Relationship of dental diseases with coronary artery diseases and diabetes in Bangladesh
Introduction
Coronary artery disease (CAD) is one of the major causes of morbidity and mortality worldwide, including low and middle income countries (1,2). In recent years, the prevalence of CAD increased rapidly in most of the developing countries, including Bangladesh (3). The World Health Organization projected that by the year 2020, CAD will be the leading cause of death in developing countries (3). Existing data suggest that epidemiological transition of rapid socioeconomic growth in developing countries and change in lifestyle is increasing the exposure to risk factors for CAD, such as diabetes, dyslipidaemia, genetic factors, hypertension, and smoking (3,4). However, many of these traditional risk factors do not explain the pathophysiological etiology of CAD. Recent evidence points out at the possible role of several infectious agents, such as dental infections in the pathogenesis of CAD (5,6).
Diabetes mellitus (DM) is a chronic condition that has become pandemic with increasing prevalence worldwide. Patients with DM often suffer from several oral and dental diseases, such as periodontal diseases, dental caries, and tooth loss in addition to the existing complications of the disease (7). The exact prevalence of periodontal diseases in Bangladesh is not known but estimated to be in the range of 18.5% to 42% (8). Evidence suggest a bidirectional relationship between DM and periodontal diseases (7). A recent study in Bangladesh reported that periodontal diseases can adversely affect the metabolic control of DM (9). The association between CAD, DM and oral health parameters has been explored in many studies in developed countries. However, data from developing countries are limited. We therefore conducted this study to assess the relationship between dental disease with CAD and DM in patients admitted at a tertiary hospital in Bangladesh.
Methods
Study design, population and site
A cross-sectional study was conducted among 216 consecutive patients admitted at the Bangladesh Institute of Research and Rehabilitation in Diabetes, Endocrine and Metabolic Disorder (BIRDEM) hospital between March and July 2011. The inclusion criteria were: both male and female patients aged between 18–70 years, admitted at BIRDEM hospital with CAD, DM or both. Those with serious complications, emergency admissions, or undergoing any surgical operative procedure were excluded.
Data collection
Data were collected by a team of two medical officers, two research nurses and a dentist experienced in hospital data collection, and trained by the investigators for five days in BIRDEM hospital. A pretested questionnaire was used for data collection through face-to-face interviews.
Variables and measurements
The questionnaire contained questions related to socio-demographic status, smoking habits, physical activity, daily consumption of vegetables, fruits, salt and oil. Physical activity was considered as recommended 150 minutes per week of vigorous activity. The daily recommended consumption of vegetables and fruits, salt and oil was defined as 400 grams or 5 serving, 5 grams or 1 teaspoon and 50 grams or 12 tea spoons, respectively according to WHO guidelines and recommendations. Blood pressure (BP) was measured using a mercury sphygmomanometer by the study physician in the wards when the patients was relaxed and repeated after ten minutes. The mean value of the two readings was considered. Weight and height was measured using standardized weight and height scale. Body mass index (BMI) was measured as weight in kilograms divided by height in centimeters squared. Blood samples for measurement of serum total cholesterol, triglyceride (TG), high density lipoprotein (HDL), low density lipoprotein (LDL), glycated hemoglobin (HbA1c), c-reactive protein (CRP), fibrinogen, serum creatine kinase MB (CK-MB), troponin, serum creatinine and serum glutamic-pyruvic transaminase (SGPT) were collected from the wards using aseptic techniques by the research nurse. All blood samples were analyzed in the BIRDEM laboratory using standard methods. Echocardiographic findings and results of the coronary angiogram (CAG) status of the patients were collected from patients’ medical records and interpreted by a cardiologist.
Dental examinations
All patients underwent a comprehensive dental examination performed by a single dentist with extensive clinical experience during the hospital stay and included evaluation of bleeding on probing, periodontitis, gum recession and decay and missing teeth (DMFT).
