Direct communication between the left circumflex and the right coronary arteries: a very rare coronary anomaly circulation
Introduction
Coronary artery anomalies (CAA) are a diverse group of congenital disorders, and the pathophysiological mechanisms and manifestations are highly variable. Their incidence ranges from 0.03% to 0.2% of the patients undergoing routine catheterization (1-3). Intercoronary communications (ICC) are a very rare subset of CAA with uni- or bidirectional blood flow between two or more coronary arteries (4). They differ from collateral arteries and fistulas and does not reflect underlying coronary disease (5,6). The real significance of ICC and their consequences are still unknown. Computational fluid dynamics (CFD) in combination with computed tomography angiographic (CTA) images is capable of reproducing flow feature in the aorta and adjacent arteries (7).
We present herein an extremely rare case of a bidirectional ICC between the left circumflex artery (LCx) and the right coronary artery (RCA), without occlusive coronary artery disease, incidentally diagnosed in an urgent coronary angiography due to an acute coronary syndrome.
Case report
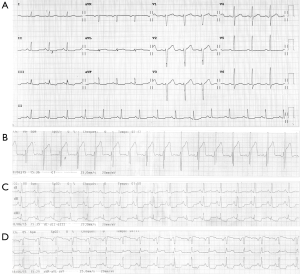
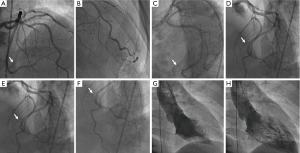
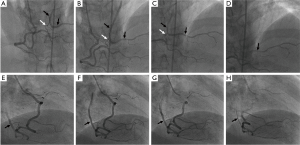
A 58-year-old man, active, with long-term type 2 melitus diabetes, hypertension, dyslipidaemia, former ethanol abuse and chronic amaurosis. There were no previous episodes of myocardial infarction (MI), stroke, coronary artery disease neither personal of familiar histories of sudden cardiac death. During intraocular injection of anesthetic drugs previous to an oftalmologic surgery, he developed a sudden episode of sinus bradycardia and arterial hypotension associated to diaphoresis and signs of low cardiac output, reversed with intravenous atropine. The resting electrocardiogram revealed discreet ST segment elevation in the lateral leads and the mirror ST segment depression in the inferior leads (Figure 1). Despite the absence of acute chest pain, this clinical scenario was sought to be a consequence of an acute MI, the reason why the patient was immediately referred to an urgent coronary angiography, which revealed no significant luminal narrowing or occlusions. Nonetheless and surprisingly, selective injection into the RCA showed retrograde filling of the distal and mid portions of the LCx postero-lateral branch from the distal portion of the RCA (Figures 2-5). Retrograde filling was not related to collaterals, but to a bidirectional direct ICC. Since there were no significant coronary lesions, the patient was managed with optimal medical treatment (ASA 100 mg/d, clopidogrel 75 mg/d, atenolol 100 mg/d, atorvastatin 80 mg/d, enalapril 40 mg/d, metformin 2,000 mg/d). Once stabilized from a clinical standpoint, he was discharged home two days after the index event.


Discussion
CAA are congenital changes in their origin, course, and/or structure. Several controversies remain in terms of their incidence, classification, screening, heredity, and treatment. Despite being mostly asymptomatic, clinical presentation in adults may result from myocardial ischemia, manifesting as angina, syncope, arrhythmias, and even sudden death. In young athletes, apparently healthy, they are the second most frequent cause of sudden death (1,2,10).
ICC are a very rare congenital CAA defined as an open-ended circulation with uni- or bidirectional blood flow between two (or more) coronary arteries (6). They differ from collateral arteries and fistulas by their angiographic features, and do not usually reflect underlying coronary artery disease (5,6).
Compared with collaterals, ICC are larger in diameter (generally >1 mm), extramural, and straight. Furthermore, the histological structure of the connecting vessel has the characteristics of a normal arterial wall, with a well-defined muscular layer (4-6).
Coronary artery fistulas, in turn, are abnormal communications between a coronary artery and a cardiac chamber or major vessel (11). They may be congenital or acquired due to trauma or iatrogenic causes (5).
