIMI grading system or in complications.
Full table
The incidence rates of contrast-induced nephropathy (CR 6.1% vs. ICR 4.6%, P=0.688), stent thrombosis (CR 0.8% vs. ICR 1.7%, P=0.452) and major bleeding events (CR 2.3% vs. ICR 2.3%, P=0.996) did not differ between the groups.
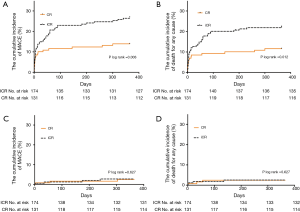
The 1-year incidence of MACE was significantly lower in the CR group than in patients undergoing ICR (CR 14.5% vs. ICR 27.0%, P=0.008). We also observed significant reductions in overall mortality (CR 11.5% vs. ICR 22.4%, P=0.012) and cardiac mortality (CR 9.2% vs. ICR 17.8%, P=0.029) in the CR group. This difference was greatest within the first month after the intervention, but it remained statistically significant throughout the observation period. More detailed data can be seen on the Kaplan-Meier curve presented in Figure 2. The number of repeat interventions was lower in the CR group; however, the difference did not reach statistical significance (CR 2.3% vs. ICR 5.7%, P=0.123).
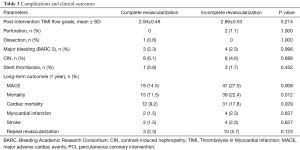
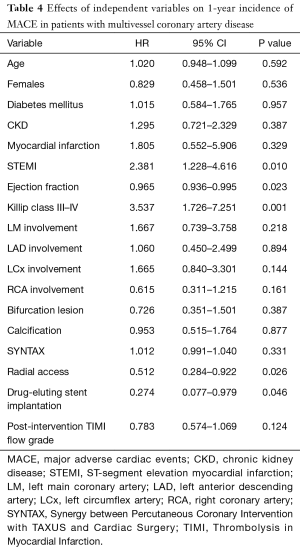
Furthermore, we analyzed independent factors affecting the 1-year incidence of the MACE in the entire sample of patients with multivessel coronary artery disease. The most valuable results are included in Table 4. A number of factors, including ST-segment elevation MI, low ejection fraction, and Killip class III–IV acute heart failure, increase the risk of the MACE. Radial access, the use of drug-eluting stents and CR are associated with a lower risk of MACE.
Full table
Discussion
There is currently contradictory evidence to support the choice of treatment plan for patients with multivessel coronary artery disease. A number of studies have shown that CR during percutaneous coronary interventions is associated with a higher risk of MI compared with stenting of the symptomatic artery alone (10). Other investigators do not report a significant difference between groups of patients undergoing complete or ICR for either ST-segment elevation or non-ST-segment elevation acute coronary syndrome (11,12).
However, a recent meta-analysis demonstrated significant reductions in both total mortality and MI in the CR group. Another interesting finding was that the staged revascularization did not improve these outcomes (13). Besides that, a number of recently published studies mentioned lower mortality and MACE incidence in patients undergoing CR (14-17).
It should also be mentioned that the current guidelines recommend CR for patients with cardiogenic shock (18). However, a recent meta-analysis demonstrated no advantage of CR over intervention on the infarct-related artery in cardiogenic shock (19). These data also agree with the results of the recent CULPRIT SHOCK trial, which demonstrated an increase in the composite endpoint that included death or renal failure within 30 days in the CR group (20).