Data analysis
Data were presented as numbers (n) and percentages (%) with mean ± standard deviation (SD). Sample proportions were compared by chi-square tests with Yates’ correction and Fishers’ exact tests for categorical variables. Student’s t-test and Mann Whitney tests were performed for parametric and non-parametric continuous variables. Association of dental diseases with DM and CAD were analyzed using multivariate logistic regression models with adjusting for age, sex, and smoking. Odds ratios (OR) with 95% confidence interval (CI) were shown and a P value of <0.05 was considered as statistical significant.
Ethics
All participants in the study were informed about the objectives of the study and that participation was voluntary, and participants could leave the study at any time which will not affect the services they were receiving at the hospital. Confidentiality of the participants was maintained and data was restricted to the study investigators. All participants provided written informed consent before participating in the study. The study protocol was approved by the institutional review board of the Bangladesh Medical Research Council (BMRC).
Results
Socio-demography of the study participants
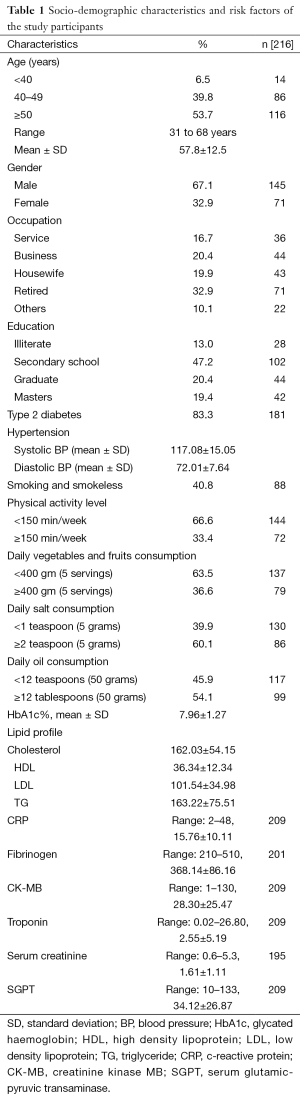
The mean age of the participants was 57.8±12.5 years and ranged from 31–68 years. Almost two-thirds of the participants (67.1%) were male. The main occupation of the participants was service (16.7%), business (20.4%), housewife (19.9%), retired (32.9%) and others (10.1%). More than half of the participants were illiterate or completed secondary education. The mean monthly income of the participants was 16,374±14,262 Bangladeshi Taka (Table 1).
Full table
Risk factors for DM and CAD
The mean BMI of the patients was 24.81±4.34. The mean waist circumference was 87.89±18.46 cm (range, 39–125 cm). The mean systolic and diastolic BP was 117.08±15.05 and 72.01±7.64 mmHg. Among the study participants 83.8% had type 2 DM.
The overall prevalence of tobacco use in any form was 40.8%. The proportion of current, recent, former and never smokers were 6.5%, 3.7%, 30.6% and 59.3% respectively. The duration of smoking was <20 years in 9.7% and equal and more than 20 years in 20.4% patients respectively. Two-third of the participants reported <150 min/week vigorous activity and 33.4% performed recommended physical activity. The proportion of patients taking recommended daily consumption of vegetables and fruits, salt and oil was 36.6%, 39.6% and 45.9%, respectively (Table 1).
Biochemical parameters
The mean total cholesterol was 162.03±54.15 mg/dL, HDL cholesterol 36.34±12.34 mg/dL, LDL cholesterol 101.54±34.98 mg/dL and TG was 163.22±75.51 mg/dL. The mean HbA1c was 7.96%±1.27%. The mean CRP was 15.76±10.11, fibrinogen 368.14±86.16, CK-MB 28.30±25.47 units/L, troponin 2.55±5.19, serum creatinine 1.61±1.11 and SGPT was 34.12±26.87 (Table 1). Biochemical analysis showed that 35.3% patients had fibrinogen (>400 mg/dL), 74.65 had CK-MB ≤24 units/L, 55.4% had troponin ≤0.2 ng/mL, 55.4 had serum creatinine >1.2 mg/dL, 21.1% had SGPT >40 U/L. The serum lipid profile analysis showed that 30.6% had cholesterol >200 mg/dL, 48.3% had LDL ≤100 mg/dL, 30.6% had HDL >40 mg/dL and 51.7% had TG >150 mg/dL.