ICC are rarely seen during coronary angiography in patients with and without coronary artery narrowing (4,6). Yamanaka and Hobbs have reported the incidence of ICC to be 0.002% in a very large study comprising 126,595 patients (12).
Two types of ICC have been reported so far: between left anterior descending and posterior descending arteries in the distal interventricular groove or between the LCX and RCA in the posterior atrioventricular groove (4,12-14), as shown in our case.
The real significance of ICC and their consequences are still unknown. Some authors believe that these connections may play a protective role for the myocardium in case of any significant coronary artery obstruction develops in one of the connecting vessels. In turn, myocardial ischemia can result from the coronary steal phenomenon by the unidirectional flow (4,13). CFD in combination with CTA images is capable of reproducing flow feature in the aorta and adjacent arteries, in order to better understanding of the induced flow alterations (7).
There are several reports of the connection between ICC and spontaneous vasospastic angina. Some authors even advocate that provocation of coronary vasospasm can be useful if ICC without significant coronary obstruction is found in patients with chest pain, in order to document this cause-effect relationship (4).
In our case, since there were no significant coronary lesions in none of the coronary arteries, we believe that the reported ICC may be the cause of the acute coronary syndrome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation 2007;115:1296-305. [PubMed]
- Oliveira MD, de Melo PH, Esteves Filho A, et al. Type 4 dual left anterior descending artery: a very rare coronary anomaly circulation. Case Rep Cardiol 2015;2015:580543.
- Oliveira MD, de Fazzio FR, Mariani Junior J, et al. Superdominant Right Coronary Artery with Absence of Left Circumflex and Anomalous Origin of the Left Anterior Descending Coronary from the Right Sinus: An Unheard Coronary Anomaly Circulation. Case Rep Cardiol 2015;2015:721536.
- Kim SH, Kim DH, Choi WG, et al. Intercoronary Communication between the Circumflex and Right Coronary Arteries Coexisted with Coronary Vasospasm. Korean Circ J 2013;43:488-90. [PubMed]
- Turker Y, Tibilli H. Congenital coronary artery fistula in an intercoronary communication between the left main and the diagonal branch of the left anterior descending coronary artery: an interesting case report. Rev Port Cardiol 2014;33:55.e1-4.
- Reig J, Jornet A, Petit M. Direct connection between the coronary arteries in the human heart. Intercoronary arterial continuity. Angiology 1995;46:235-42. [PubMed]
- Karmonik C, Partovi S, Rengier F, et al. Hemodynamic assessment of partial mechanical circulatory support: data derived from computed tomography angiographic images and computational fluid dynamics. Cardiovasc Diagn Ther 2015;5:160-5. [PubMed]
- Oliveira MD, Cavalcanti RR, Kajita AH, et al. Contrast injection in the RCA showing the retrograde filling of the LCx postero-lateral branch, with a bidirectional flow pattern. PA cranial incidence. Asvide 2015;3:025. Available online: http://www.asvide.com/articles/776
- Oliveira MD, Cavalcanti RR, Kajita AH, et al. Contrast injection in the RCA showing the retrograde filling of the LCx postero-lateral branch, with a bidirectional flow pattern. RAO incidence. Asvide 2016;3:026. Available online: http://www.asvide.com/articles/777
- Almeida C, Dourado R, Machado C, et al. Coronary artery anomalies. Rev Port Cardiol 2012;31:477-84. [PubMed]
- Vavuranakis M, Bush CA, Boudoulas H. Coronary artery fistulas in adults: incidence, angiographic characteristics, natural history. Cathet Cardiovasc Diagn 1995;35:116-20. [PubMed]
- Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn 1990;21:28-40. [PubMed]
- Atak R, Güray U, Akin Y. Images in cardiology: intercoronary communication between the circumflex and right coronary arteries: distinct from coronary collaterals. Heart 2002;88:29. [PubMed]
- Gavrielatos G, Letsas KP, Pappas LK, et al. Open ended circulation pattern: a rare case of a protective coronary artery variation and review of the literature. Int J Cardiol 2006;112:e63-5. [PubMed]


