Utility of brain natriuretic peptide assay as a predictor of short term outcomes in patients presenting with syncope to the emergency department
Introduction
Syncope is a transient loss of consciousness with an inability to maintain postural tone that is followed by prompt and complete recovery (1). It affects 6 in 1,000 people yearly, accounting for 3% of emergency department (ED) visits and 1–6% of hospital medical admissions (1,2).
On average 30–40% of these patients are admitted to hospitals, resulting in nearly 200,000 hospital admissions annually in the United states with an approximate cost of 2.5 billion in year 2000 (1-3).
Current admissions practices result in marginal diagnostic and therapeutic benefit and consume healthcare resources. Recent emphasis has focused on risk stratifying syncope patients. There is a need to identify high risk patients requiring further investigation, and those with low risk who can be discharged safely. In recent years, a large number of risk stratification studies have been proposed including; the Syncope Evaluation in the Emergency Department Study (SEEDS), Osservatorio Epidemiologico Sulla Sincope nel Lazio (OESIL) (3,4), San Francisco Syncope Rule (SFSR) (5), Short term Prognosis of Syncope (STEP) (6), and the Risk Stratification of Syncope in the Emergency Department (ROSE) study (7,8). ROSE study was the first one to recommend the use of point of care BNP measurements, rectal examinations, and oxygen saturation in risk stratification of syncope patients and had an excellent sensitivity and negative predictive value that helped identifying high-risk patients and potentially reduced admission rates by 30% (7).
Brain (or B-type) natriuretic peptide (BNP) is secreted in response to an increase in ventricular volume and pressure load. BNP is a well-known prognostic marker in cardiovascular diseases such as heart failure and myocardial infarction (MI) (9). In addition recent studies have validated its potential utility at identifying higher risk individuals with other cardiac and non-cardiac disease states (10,11).
The aim of our study was to assess the use of BNP value to predict short term (one month) serious outcomes for patients presenting to ED with syncope. Our study attempted to determine if adding BNP to the standard evaluation of syncope in ED will help in risk stratification of patients and avoid unnecessary admissions without increasing adverse outcomes.
Methods
This prospective cohort study examined the use of BNP test as a predictor of short term serious outcomes in 159 patients who presented to ED with syncope between August 2012 and August 2013 in two tertiary teaching medical centers. Syncope was defined as a transient loss of consciousness with an inability to maintain postural tone that is followed by prompt and complete recovery. All patients were 18 years or older, eligible patients were identified in the ED triage and assessed for study inclusion by the attending physician. The goal of the study was explained to the patients, and written consent was obtained from all enrolled patients. This study received approval from ethics committee.
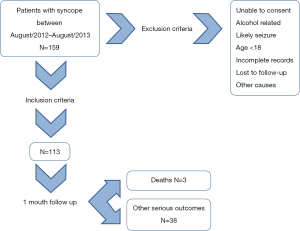
Exclusion criteria included patients under 18 years of age, patients who were unable to give consent, the presence of persistent neurological deficit suggestive of stroke, collapse related to alcohol consumption, hypoglycemia, trauma or seizure activity and clinician ordering BNP during evaluation. Of 159 patients, 113 were eligible for the study inclusion (Figure 1).
All patients underwent a standardized assessment including a full history and physical examination, lying and standing blood pressure measurement, 12 leads electrocardiogram (ECG), laboratory assessment, and review of current medications. BNP was measured using a whole blood immunoassay technique utilizing commercial assays. Treating physicians were blinded to the result of the BNP test and treatment decisions were not affected by the BNP value. Patients were admitted, referred for outpatient evaluation or discharged according to current ED protocols. Patient’s condition was followed; whether in hospital through the hospital electronic patient record system, or as out-patient by telephone calls 30 days after presentation to identify admissions, revisits to ED for the same complaint or serious clinical events that might have occurred outside the study site.
The primary endpoint was the combination of serious outcomes including all-cause mortality at 30 days after ED presentation. Serious outcomes were defined as death, acute MI, life threatening arrhythmia (ventricular fibrillation, sustained ventricular tachycardia, or asystole), a decision to implant a pacemaker/cardiac defibrillator within one month of collapse, stroke, and major bleeding requiring blood transfusion of >2 units or acute surgical or endoscopic intervention.