Dental disease status
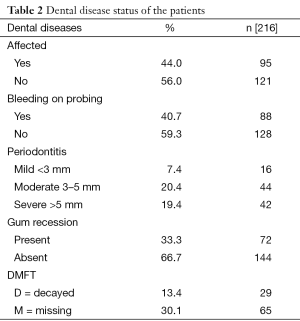
The overall proportion of patients with any dental disease was 44%, and 40.7% participant had bleeding on probing. In case of periodontitis, mild (<3 mm), moderate (3–5 mm) and severe (>5 mm) periodontitis were reported among 7.4%, 20.4% and 19.4% respectively. Almost one-third of the participants reported gum recession, 13.4% showed decaying and 30.4% had missing teeth (Table 2).
Full table
Echocardiography and coronary angiographic findings
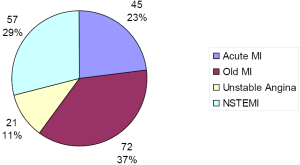
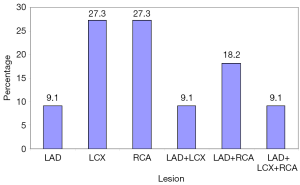
Echocardiography reports by 2D and M-mode showed that left ventricular ejection fraction (LVEF%) was [30–50] reduced in 51.5% patients. 29% patients were admitted with acute myocardial infarction (acute MI), 23% with old MI, 11% with unstable angina (UA) and 26.4% with non ST elevation MI (NSTEMI) respectively (Figure 1). The proportion of patients with left anterior descending artery (LAD) stenosis was 9.1%, left circumflex artery (LCX) stenosis 27.3% and right coronary artery stenosis was (RCA) 27.3% respectively. Combination of stenosis LAD + LCX was 9.1%, LAD + RCA was 18.2% and LAD + LCX + RCA was 9.1% (Figure 2).
Relationship of dental disease with DM and CAD
The mean ejection fraction in patients with DM and dental disease was 37.43±9.47 and DM without dental disease was 52.94±10.84 (P<0.001). Similarly, in patients with DM and dental disease the mean HbA1c was 9.69±1.92 and in those with DM and no dental disease HbA1C was 6.22±0.62 (P<0.001).
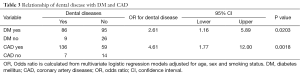
Multivariate logistic regression analyses indicates that patients with DM had 2.6 times higher odds of association with dental diseases compared to their counterparts (95% CI, 1.16–5.89, P=0.0203). Similarly, patients with CAD had 4.6 times higher odds of association with dental diseases compared to patients without CAD (95% CI, 1.77–12.01, P=0.0018) (Table 3).
Full table
Discussion
This is the first study in Bangladesh, to the best of our knowledge, comparing the relationship of dental diseases with angiographically detected CAD and confirmed cases of DM. Our study suggests a significant relationship of dental diseases with DM and CAD in Bangladeshi patients admitted at a tertiary hospital. The prevalence of dental diseases in our patients was 44% (95% CI, 37.4–50.6), which is higher than previous reports in Bangladesh (8). A recent study among patients with DM in urban Dhaka showed that the proportion of periodontitis was the highest (55.8%), followed by gingivitis 32.5%, periodontitis with endodontic lesion exactly 5% and necrotizing periodontal diseases 4.2% whereas periodontal abscesses showing the lowest was 2.5% (9). This study showed a significant association of periodontal diseases with age and reported that for each year increase of chronological age of the patients there was 0.20% increase of occurrence of periodontal diseases
A possible explanation for the reported association between dental diseases and CAD could be due to the role of bacterial products and inflammatory factors from dental infections that spreads into the blood stream and could have a role in atherosclerotic plaque formation, leading to development of CAD (10). However, such associations still need proof of concept. As diabetes is a costly condition affecting millions of people in Bangladesh (11), measures for its early prevention might contribute to preventing CVD mortality and morbidity.
