
The potential for missed work days due to possible COVID-19 exposure at large scientific meetings
On March 9th, the American College of Cardiology (ACC) announced the cancellation of their annual meeting, scheduled to start on March 28th in Chicago, IL, USA, due to concerns regarding coronavirus disease (COVID-19) following rapidly increasing confirmed cases in the United States. Notably, this was the first cancellation of the ACC’s Annual Scientific Session in the last 69 years (1).
The debate leading up to the formal cancellation among attendees, particularly on social media platforms such as Twitter, was rampant with a wide spectrum of views regarding plans to attend. Interestingly, a number of institutions, both private and academic, formally released work-related travel bans for all non-essential travel through the month and beyond. These events and debate raise the question—in the modern hyper-connected world, what is the potential impact of attending a large scientific conference in the setting of an ongoing pandemic?
Let us first consider the Biogen strategic management meeting held in Boston, MA, in late February 2020. The meeting had approximately 175 attendees including both United States and international citizens (2). Following the meeting, multiple attendees developed flu-like symptoms with numerous testing positive for COVID-19. By early March, 70 of 92 confirmed cases of COVID-19 in the state of Massachusetts (or 40% of the meeting attendees) were traced to that meeting (3). In response, Biogen placed all attendees of that meeting in quarantine.
What could the ramifications be if a major specialty medical conference, with ~10,000 expected medical delegates, decided to convene their scheduled meeting? Creating inferences based on reported data from China, Italy, Iran, and other regions which have been rampantly afflicted with COVID-19 outbreaks (4,5), we devised a decision analysis tree, as shown in Figure 1. Based on reported mortality rates ranging from 2% to 3% of all patients diagnosed with COVID-19, we estimated a 50% infection rate among exposed individuals and 10% hospitalization rate among infected individuals with 2% rate of medical leave consisting of 4 weeks or greater. Next, we estimated that among the remaining 90% of attendees who were infected with COVID-19, 80% would develop symptoms requiring self-quarantine for a 2-week period while 20% remain asymptomatic and resume clinical duties with appropriate precautions.
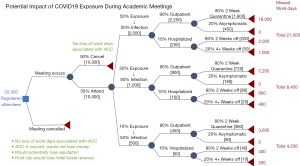
We created three potential scenarios varying from a conservative 10% exposure rate to a more liberal 50% exposure rate with 50% of these individuals becoming infected. Using a 10% exposure rate, approximately 1,000 attendees would be exposed and 500 attendees would be infected. Of these, an estimated 50 attendees would be hospitalized and 10 would require greater than 4 weeks of medical leave. Of the 450 attendees infected but not hospitalized, 360 would be placed in a 2-week quarantine until no longer contagious. Assuming a 5-day work week, this translates to an estimated loss of 4,200 work days, or a cumulative loss of 11.5 work years.
Conversely, using a 50% exposure rate, approximately 5,000 attendees would be exposed and 2,500 attendees would become infected of which 250 would develop symptoms warranting hospitalization and 50 would develop severe symptoms resulting in medical leave of greater than 4 weeks. An estimated 1,800 attendees would be self-quarantined for 2 weeks. In total, this would result in a loss of 21,000 work days, or a staggering 57.5 work years.
Prior to putting these estimations in context, one must consider the inherent uncertainties and limitations in light of the novelty of this virus. One, we attempted to remain conservative with best knowledge of the epidemiology of COVID-19 at each point of the decision tree, including exposure rates, symptom burden, and length of medical leave. Importantly, the true impact would depend on a host of factors, including degree of attendee interaction and prevalence of COVID-19 infection among the cohort. These risks could be mitigated by maintaining appropriate social distancing, hand hygiene, masks, and temperature checks at entry. Second, despite a mortality rate that is non-trivial, we did not account for potential attendee deaths which in our various scenarios could range from 10 to 50 deaths. The repercussions would be dramatic and significantly increase the impact of downstream burden, both psychosocial and economic. Lastly, given a median incubation period of 5 days, another important consideration is the possibility of attendees to exponentially increase the estimated impact by infecting family members, coworkers, and other members of their local community before manifesting symptoms.
The burden of such a significant and simultaneous loss of the physician workforce is impossible to estimate but would certainly have a severe, detrimental impact to every aspect of the healthcare system. First and foremost, the patients whom healthcare providers have dedicated their careers to would be severely lacking in a time when they need them the most. Access to care, already a significant problem in the United States, would be further exacerbated. Moreover, appears that those at highest risk for complications due to COVID-19 are those who have other medical comorbidities, are immunosuppressed, or are elderly (4). The complexity of these patients concomitantly diagnosed with a novel illness likely requires multidisciplinary care with specialist input for unforeseen disease manifestations, further highlighting an “all hands on deck” mentality to take care of a currently unpredictable burden of illness.
Another important consideration is the financial impact of missed work days on the host cities, the scientific organizations and the local the health care organization. While it is impossible to gauge the extent of the host city’s losses, the potential losses for the scientific organization would be significantly mitigated by insuring such large events. However, the potential cost on the health care system can be staggering. In our example, assuming an average annual billing of ~$2,000,000 per physician, may result in ~$25–115 million in lost billing (without taking into consideration the impact on technical revenue). Moreover, there could be significant costs associated with caring for those that require prolonged hospitalizations, including utilization of limited intensive care resources, for a subset of attendees. The impact of these potential losses downstream is difficult to quantify but may be highly significant with long-lasting implications.
The current epidemic of COVID-19 requires everyone—patients, health care workforce, and organizations—to carefully and deliberately make decisions for the greater good. We applaud the various organizations which cancelled their annual meetings for making the safest decision in light of the current crisis. The academic mission, scientific discovery, and collaboration of ideas remains the core of building a better tomorrow in medicine. Perhaps, while initially appearing to stunt that mission, COVID-19 may have opened the doors for an innovative future where conference medium can be virtually spread around the world to all interested parties and thus greatly increase the scientific reach and impact (6).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.6.org/10.21037/cdt-20-418). MYD serves as an unpaid editorial board member of Cardiovascular Diagnosis and Therapy from Feb 2019 to Jan 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Phend C. ACC Meeting Cancelled. MedPage Today, March 9, 2020. Available online: https://www.medpagetoday.com/meetingcoverage/acc/85311
- DeAngelis A. Up to 175 people may have been exposed to coronavirus at Biogen meeting. Boston Business Journal, March 6, 2020. Available online: https://www.bizjournals.com/boston/news/2020/03/06/up-to-175-people-may-have-been-exposed-to.html
- Holcombe M. 70 of 92 coronavirus cases in Massachusetts linked to Biogen employees after biotech firm's Boston meeting. CNN Health, March 11, 2020. Available online: https://www.cnn.com/2020/03/11/health/coronavirus-massachusetts-state-of-emergency/index.html
- Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239-42. [Crossref] [PubMed]
- Mizumoto K, Kagaya K, Zarebski A, et al. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill 2020;25:2000180. [Crossref] [PubMed]
- Kumar A, Patel DR, Nissen SE, et al. Implementing Virtual Innovations During the COVID-19 Pandemic for a Better Tomorrow in Health Care. JACC Case Rep 2020;2:1376-8. [Crossref]