The authors of studies conducted in elderly patients disagree on the value of CR. It is also reported that the percentage of patients undergoing CR is extremely low, 35–36% (7,21). This percentage was somewhat higher in our study, approximately 43%. Rumiz et al. compared the outcomes of complete and ICR in patients aged under or over 75 years. He concluded that CR had no effect on treatment outcomes in patients over 75 years of age, unlike in younger patients (21). de La Torre Hernandez et al. reported lower mortality and incidence of major coronary events in patients undergoing stenting of all hemodynamically relevant lesions (7). In the reported study, we also obtained a lower MACE rate in patients after CR, despite their severe comorbidities and complex coronary anatomy. These factors, in turn, entail a higher periprocedural risk than in younger patients (22). It should be underlined, however, that we did not obtain a significant increase in the incidence of contrast-induced nephropathy or stent thrombosis in the CR group. ST-segment elevation MI, low ejection fraction, and Killip class III–IV acute heart failure were essential factors that increased the risk of death. These results are also in agreement with the conclusions of other authors, as the studies of Caretta et al. and Kozlov et al. demonstrated that low left ventricular ejection fraction was among the most important independent risk factors of death in patients over 80 years of age (23,24). Another interesting finding was that the use of drug-eluting stents and radial access were associated with a lower risk of MACE. These data confirm the results of other studies that were conducted in elderly patients (7,22). The findings of the XIMA trial are also important. The authors compared the results of using drug eluting stent (DES) and bare metal stent (BMS) in octogenarians. DES were associated with a lower incidence of MI and target vessel revascularization without increased incidence of major hemorrhage. Besides that, of particular interest was the reduction in primary endpoint events with the DES strategy when using the radial artery for access or performing multivessel procedures (25). Notwithstanding the lower incidence of the MACE in the CR group, it should be remembered that a decision on whether to perform CR should be made based on the patient's general condition, the severity and technical feasibility of percutaneous coronary intervention, and cardiovascular risk factors.
Limitations of the study
The main limitations of this study were in its prospective, single-centre, non-randomized design. As a result, some factors affecting the treatment outcome might be underestimated or estimated improperly. Besides that, this type of registries suffers from inherent selection bias. However, our study reflects the actual current clinical practice worldwide and a representative patient sample. As far as we know, this study was conducted in one of the largest groups of patients over 80 years of age with multivessel coronary artery disease who were treated with PCI for acute coronary syndrome, with a significant percentage of them undergoing CR.
Conclusions
Multivessel coronary artery disease is a very common finding in patients aged over 80 years admitted for acute coronary syndrome. CR decreases the incidence of major coronary events, overall mortality and cardiac mortality in this patient group. Complete coronary revascularization can be carried out safely in very elderly patients without increasing the risk of complications. The most important factors increasing the 1-year risk of MACE are ST-segment elevation MI, low ejection fraction, and Killip class III–IV acute heart failure. Radial access, the use of drug-eluting stents and CR are associated with a lower risk of MACE.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Ethics Committee I.M. Sechenov First Moscow State Medical University (Sechenov University) (No. 470p) and informed consent was taken from all the patients.
References
- Mather M, Jacobsen LA, Pollard KM. Aging in the United States. Population Bulletin 2015;70.
- Llaó I, Ariza-Solé A, Sanchis J, et al. Invasive strategy and frailty in very elderly patients with acute coronary syndromes. EuroIntervention 2018;14:e336-42. [Crossref] [PubMed]
- Park DW, Clare RM, Schulte PJ, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA 2014;312:2019-27. [Crossref] [PubMed]
- Toma M, Buller CE, Westerhout CM, et al. Non-culprit coronary artery percutaneous coronary intervention during acute ST-segment elevation myocardial infarction: insights from the APEX-AMI trial. Eur Heart J 2010;31:1701-7. [Crossref] [PubMed]