In our study, DM patients with dental disease had significantly lower ejection fraction and higher HbA1c compared to their counterparts. A previous study also showed positive association between dental disease and worse glycemic control (12). The study reported that patients with type 2 DM were at higher risk of having severe forms of periodontal disease compared with non-diabetic subjects and highlighted the need for frequent supportive periodontal care for patients diagnosed with type 2 DM at the clinics (12). Previous studies in Bangladesh showed that patients with diabetes in Bangladesh, often present with uncontrolled diabetes, dyslipidaemia, depression, and low knowledge about their diabetes (13-16).
A study by Janket et al. compared the associations of dental score (ADS) with the traditional Framingham Heart Score in discrimination of CAD cases and controls (17). A predictive model including the ADS, CRP, HDL cholesterol and fibrinogen offered similar predictive value to the Framingham Heart Score and when the ADS were removed from the model, its predictive ability fell down, suggesting that the dental score contributed to CAD prediction on addition to known biochemical predictors. In this study, patients with CAD had approximately 4.6 times more chance for association with dental disease than those without CAD which is similar to a previous study (18). Our results are consistent with previous reports showing significant association between dental diseases and CAD after adjusting for common risk factors of age, sex and smoking (10).
In this study, periodontal conditions were moderate and severe in 20.4% and 19.4% of the patients respectively. Similar results were established in several other studies (19-21). Almost two-thirds of our participants reported less than recommended amounts of daily vegetables and fruits consumption, which is in line with previous reports in Bangladesh (13,22,23). A previous study showed that altered nutritional status, such as reduced intake of citrus fruit and vitamin C, might increases the risks of both inflammation and cardiovascular diseases (24,25).
The major strength of this study was the detection of dental disease, CAD and DM by trained dentists, use of angiographic reports and HbA1c. A limitation of this study was the cross-section design, which cannot conclude the causal association. In addition, this study was conducted at a tertiary hospital in Dhaka city among patients seeking healthcare and thus the results cannot be generalizable to the entire Bangladeshi population. Further multi-center longitudinal studies are needed measuring the markers of activated inflammation and hemostasis and determining the causal relationship of dental disease with DM and CAD.
Conclusions
Patients with DM and dental disease had lower left ventricular ejection fraction and poor glycemic control than their counterparts. Patients with DM and CAD have higher chances of developing dental diseases which might increase morbidity in these patients. Further studies to ascertain the causal relationship of dental disease with DM and CAD are essential in our population. Involving clinicians and dentists for management of DM and CAD patients might help to improve the management of these chronic conditions.
Acknowledgements
We would like to express our gratitude to all the staffs and patients involved in this study. We also acknowledge the support of different colleagues from BIRDEM hospital to support our works, especially Drs. Rownak Jahan Tamanna, Shahana Parveen, Saira Rahman, Md Rashedul Islam, Monjoya Banik, and Syeda Zerin Imam.
Funding: This study was funded by BMRC (Grant Number. BMRC/HNPSP-RP/2011/641).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med 2012;366:54-63. [Crossref] [PubMed]
- Islam SM, Purnat TD, Phuong NT, et al. Non-communicable diseases (NCDs) in developing countries: a symposium report. Global Health 2014;10:81. [Crossref] [PubMed]
- Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J 2004;148:7-15. [Crossref] [PubMed]
- Choudhury KN, Mainuddin AK, Wahiduzzaman M, et al. Serum lipid profile and its association with hypertension in Bangladesh. Vasc Health Risk Manag 2014;10:327-32. [PubMed]
- Emingil G, Buduneli E, Aliyev A, et al. Association between periodontal disease and acute myocardial infarction. J Periodontol 2000;71:1882-6. [Crossref] [PubMed]
- Bhateja S, Arora G. Cardiovascular Diseases and Periodontal diseases: Exploring the Connection: A Review. Journal of Cardiology and Therapy 2014;1:181-3. [Crossref] [PubMed]
- Campus G, Salem A, Uzzau S, et al. Diabetes and periodontal disease: a case-control study. J Periodontol 2005;76:418-25. [Crossref] [PubMed]
- Oates E, Dzintars K. Interaction between enfuvirtide, an injectable fusion inhibitor, and niacin in an HIV-infected patient. Ann Pharmacother 2010;44:2014-7. [Crossref] [PubMed]
- Mahmud SZ, Alif SM, Tarafder MA, Hossain SM. The Correlation between Periodontal Diseases and Chronological Age among Type 2 Diabetes Mellitus Patients attending at National Healthcare Network (NHN) Mirpur Centre, Dhaka, Bangladesh. Birdem Med J 2013;3:74-9.