Interval data were tested for normality using the D’Agostino-Pearson normality test, which demonstrated significant deviations from normal distributions. Therefore, Mann-Whitney test was used throughout for group-wise comparisons of these data. Categorical variables were analyzed in 2×2 contingency tables using Fisher’s exact test to ascertain P values. Cut-offs were determined by receiver operator characteristic curve (ROC) analysis. All probabilities were 2-sided and P values <0.05 were considered statistically significant. Baseline characteristics required a (P<0.25) difference to be included in a logistic regression model to determine adjusted odds ratios (ORs) and 95% confidence intervals (95% CI). Only outcomes which were significant on a univariate basis were subjected to multivariate analysis. Calculations were made using Prism® v.6 software (GraphPad Corp, San Diego, CA, USA) and SPSS® v. 18 (IBM Corp. Armonk, NY, USA).
Results
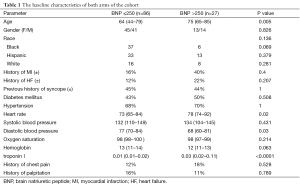
We included 113 patients presenting to ED with syncope to ED between August 2012 and August 2013. Patients were divided into two groups according to their serum BNP level with a cutoff value of 250; 86 patients were in the BNP ≤250 group and 27 patients were in the BNP >250 group. The baseline characteristics of both arms of the cohort are provided in Table 1. There was a statistically significantly differences between the two groups in age (75 vs. 64 years, P=0.05), diastolic blood pressure (P=0.03), heart rate (P=0.02) and troponin I (P<0.001). In addition, other characteristics met our criteria for evaluation as potential confounders (P≤0.25); these were congestive heart failure and hemoglobin concentration.
Full table
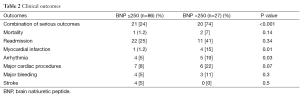
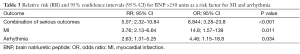
Out of the 113 patients, a total of 41 patients (36%) had serious outcomes within 30 days, 21 of them were in the low BNP group and 20 were in the high BNP group. When both groups were compared, the high BNP group has an 8.844 fold increase risk of serious outcomes (OR 8.844, 95% CI: 3.281 to 23.8, P<0.001), a 14.8 fold increase risk of MI (OR =14.8, 95% CI: 1.57 to 139, P=0.011), and a 4.46 fold increase risk life threatening arrhythmia (OR =4.46, 95% CI: 1.15–18.8, P=0.034). However, there was no statistically significant difference between the two groups in the combination of serious outcomes, one month mortality, major bleeding, major cardiac procedures or stroke as illustrated in Table 2. We evaluated the relative risk (RR) of both MI and life threatening arrhythmia as a function of BNP at > or ≤250 units. These are shown in Table 3, along with the ORs and 95% CI which were evaluated before and after adjustment for the confounding variables. Patients with BNP >250 has a 14.8 fold increase risk of MI (OR =14.8, 95% CI: 1.57 to 139, P=0.011), and a 4.46-fold increase risk life threatening arrhythmia (OR =4.46, 95% CI: 1.15 to 18.8, P=0.034). The ORs, adjusted for the confounding variables mentioned above are shown in Figure 2. For MI, the OR, after adjustment were reduced substantially; nevertheless, no confounding exposures obviated the independence of BNP level as a risk factor. In the case of arrhythmia, however, BNP as a risk factor appears to be dependent upon history of previous MI (OR =3.65; 95% CI: 0.97 to 13.7).
Full table
Full table
Comparison between ROSE rule and San Francisco rule in predicting outcomes
San Francisco Syncope Rule and ROSE Rule scores were calculated for every patient by the study team. However, the results were not available for the treating physicians.
Out of the 113 patients included in the study, 50 patients (44%) were considered high risk by ROSE rule compared to 59 patients (52%) identified as high risk by San Francisco rule. There was a significant association between Rose rule’s high risk patients and poor outcomes compared to San Francisco rule which didn’t show significant association (OR: 2.82; CI: 1.29 to 6.18; P<0.01), (OR: 1.24; CI: 0.58 to 2.66; P<0.69), respectively.