- Hannan EL, Wu C, Walford G, et al. Incomplete revascularization in the era of drug-eluting stents: impact on adverse outcomes. JACC Cardiovasc Interv 2009;2:17-25. [Crossref] [PubMed]
- Harada M, Miura T, Kobayashi T, et al. Clinical impact of complete revascularization in elderly patients with multi-vessel coronary artery disease undergoing percutaneous coronary intervention A sub-analysis of the SHINANO registry. Int J Cardiol 2017;230:413-9. [Crossref] [PubMed]
- de La Torre Hernandez JM. Multivessel disease in patients over 75years old with ST elevated myocardial infarction. Current management strategies and related clinical outcomes in the ESTROFA MI+75 nation-wide registry. Cardiovasc Revasc Med 2018;19:580-8. [Crossref] [PubMed]
- Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999-3054. [Crossref] [PubMed]
- Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Bauer T, Zeymer U, Hochadel M, et al. Prima-vista multi-vessel percutaneous coronary intervention in haemodynamically stable patients with acute coronary syndromes: analysis of over 4.400 patients in the EHS-PCI registry. Int J Cardiol 2013;166:596-600. [Crossref] [PubMed]
- Pimor A, Auffret V, Didier R, et al. Immediate complete revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease treated by primary percutaneous coronary intervention: Insights from the ORBI registry. Arch Cardiovasc Dis 2018;111:656-65. [Crossref] [PubMed]
- Mariani J, Macchia A, De Abreu M, et al. Multivessel versus Single Vessel Angioplasty in Non-ST Elevation Acute Coronary Syndromes: A Systematic Review and Metaanalysis. PLoS One 2016;11:e0148756. [Crossref] [PubMed]
- Pasceri V, Patti G, Pelliccia F, et al. Complete Revascularization During Primary Percutaneous Coronary Intervention Reduces Death and Myocardial Infarction in Patients With Multivessel Disease: Meta-Analysis and Meta-Regression of Randomized Trials. JACC Cardiovasc Interv 2018;11:833-43. [Crossref] [PubMed]
- Toyota T, Shiomi H, Taniguchi T, et al. Culprit Vessel-Only vs. Staged Multivessel Percutaneous Coronary Intervention Strategies in Patients With Multivessel Coronary Artery Disease Undergoing Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction. Circ J 2016;80:371-8. [Crossref] [PubMed]
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115-23. [Crossref] [PubMed]
- Hawranek M, Desperak P, Gąsior P, et al. Early and long-term outcomes of complete revascularization with percutaneous coronary intervention in patients with multivessel coronary artery disease presenting with non-ST-segment elevation acute coronary syndromes. Postepy Kardiol Interwencyjnej 2018;14:32-41. [Crossref] [PubMed]
- Correia C, Galvão Braga C, Martins J, et al. Multivessel vs. culprit-only revascularization in patients with non-ST-elevation acute coronary syndromes and multivessel coronary disease. Rev Port Cardiol 2018;37:143-54. [Crossref] [PubMed]
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77. [Crossref] [PubMed]
- Kolte D, Sardar P, Khera S, et al. Culprit Vessel-Only Versus Multivessel Percutaneous Coronary Intervention in Patients With Cardiogenic Shock Complicating ST-Segment-Elevation Myocardial Infarction: A Collaborative Meta-Analysis. Circ Cardiovasc Interv 2017;10:005582. [Crossref] [PubMed]
- Thiele H, Akin I, Sandri M, et al. PCI Strategies in Patients with Acute Myocardial Infarction and Cardiogenic Shock. N Engl J Med 2017;377:2419-32. [Crossref] [PubMed]
- Rumiz E, Berenguer A, Vilar JV, et al. Long-term outcomes and predictors of morbi-mortality according to age in stemi patients with multivessel disease: Impact of an incomplete revascularization. Catheter Cardiovasc Interv 2018;92:E512-7. [Crossref] [PubMed]
- Bromage DI, Jones DA, Rathod KS, et al. Outcome of 1051 Octogenarian Patients With ST-Segment Elevation Myocardial Infarction Treated With Primary Percutaneous Coronary Intervention: Observational Cohort From the London Heart Attack Group. J Am Heart Assoc 2016;5:003027. [Crossref] [PubMed]
- Caretta G, Passamonti E, Pedroni P, et al. Outcomes and predictors of mortality among octogenarians and older with ST-segment elevation myocardial infarction treated with primary coronary angioplasty. Clin Cardiol 2014;37:523-9. [PubMed]
- Kozlov KL, Bessonova NA, Yakovlev VV. The development of chronic heart failure in elderly patients with low ejection fraction at baseline in the acute phase of myocardial infarction. Adv Gerontol 2017;30:618-22. [PubMed]
- de Belder A, de la Torre Hernandez JM, Lopez-Palop R, et al. A prospective randomized trial of everolimus-eluting stents versus bare-metal stents in octogenarians: the XIMA Trial (Xience or Vision Stents for the Management of Angina in the Elderly). J Am Coll Cardiol 2014;63:1371-5. [Crossref] [PubMed]