- Zibaeenezhad MJ. Association between periodontal disease and coronary artery disease. Cent Eur J Med 2008;3:308-14.
- Shariful Islam SM, Lechner A, Ferrari U, et al. Social and economic impact of diabetics in Bangladesh: protocol for a case-control study. BMC Public Health 2013;13:1217. [Crossref] [PubMed]
- Al-Khabbaz AK. Type 2 diabetes mellitus and periodontal disease severity. Oral Health Prev Dent 2014;12:77-82. [PubMed]
- Islam SM, Mainuddin A, Islam MS, et al. Prevalence of risk factors for hypertension: A cross-sectional study in an urban area of Bangladesh. Glob Cardiol Sci Pract 2015;2015:43.
- Islam SM, Rawal LB, Niessen LW. Prevalence of depression and its associated factors in patients with type 2 diabetes: A cross-sectional study in Dhaka, Bangladesh. Asian J Psychiatr 2015;17:36-41. [Crossref] [PubMed]
- Islam SM, Ferrari U, Seissler J, et al. Association between depression and diabetes amongst adults in Bangladesh: a hospital based case-control study. J Glob Health 2015;5:020406. [Crossref] [PubMed]
- Islam SM, Niessen LW, Seissler J, et al. Diabetes knowledge and glycemic control among patients with type 2 diabetes in Bangladesh. Springerplus 2015;4:284. [Crossref] [PubMed]
- Janket SJ, Qvarnström M, Meurman JH, et al. Asymptotic dental score and prevalent coronary heart disease. Circulation 2004;109:1095-100. [Crossref] [PubMed]
- Mattila KJ, Nieminen MS, Valtonen VV, et al. Association between dental health and acute myocardial infarction. BMJ 1989;298:779-81. [Crossref] [PubMed]
- Humphrey LL, Fu R, Buckley DI, et al. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med 2008;23:2079-86. [Crossref] [PubMed]
- Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med 2004;15:403-13. [Crossref] [PubMed]
- Genco RJ, Trevisan M, Wu T, et al. Periodontal disease and risk of coronary heart disease. JAMA 2001;285:40-1. [Crossref] [PubMed]
- Islam SM, Alam DS, Wahiduzzaman M, et al. Clinical characteristics and complications of patients with type 2 diabetes attending an urban hospital in Bangladesh. Diabetes Metab Syndr 2015;9:7-13. [Crossref] [PubMed]
- Biswas T, Islam SM, Islam A. Prevention of hypertension in Bangladesh: a review. Cardiovasc J 2015;7:137-44. [Crossref] [PubMed]
- Lowe G, Woodward M, Rumley A, et al. Total tooth loss and prevalent cardiovascular disease in men and women: possible roles of citrus fruit consumption, vitamin C, and inflammatory and thrombotic variables. J Clin Epidemiol 2003;56:694-700. [Crossref] [PubMed]
- Karim MA, Majumder AA, Islam KQ, et al. Risk factors and in-hospital outcome of acute ST segment elevation myocardial infarction in young Bangladeshi adults. BMC Cardiovasc Disord 2015;15:73. [Crossref] [PubMed]