Discussion
Syncope represents a difficult diagnostic dilemma for physicians. A survey of North American physicians revealed that the disposition of patients with syncope was the second most common decision problem (12). The direct cost of diagnosing and treating syncope is substantial. The estimated total annual cost for syncope related admissions were $2.5 billion in year 2000 (1).
Delineating the underlying causes of syncope and the risk of adverse outcome can be challenging. Most syncope causes are benign, but occasionally, it can be associated with significant morbidity and mortality. Some patients require emergent hospitalization for workup and treatment of life-threatening or potentially life-threatening causes; others need close outpatient follow-up and evaluation, whereas some patients need no further evaluation like patients with neurally mediated or orthostatic syncope (13).
For syncope patients in whom the etiology remains unclear after the initial ED or ambulatory clinic evaluation, the need for hospitalization is less well defined and consequently so-called “risk stratification” methods have been advocated. EDs commonly advocate the use of screening protocols based on current practice guidelines in an attempt to ensure early identification of all high-risk patients. However, some of the previously used protocols were extensive, complicated, and nonspecific, and didn’t gain widespread acceptance and were rarely applied in general practice. Ideally, screening protocols should be simple and reproducible, identify all patients with high risk features, and separate those patients who would benefit from further workup and possible hospital admission from those who are low-risk and do not necessitate further resource utilization, testing, and unnecessary medical expenditure. Both the San Francisco Syncope Rule and the ROSE rule have been proposed as reliable risk stratification criteria for patients presenting to the ED with syncope with no obvious precipitating cause. The highly sensitive San Francisco Syncope Rule was derived by assessing the accuracy and reliability of 50 predictor variables used in the evaluation of patients with syncope in a multiphase prospective cohort study (5,14). It has helped in augmenting physician judgment and allowing physicians to rationally decide which patients with syncope need admission based on their short-term risk. The rule is easily remembered by the mnemonic: CHESS (history of Congestive heart failure, Hematocrit <30%, abnormal ECG, Shortness of breath and, initial Systolic blood pressure <90 mmHg). It emphasizes most of the key risk factors that have been studied and identified in several retrospective studies and current practice guidelines. However, it does not include the use of more recent biomarkers such as BNP. Addition of these types of biomarkers may add important prognostic information, help improve risk stratification of patients, and identify patients who may need hospital admission (15).
BNP is a well-known prognostic marker in cardiovascular diseases such as heart failure and MI (9,16). In addition recent studies have validated its potential utility in identifying higher risk individuals with other cardiac and non-cardiac diseases (10,11). Because many of the major prognostic factors in syncope are related to cardiac disease, the role of biomarkers such as BNP in risk stratification of patients with syncope was studied previously (17). Reed et al. developed the ROSE Rule in an attempt to incorporate the use of BNP in risk stratification of syncope patients presenting to the ED (7,8). The ROSE rule consists of seven variables easily remembered by the mnemonic “BBRACES”: (BNP >300 pg/mL, Bradycardia <50 BPM, Rectal examination showing FOBT +ve, Anemia with Hemoglobin <9, Chest pain, EKG showing Q waves and Oxygen Saturation <94%). ROSE study was the first study to recommend the use of point of care BNP measurements, rectal examinations, and oxygen saturation in risk stratification of syncope patients. It also had an excellent sensitivity and negative predictive value that helped identify high-risk patients and potentially reduced admission rates by 30% (7,18).
Our study attempted to determine if adding BNP to the standard evaluation of syncope in ED will help in risk stratification of patients and avoid unnecessary admissions without increasing adverse outcomes. The primary endpoint was the combination of serious outcome including all-cause mortality at one month after ED presentation. Our study results showed that syncope patients with elevated BNP (>250) on presentation had worse outcomes. Specifically, they had higher incidence of both MI and life threatening arrhythmia within one month after ED presentation. These results show that incorporation of the ROSE rule and BNP assay can help refine syncope assessment protocols and improve patient outcomes.
The main limitation of our study is the non-randomized and observational design. Our study included a small number of patients which may have led to selection bias. Also, a possible limitation to the use of BNP for syncope risk stratification is that it might identify patients who are older or who have structural heart disease. A large multicenter prospective study is needed to establish the utility of BNP as a true prognostic factor in patients with syncope.
Conclusions
Our study results further validates the ROSE rule and the utility of BNP in risk stratification of syncope patients. This study showed that measuring BNP and adding ROSE rule to the standard evaluation of syncope can sufficiently predict short term serious outcomes for patients presenting to ED with syncope. In addition, it will help identify high-risk patients and possibly prevent unnecessary admissions without increasing adverse outcomes. Larger randomized trials are needed to further explore the utility of biomarkers in the evaluation of syncope.
Acknowledgements
Authors are gratefully acknowledge the help of Dr. Habib Habib and Dr. Anish Samuel in data collection.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sun BC, Mangione CM, Merchant G, et al. External validation of the San Francisco Syncope Rule. Ann Emerg Med 2007;49:420-7, 427.e1-4.
- Sun BC, Emond JA, Camargo CA Jr. Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol 2005;95:668-71. [Crossref] [PubMed]
- Colivicchi F, Ammirati F, Melina D, et al. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J 2003;24:811-9. [Crossref] [PubMed]
- Birnbaum A, Esses D, Bijur P, et al. Failure to validate the San Francisco Syncope Rule in an independent emergency department population. Ann Emerg Med 2008;52:151-9. [Crossref] [PubMed]
- Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med 2004;43:224-32. [Crossref] [PubMed]
- Costantino G, Perego F, Dipaola F, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission: results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol 2008;51:276-83. [Crossref] [PubMed]
- Reed MJ, Newby DE, Coull AJ, et al. The ROSE (risk stratification of syncope in the emergency department) study. J Am Coll Cardiol 2010;55:713-21. [Crossref] [PubMed]
- Reed MJ, Newby DE, Coull AJ, et al. Role of brain natriuretic peptide (BNP) in risk stratification of adult syncope. Emerg Med J 2007;24:769-73. [Crossref] [PubMed]
- Doust JA, Glasziou PP, Pietrzak E, et al. A systematic review of the diagnostic accuracy of natriuretic peptides for heart failure. Arch Intern Med 2004;164:1978-84. [Crossref] [PubMed]
- Tanimoto K, Yukiiri K, Mizushige K, et al. Usefulness of brain natriuretic peptide as a marker for separating cardiac and noncardiac causes of syncope. Am J Cardiol 2004;93:228-30. [Crossref] [PubMed]
- Doust JA, Pietrzak E, Dobson A, et al. How well does B-type natriuretic peptide predict death and cardiac events in patients with heart failure: systematic review. BMJ 2005;330:625. [Crossref] [PubMed]
- Graham I, Stiell I, McAuley L, et al. Potential areas for new clinicaldecision rules: comparison of North America and Europe Annu Meet Int Soc Technol Assess Health Care 1999;15:126. [abstract].
- Reed MJ, Gray A. Collapse query cause: the management of adult syncope in the emergency department. Emerg Med J 2006;23:589-94. [Crossref] [PubMed]
- Quinn JV, Stiell IG, McDermott DA, et al. The San Francisco Syncope Rule vs physician judgment and decision making. Am J Emerg Med 2005;23:782-6. [Crossref] [PubMed]
- Elesber AA, Decker WW, Smars PA, et al. Impact of the application of the American College of Emergency Physicians recommendations for the admission of patients with syncope on a retrospectively studied population presenting to the emergency department. Am Heart J 2005;149:826-31. [Crossref] [PubMed]
- Gopinathannair R, Mazur A, Olshansky B. Syncope in congestive heart failure. Cardiol J 2008;15:303-12. [PubMed]
- Reed MJ, Newby DE, Coull AJ, et al. Role of brain natriuretic peptide (BNP) in risk stratification of adult syncope. Emerg Med J 2007;24:769-73. [Crossref] [PubMed]
- Williamson C, Reed MJ. Syncope: the emergency department and beyond. Intern Emerg Med 2015;10:843-50. [Crossref] [PubMed]